URINARY BLADDER & Urethra
Q.1 What are the variations in the shape of the urinary bladder?
- When empty, tetrahedral and lies within pelvis
- When fills, ovoid and extends into the abdominal cavity. The maximum capacity of the urinary bladder is about 500 ml.
Q.2 What are the variations in the position of the bladder with age?
In infants, at a higher level, the internal urethral orifice lies at the level of the superior border of the symphysis pubis. Then orifice descends rapidly for the first three years, then slowly from 4 to 9 years, then it again descends to the adult position after puberty.
Q.3 What are the peritoneal folds of urinary bladder?
- Median umbilical fold
- Median umbilical ligament (fold):
Connect superior vesical arteries to umbilicus - Lateral false ligament:
Connect the superior surface of the bladder to the lateral wall of the pelvis - Posterior false ligament:
Connect the lateral margin of the base of the bladder to the rectum.
Q.4 Name the ligaments formed by the pelvic fascia around urinary bladder?
- Lateral true ligament:
Formed from fascia covering obturator internus - Medial puboprostatic ligament
- Lateral puboprostatic ligament.
In females, bands similar to puboprostatic ligaments are known as pubovesical ligaments. Formed from the fascia over the upper surface of the levator ani. - Median umbilical ligament:
Remnant of urachus.
Connects the apex of the urinary bladder to the umbilicus. - Posterior ligament:
Connects base of bladder to lateral pelvic wall.
Q.5 What are the relations of the base of urinary bladder?
In males:
- Upper part: Rectovesical pouch containing intestine.
- Lower part: Seminal vesicles, Terminations of vasa deferentia.
In females:
- Cervix
- Vagina
Q.6 What are the characteristic features of the trigone of the bladder?
- Mucosa is firmly attached to the muscular coat.
- Has an internal urethral orifice, at anteroinferior angle, and two ureteric openings, at postero-lateral angles.
- Uvula vesicae is a slight elevation just posterior to the urethral orifice.
- Interureteric ridge forms the base of trigone, which are the continuations of the longitudinal muscle coat of two ureters.
Q.7 What are the boundaries of paravesical fossa?
Laterally, it is bound by ductus deferens in male and the round ligament of the uterus in females.
Q.8 What is the arterial supply of urinary bladder?
- Superior and inferior vesical arteries, branches of the anterior trunk of the internal iliac artery.
- Obturator and inferior gluteal arteries.
- In females, also the uterine artery and vaginal artery in place of inferior vesical artery
Q.9 What is the nerve supply of urinary bladder?
- Parasympathetic efferent fibers (nerve originates S2,3,4):
Motor to detrusor muscle and inhibitory to sphincter vesicae. - Sympathetic efferent fibers (T10 to L2):
Inhibitory to detrusor and motor to sphincter vesicae. - Somatic pudendal nerve (S2,3,4):
Supplies sphincter urethrae. - Sensory nerve:
Both parasympathetic and sympathetic nerves. They carry the sensation of pain and distension.
Q.10 What is fascia of Denonvilliers?
It is rectovesical fascia in males, separating rectum and triangular area between two ductus deferens at base of bladder.
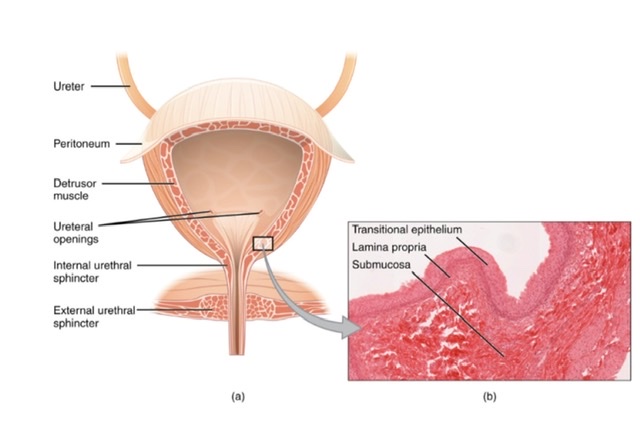
Q.11 What is the histological structure of urinary bladder?
Made up of three coats:
- Serous coat: Outer.
- Muscular coat: Forms detrusor muscle, consists of three layers of smooth muscle fibers, an external and internal longitudinal and a middle circular.
- Mucosa: Epithelium is of transitional variety. Submucosa and glands are absent.
Q.12 Why it is possible to drain a distended bladder through the anterior abdominal wall without injuring the peritoneum?
In adults, the bladder is a pelvic organ. When it distends, its upper part cornea in contact with anterior abdominal wall above the pubic symphysis. As bladder ascends, the fold of peritoneum passing from the anterior abdominal wall to the superior surface of the bladder also rises so no peritoneum intervenes between the distended bladder and anterior abdominal wall. So it can be relieved by a needle just above the pubic symphysis.
Q.13 How urinary bladder is developed?
- Epithelium of urinary bladder:
Endodermal, cranial part of vesico-urethral canal. - Epithelium of trigone:
Mesodermal, absorbed mesonephric ducts. - Muscular and serous coat:
Splanchnopleuric mesoderm.
Q.14 What are common congenital anomalies of urinary bladder?
- Bladder may be duplicated.
- Sphincter vesicae may be absent.
- Hourglass bladder:
Divided into two compartments by a constriction in the middle of the organ. - Communication with rectum or vagina may exist.
- Congenital diverticula may be present.
Q.15 What is ectopia vesicae?
A congenital defect in which the lower part of the anterior abdominal wall and anterior wall of the bladder does not develop. The cavity of the bladder may be exposed on the surface of the body. Usually associated with epispadias (urethra opens on the dorsal aspect of the penis).
Q.16 What does the urachus presents?
The fibrous allantois, which extends from apex of bladder to umbilicus.
Q.17 What are Lacunae of Luschka?
These are small cavities that may remain in urachus. One of these may enlarge to form a cyst.
URETHRA
Q.1 What is the length of urethra?
In males: 18-20 cm
In females: 4 cm long
Q.2 What are the parts of the urethra in males?
- Prostatic part: 3 cm.
- Membranous part: 1.5 to 2 cm.
Passes through the urogenital diaphragm. - Spongy (penile) part: 15 cm
Q.3 What are the features of the floor of the prostatic part?
- Urethral crest (veru montanum):
Median longitudinal ridge on the posterior wall. - Colliculus seminalis:
Elevation in the middle part of the crest.
In midline has opening of blind sac, prostatic utricle.
On either side of the crest has the opening of left and right ejaculatory ducts. - Prostatic sinuses:
On each side of the crest, has the opening of prostatic ducts.
Q.4 Which is the narrowest part of urethra?
The narrowest part of the male urethra is an external orifice, otherwise, the membranous urethra is the narrowest part.
Q.5 What is the position of the Bulbourethral gland?
These are placed one on each side of the membranous urethra. Their ducts open into the penile urethra.
Q.6 What are the variations in the shape of the lumen of male urethra?
- Prostatic part: Semilunar .
- Membranous part: Star-shaped.
- Spongy part: Transverse, except external urethral orifice which is vertical slit.
Q.7 What are the characteristic features of sphincters of urethra?
- Internal urethral sphincter (Sphincter vesicae) :
– Involuntary.
– Supplied by sympathetic nerve.
– Made up of smooth muscle fibers with elastic and collagenous fibers.
- External urethral sphincter (Sphincter urethrae)
– Voluntary
– Supplied by pudendal nerve.
– Made up of striated muscle fibers.
Q.8 What is the lymphatic drainage of urethra?
Membranous and prostatic part drains into internal iliac lymph nodes. Penile part drains into superficial inguinal nodes.
Q.9 What are Home’s tubules?
These are glandular invaginations of transitional epithelium on each side of internal urethral orifice near the bladder neck in females.
Q.10 Which part of the male urethra is ruptured during instrumentation?
Membranous part because it is narrowest and least dilatable.
Q.11 What is the commonest cause of urethral stricture?
Gonococcal infection
Q.12 Why the instruments in urethra should be introduced with beak downwards?
Because immediately within external meatus, urethra dilates into a terminal fossa, whose roof bears a mucosal fold (Lacuna Magna) which may catch the tip of the catheter.
Q.13 How the urethra is developed?
Female urethra:
Caudal part of vesicourethral canal.
Male urethra:
- From urinary bladder up to opening of ejaculatory ducts:
Endodermal (caudal part of vesico-urethral canal) - Rest of prostatic urethra and membranous urethra:
Pelvic part of definitive urogenital sinus - Penile part except terminal part:
Epithelium of phallic part of definitive urogenital sinus - Terminal part of penile urethra:
From ectoderm
Q.14 What is hypospadias?
Due to the inability of urethral folds to unite anteriorly, the urethra opens on the undersurface of the penis.
Q.15 What is epispadias?
The urethral orifice opens on the dorsal aspect of the penis.

Comments (0)