URINARY BLADDER
The urinary bladder is a muscular reservoir of urine, lying in the anterior part of the pelvis.
Location of Urinary Bladder:
The urinary bladder is situated in the anterior part of the lesser pelvis immediately behind the pubic symphysis and in front of the rectum in males and uterus in the female
The location of the urinary bladder varies with the amount of urine it contains and with age:
When the bladder is empty it lies entirely within the lesser pelvis but when it becomes distended with urine, it expands upward and forward into the abdominal cavity
In children, the bladder is an abdominopelvic organ even when it is empty because the pelvic cavity is small and the neck of the bladder lies at the level of the upper border of the pubic symphysis.
Size and Shape:
It is tetrahedral in shape when empty and ovoid in shape when distended.
Capacity
Normally in adult males, the capacity varies from 120 to 320 ml.
The mean capacity is about 220 ml. An amount of urine beyond 220 ml causes a desire to micturate but the bladder is usually empty about 250-300ml
An empty and contracted bladder as seen in a cadaver is tetrahedral in shape and presents the following external features:
- Apex
- Base
- Neck
- Three surfaces (superior and two inferolateral surfaces)
- Four borders (anterior, posterior, and two lateral)
Relations
Base
- Rectovesical pouch in the male
- Vesico uterine pouch in the female
- Vasa deferentia and seminal vesicles (separated from the rectum by fascia of Denonvilliers)
Superior Surface:
- Peritoneal cavity containing loops of ileum
- Coils of ileum
- Sigmoid colon
- Uterine cervix (in female)
Anterior Surface:
- Retropubic space
- Puboprostatic ligaments
- Obturator internus and levator ani muscles
Apex:
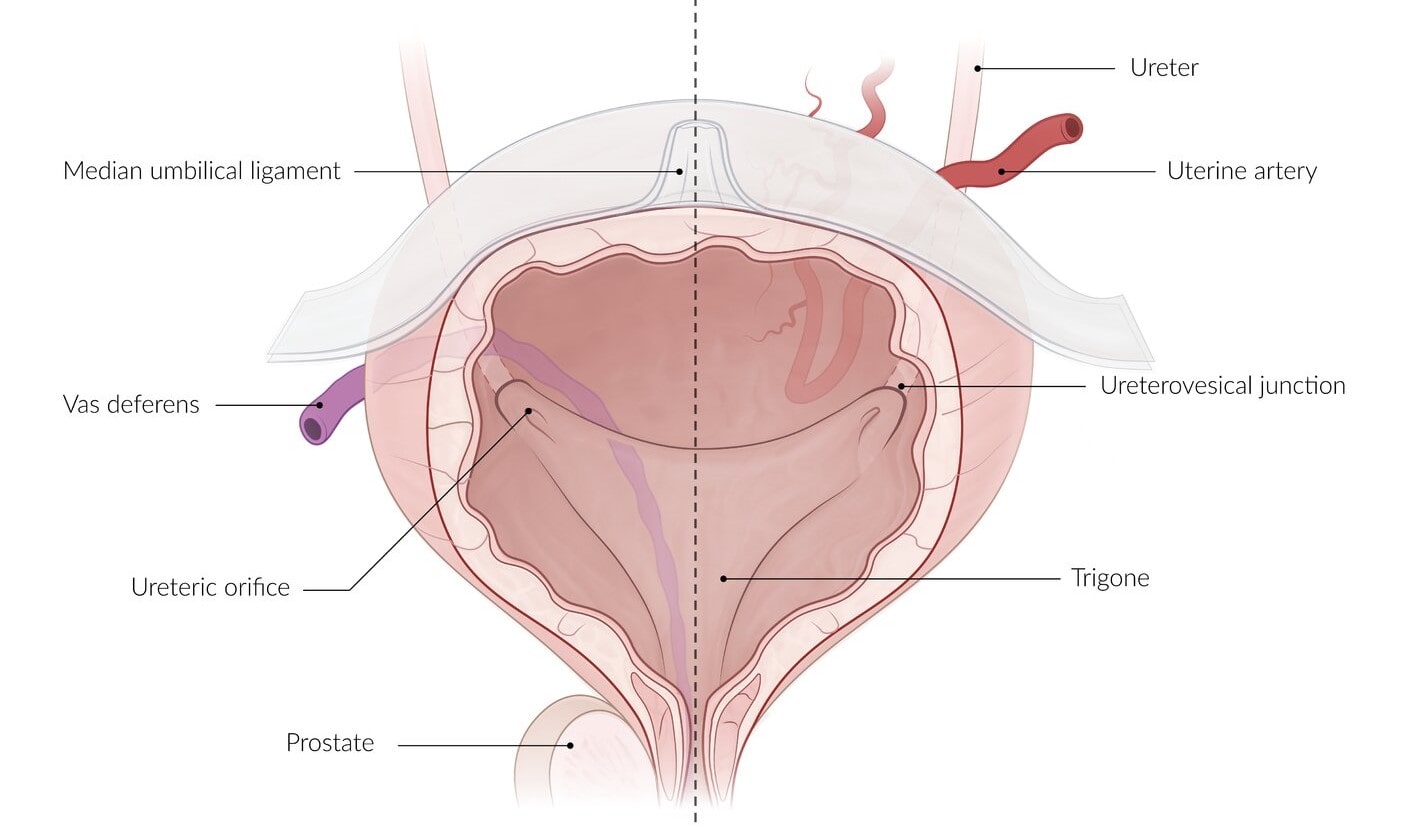
Median umbilical ligament
Neck:
Prostate gland (in male)
Urogenital diaphragm
Ligament of Urinary Bladder:
Ligaments of the bladder are of two types - True and False ligaments
True Ligaments
These are formed by the condensation of pelvic fascia around the neck and the base of the bladder and have a supportive function for the bladder.
- Lateral ligaments (2 in number, right, and left)
- Puboprostatic ligaments (4 in number,)
- Lateral puboprostatic ligament
- Medial puboprostatic ligament
- Median umbilical ligament (Remnant of the urachus. Connects the apex of the urinary bladder to the umbilicus.)
- Posterior ligament (two in number, right, and left)
False Ligaments
These are peritoneal folds and do not have the supportive function as performed by true ligaments. They are seven in number.
Anteriorly there are three folds:
- Median umbilical fold,
- Two medial umbilical folds,
Laterally a pair of false lateral ligament
Posteriorly a pair of the false posterior ligament
INTERIOR OF THE BLADDER
In an empty bladder, the greater part of mucosa shows irregular folds (rugae) because it is loosely attached to the subjacent muscular layer.
Over a small triangular area, immediately above and behind the internal orifice of the urethra (trigone of the bladder), the mucous membrane is firmly bound to the muscular coat and therefore is smooth.
The limits of trigone are defined superiorly by the openings of the ureters and inferiorly by the urethra.
Trigone of urinary bladder presents the following features:
- Anteroinferior angle, formed by the internal orifice of the urethra.
- Two posterosuperior angles, formed by openings of the ureters.
- Uvula vesicae, a slight elevation in the mucous membrane immediately above and behind the internal urethral orifice.
- Interureteric ridge/crest (bar of Mercier) forms the superior boundary of the trigone and connects the two ureteric orifices.
Structure of Urinary bladder
The wall of the urinary bladder presents from outside inwards the following coats
| Serous coat: Derived from the peritoneum. It covers the superior surface and in the male upper part of the base of the bladder. |
| Muscular coat: Muscular coat is also known as detrusor muscle & consists of three ill-defined layers of smooth muscles. Outer longitudinal Middle circular & Inner longitudinal |
| Submucous coat: Consists of loose areolar tissue and is present all over the bladder except the trigone. |
| Mucous coat: The mucosa is lined by transitional epithelium or urothelium. |
Artery Supply of Urinary Bladder:
Superior and Inferior vesical arteries which are the branches of the anterior division of internal iliac arteries.
The other arteries which make a small contribution in supplying the lower part of the bladder
- Obturator and inferior gluteal arteries.
- Uterine and vaginal arteries in the female
VENOUS DRAINAGE
The veins of the bladder do not follow the arteries.
They form a complicated plexus on the inferolateral surfaces near the prostate called the vesical venous plexus.
- This plexus passes backward in the posterior ligaments of the urinary bladder to drain into the internal iliac veins.
- It communicates:
(a) In the male with the prostatic venous plexus.
(b) In the female with the veins at the base of the broad ligament
Nerve supply of Urinary Bladder:
Motor innervation: It is provided by the parasympathetic, sympathetic, and somatic fibers.
| Parasympathetic fibers are derived from S2, S3, S4 (spinal micturition center) segments of the spinal cord. They are motor to the detrusor muscle and inhibitory to the sphincter vesicae (internal urethral sphincter). |
| Sympathetic fibers are derived from T11, T12 thoracic, and L1, L2 lumbar segments of the spinal cord. They are inhibitory to the detrusor and motor to the sphincter vesicae. |
| Somatic fibers (pudendal nerve) are derived from S2, S3, S4 spinal segments. They are motor to the external urethral sphincter. |
Clinical Anatomy of Urinary bladder
Automatic reflex bladder: It results from complete transection of the cord above the lower micturition center (S2, S3, S4) involving pyramidal tracts (upper motor neurons)
Clinically it presents as:–
- The voluntary inhibition and initiation of micturition are lost.
- The bladder empties reflexly every 1 to 4 hours.
- When the filling reaches a certain level, the detrusor muscle contracts reflexly as in early infancy. This is called automatic or reflex bladder.
Also read: Anatomy Question Collection
Also read: Anatomy Questions & Answers
Also read: Anatomy notes

Comments (0)