Prostate
The prostate is a conical, fibro-muscular-glandular organ that surrounds the proximal part of the male urethra. Its female homolog is paraurethral glands (of Skene).
The prostate is located in the lesser pelvis below the neck of the urinary bladder and above the urogenital diaphragm.
Function of Prostate:
The prostate secretes acid phosphatase, fibrinolysin, citric acid, amylase, prostate-specific antigen (PSA) & prostaglandins. Its secretions form the bulk of the seminal fluid (semen).
Coverings of Prostate:
1. True capsule: It is formed by the condensation of the peripheral fibrous stroma of the gland.
2. Fale Capsule: It is derived from the visceral layer of pelvic fascia. It is outside the true capsule & envelops the prostate & urinary bladder in the same compartment.
Presenting Part:
Apex: It is directed downward & rests on the superior surface of the urogenital diaphragm.
Base: It is directed upward & surrounds the neck of the urinary bladder.
Anterior Surface: It is situated 2 cm behind the pubis symphysis & separated from symphysis by the retropubic space (of Retzius).
Posterior Surface: It is broad and flat and lies in front of the ampulla of the rectum.
Two inferolateral surfaces: These are related to the anterior fibers of the levator ani.
Anatomical Lobes:
The posterior surface is divided into small upper & larger lower areas by a transverse sulcus. The upper area represents the median lobe and the lower area is divided by a median sulcus into two lateral lobes.
Surgical Lobes:
- Anterior lobe
- Posterior lobe
- Median lobe
- Two lateral lobes.
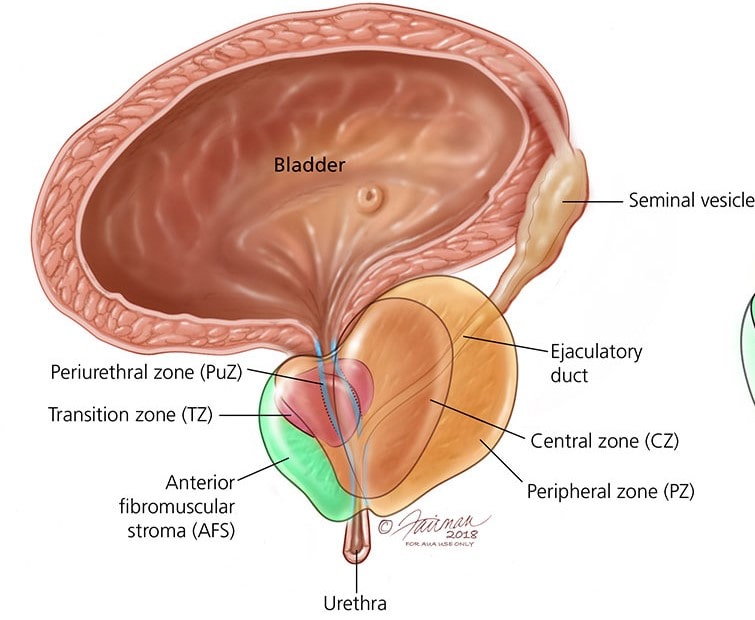
Zones of Prostate:
From outside to inwards-
| Peripheral Zone (70%): Prostatic carcinoma mainly arises from the peripheral zone. |
| Central Zone (25%): The central zone is rarely involved in any diseases. |
| Transitional Zones (5%): Benign prostatic hypertrophy (BPH) affects the transitional zone. |
Structure within the Prostate:
- Prostatic urethra
- Ejaculatory ducts
- Prostatic utricle
Structure of Prostate:
The prostate gland is made up of fibrous tissue (1/4), muscular tissue (1/4), and glandular tissue (1/2).
| Fibrous Tissue: It is thickened at the periphery to form the true capsule of the prostate gland. |
| Muscular Tissue: It consists of smooth muscles & is continuous with the detrusor muscle of the urinary bladder. |
| Glandular Tissue: It consists of tubuloalveolar glands arranged in three concentric groups (mucosal, submucosal, and main); all of them open into the urethra. |
Artery Supply of Prostate:
The prostate gland is supplied by the branches of the inferior vesical, middle rectal, and internal pudendal arteries.
Venous Drainage of Prostate:
The veins form the prostatic venous plexus around the sides & base of the gland & occupy the space between true & false capsules. It receives the deep dorsal vein of the penis in front & is continuous above with vesical venous plexus.
Nerve Supply:
| Sympathetic: By superior hypogastric plexus. The preganglionic sympathetic fibers arise from L1-L2 spinal segments. |
| Parasympathetic: By pelvic splanchnic nerves which convey preganglionic fibers from S2-S4 spinal segments. |
Development of Prostate:
Parenchyma: It develops in the third month of intrauterine life (IUL) as a series of endodermal buds (outgrowths) from the lining of primitive urethra & an adjoining portion of the urogenital sinus.
Stroma: It develops in the 4th month of IUL from surrounding mesenchyme derived from the splanchnic layer of mesoderm.
Benign Prostatic Hypertrophy (BPH):
After 50 years of age, the prostate is enlarged due to hypertrophy forming an adenoma. The BPH commonly involves the median lobe.
Clinically BPH presents as :
- Increased frequency of urination,
- Urgency of urination,
- Difficulty in starting & stopping urination,
- A sense of incomplete emptying of the urinary bladder.
The surgical removal of adenoma is called a prostatectomy.
Prostatic Carcinoma:
It usually occurs after the age of 50 years. The carcinoma is commonly found in the outer (peripheral) zone which usually involves the posterior lobe.
Clinically, it presents as :
- Pain in the perineum.
- Urinary obstruction.
- Difficulty in urination.
Also read: Anatomy Question Collection
Also read: Anatomy Questions & Answers
Also read: Anatomy notes

Comments (0)