Rectum & Anal Canal (Viva)
RECTUM
Q.1 What is the length of the rectum?
12 cm
Q.2 What is the situation and extent of the rectum?
Situation:
In the posterior part of the lesser pelvis, in front of lower three pieces of sacrum and coccyx.
Extent:
From S3 vertebra (Rectosigmoid junction) to 2-3 cm, in front and a little below the tip of coccyx (Anorectal junction).
Q.3 What are the curves of the rectum and what is their position?
Rectum lies in the median but shows two types of curvatures:
- Anteroposterior curves:
– Sacral flexure of rectum follows the concavity of sacrum and coccyx.
– Perineal flexure of the rectum is backward bent at the anorectal junction.
- Lateral curves
– Upper lateral curve is convex to right.
– Middle lateral curve is convex to left.
– Lower lateral curve is convex to right.
Q.4 What is rectal ampulla?
The lower dilated part of the rectum is called rectal ampulla.
Q.5 What are the peritoneal relations of rectum?
- Upper 1/3: Covered with peritoneum in front and at sides.
- Middle 1/3: Covered only in front.
- Lower 1/3: Devoid of peritoneum.
Q.6 What are the different types of folds of the mucous membrane of the rectum?
- Longitudinal folds: Present in the lower part of the rectum and they are obliterated by distension.
- Transverse folds (Houston’s valves): Are permanent and most marked when the rectum is distended.
These are formed by infoldings of mucous membrane containing circular and longitudinal muscle coat. - Upper fold: From right or left wall, near the upper end of the rectum.
- Middle fold: From anterior and right walls, at the rectal ampulla.
- Lowest fold: 2.5 cm below middle fold and projects from the left wall.
- Sometimes fourth fold is present 2.5 cm above the middle fold.
Q.7 What are the relations of the rectum?
Anteriorly:
- Lower part of sacrum
- Coccyx
- Piriformis muscle: Left and right
- Coccygeus muscle: Left and right
- Levator ani muscle: Left and right
- Sympathetic trauma
- Median sacral artery
- Lateral sacral artery
- Medial sacral artery
- Pudendal nerve
- Ganglion impar.
Posteriorly:
In male:
To urinary bladder, seminal vesicles, ductus deferens lower ends of ureters and prostate.
In female:
To vagina and lower part of the uterus.
In both sexes:
Sigmoid colon, Ileum
Laterally:
Coccygeus muscle (Left and right),
Levator ani muscle (Left and right),
Ileum
Q.8 What are the boundaries of the pararectal fossa?
It is bound laterally in males by sacrogenital fold and in females by rectouterine fold.
Q.9 What is the blood supply of the rectum?
- Anterior supply:
– Superior rectal artery: Continuation of the inferior mesenteric artery.
– Middle rectal arteries: Arise from anterior division of internal iliac artery.
– Median sacral artery: Arise from aorta.
- Venous drainage:
– Superior rectal veins: Continues upward as an inferior mesenteric vein.
– Middle rectal veins: Drain into internal iliac veins.
Q.10 What is the lymphatic drainage of the rectum?
- From upper half: To inferior mesenteric nodes through pararectal and sigmoid nodes.
- From the lower half: To internal iliac nodes.
Q.11 What are the supports of the rectum?
- Pelvic floor.
- Fascia of Waldeyer: Suspends lower part of rectal ampulla to sacrum.
- Lateral ligaments of rectum: Condensation of pelvic fascia.
- Rectovesical fascia: Extends from rectum to seminal vesicles and prostate in front.
- Pelvic peritoneum and related vascular pedicles.
Q.12 What structures are palpated on per rectum (PR) examination?
In a normal patient:
- In males:
Anteriorly (from below upwards):
• Bulb of penis and membraneous urethra,
• prostate,
• seminal vesicles, and
• base of the urinary bladder.
- Female:
Anteriorly,
• Vagina and uterus.
- In both sexes:
Posteriorly:
• Coccyx and lower part of the sacrum.
Laterally:
• Ischial spine and ischial tuberosity,
• Ischiorectal fossa.
Abnormalities which can be detected include:
- Within lumen:
Fecal impaction, foreign body. - In the wall:
Rectal growths, strictures but not hemorrhoids unless thrombosed. - Outside rectal wall:
Pelvic bony tumors, collections of fluid or tumors in a pouch of Douglas and rectovesical pouch, abnormalities of prostate and seminal vesicles; distended bladder, pelvic appendix, ureters, uterine tubes and ovary.
Q.13 How rectum is developed?
From primitive rectum, i.e. dorsal subdivision of cloaca.
ANAL CANAL
Q.1 What is the position of the anal canal?
Anal canal is situated in perineum between two ischiorectal fossae.
Q.2 What is the extent of the anal canal?
Extends from anorectal junction which lies 2-3 cm in front and slightly below the tip of coccyx to anus, about 4 cm below and in front of the tip of the coccyx in the cleft between two buttocks.
Q.3 What are the relations of the anal canal?
- Anteriorly: Perineal body
In males: Membranous urethra, Bulb of penis
In females: Lower end of the vagina - Posteriorly: Anococcygeal ligament Tip of coccyx.
- Laterally: Ischiorectal fossa.
- All around: Sphincter muscles.
Q.4 What are the divisions of the anal canal? What are the characteristic features of each part?
- Upper part:
• 15 mm long, up to the pectinate line.
• Lined by columnar epithelium.
• Mucous membrane shows: 6-10 longitudinal folds.
– Anal columns: Vertical mucosal folds
– Anal valves: Small crescentic folds connecting lower ends of adjoining anal columns.
– Anal sinuses: Small pockets above anal valves.
– Pectinate line: Circular line of attachment of anal valves.
- Middle part:
• 15 mm long
• Between pectinate line and white line of Hilton’s.
• Stratified squamous epithelium lining
• No sweat or sebaceous glands or hair.
• Anal columns are not present
• Submucosa have dense connective tissue.
- Lower part:
• 8 mm long
• Lined by true skin
• Has sweat and sebaceous glands.
Q.5 What is the distribution of anal glands?
Anal glands are present in the submucosa and they open above each anal valve into anal sinus. Opening of glands on anal mucosa is referred to as anal crypts.
Q.6 What is the position of Hilton’s line?
At the level of an interval between the subcutaneous part of the external anal sphincter and lower border of the internal anal sphincter. Felt as groove on digital examination.
Q.7 What are the parts of the external anal sphincter?
Made of striated muscle.
Three parts:
- Deep part:
• Surrounds the upper part of internal anal sphincter i.e., above the pectinate line and is fused with puborectalis.
• Arise from anococcygeal ligament.
• Inserted into the perineal body where fibers decussate.
- Superficial part:
• Elliptical in shape.
• Arise from the terminal part of coccyx.
• Fibers surround internal sphincter in the lower part between the pectinate part and white line of Hilton and are inserted into the perineal body.
- Subcutaneous part:
• Below internal sphincter.
• No bony attachment.
• Surrounds the lower part of the anal canal.
Q.8 What are the features of the internal sphincter?
• Involuntary.
• Formed by thickened circular muscle coat.
• Surrounds upper ¾ of the anal canal, above the subcutaneous part up to the white line of Hilton.
• Deep to external sphincter.
Q.9 How the conjoint longitudinal coat is formed?
It is formed by fusion of puborectalis with a longitudinal muscle coat of rectum at the anorectal junction.
It lies between external and internal sphincters.
Divides into fibroelastic septa, which are attached to the skin around anus and submucosa below anal valves (Corrugator cutis ani).
Q.10 What is ‘anorectal ring’?
It is a muscular ring at the anorectal junction formed by the fusion of puborectalis, deep external and internal sphincter.
Q.11 Name surgical spaces in and around the anal canal.
- Ischiorectal fossa: On each side.
- Perianal space: Around the anal canal below the white line.
- Submucous space: Above the white line, between the mucous membrane and internal sphincter.
Q.12 What is the blood supply of the anal canal?
- Arterial supply:
– Superior rectal artery (continuity of inferior mesenteric artery):
Above the pectinate line
– Inferior rectal artery, branch of internal pudendal artery:
Below the pectinate line
– Median sacral artery:
To posterior part of the anorectal junction and anal canal.
- Venous drainage:
– Internal rectal venous plexus:
In submucosa. It drains into a superior rectal vein.
It communicates with external rectal plexus.
– External rectal venous plexus:
Outside muscular coat.
Drained by inferior and middle rectal vein.
– Anal veins:
Arranged radially around the anal margin.
Q.13 What is the characteristic of venous drainage of the anal canal?
Superior rectal vein is a tributary of the portal system, middle and inferior rectal veins drain into systemic veins. These veins anastomose with each other.
Blood from the portal system can pass into systemic circulation through these anastomoses if the portal venous pressure rises leading to their dilatation.
Q.14 What is the lymphatic drainage of the anal canal?
The upper part of the anal canal drains into internal iliac nodes and lower part into superficial inguinal nodes.
Q.15 What is the developmental origin of the anal canal?
It develops partly from ectoderm (Proctoderm) and partly from endoderm (dorsal division of cloaca). The junction is indicated by the pectinate line (anal valves).
Q.16 What is the nerve supply of the anal canal?
- Above the pectinate line:
Inferior hypogastric plexus (Sympathetic).
Pelvic splanchnic (Parasympathetic). - Below pectinate line:
Inferior rectal (Somatic). - Sphincters:
Internal sphincter:
• Sympathetic and parasympathetic.
External sphincter:
• Inferior rectal and perineal branch of the fourth sacral nerve.
Q.17 What is the cause of Imperforate anus?
Failure of the anal membrane to break at the pectinate line at the end of eight weeks of intrauterine life.
Q.18 What are the other congenital anomalies of the anal canal?
- Anal stenosis.
- Anal agenesis.
- Anorectal agenesis.
Q.19 What is the cause of rectal incontinence?
- Damage to anorectal ring.
- Damage of the nerves supplying the muscles of the anorectal ring.
Q.20 What is anal fissure?
Rupture of one of anal valves, usually by passage of dry hard stool. May be painful, if skin is also involved.
Q.21 What is fistula in ano?
It is an abnormal epithelialized track connecting the anal canal with the exterior.
Caused by an abscess around the anus.
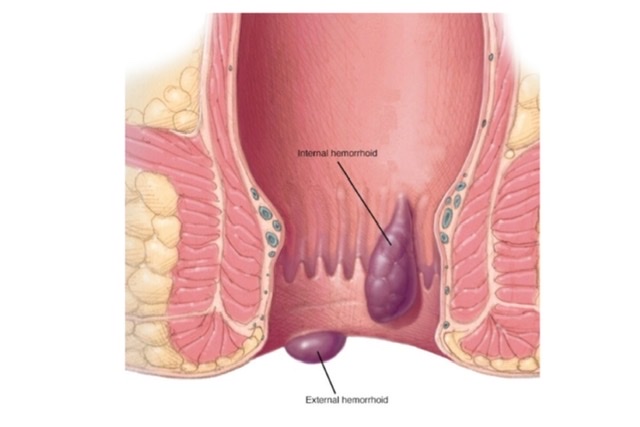
Q.22 What are hemorrhoids (Piles)?
These are the dilatations of rectal venous plexus.
They are of two types:
- External hemorrhoids are the dilated anal veins around the anal margin. These occur below the pectinate line and are very painful.
- Internal hemorrhoids are the dilated internal rectal venous plexus. These occur above the pectinate line.
Two types:
- Primary piles: Occur at 3, 7, and 11 o’clock position, representing three main radicles of superior rectal vein in the anal columns.
- Secondary piles: These are dilatations in other positions of the lumen.
Q.23 How the piles are caused?
The following factors are thought to play a role in the causation of piles.
- Hereditary:
Frequently associated with varicose veins. - Anatomical causes:
Collecting radicles of the superior rectal vein lie unsupported in the very loose submucous connective tissue of the rectum These veins pass through muscular tissues and are liable to be constricted by its contraction during defaecation. This increases pressure within them. - Morphological causes:
Valves are absent in the portal system. Hence, the whole brunt of the pressure of the portal vein is borne by the columns of the mucous membranes in the anal canal and produces high pressure in the lower rectum and anal canal. - Exciting causes:
Straining during constipation or over purgation.

Comments (0)