
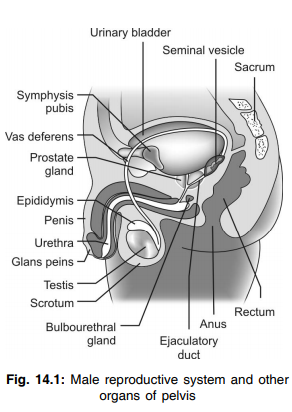
Q.1 Name the sex organs in males.
- The primary sex organs – testes
- The accessory sex organs – seminal vesicles, prostate gland, urethra and external genitalia such as the penis and scrotum.
Q.2 Which chromosome determines the type of sex? What is H-Y antigen?
Y sex chromosome determines the type of sex. The testis determining gene product is known as the H-Y antigen.
Q.3 What do you mean by SRY chromosome?
The gene present in the tip of the short arm of the human Y chromosome causes differentiation of indifferent or bipotential gonad to embryonic testis in the 7th–8th weeks after gestation. The region of the Y chromosome that contains the testis determining gene is called an SRY chromosome.
Q.4 What is sex chromatin or Barr body?
Soon after cell division has started during embryonic development one of the two X chromosomes of the somatic cell in a normal female becomes functionally inactive. The inactive X chromosome is known as sex chromatin or Barr body.
Q.5 What is the name of sex chromatin in males?
It is known as F body.
Q.6 To identify sex genotype certain cells are used for the cytological test. What are these cells?
These are: The epithelial cells of the epidermal spinous layer, buccal mucosa epithelial cells, vaginal epithelial cells, leukocytes.
Q.7. Name the abnormalities of sexual differentiation due to nondisjunction of the sex chromosome?
These are superfemale (44X XX), Klinefelter’s syndrome (44XXY), Turner’s syndrome (44X0).
Q.8 What are the phenotypic features of Klinefelter’s syndrome?
Characteristic features:
- Genetic sex is female
- Chromosomal configuration 44XXY
- Atrophied testis (Gonadal sex)
- Phenotypic features:
– Male like appearance with feminine stigma
– Bilateral Gynecomastia
– Sterile and impotent
– Low or normal plasma testosterone level
– High serum LH but normal FSH level
– Small penis, testis, seminal vesicles, etc.
– Secondary sex characters present
Q.9 Name the abnormality of sexual differentiation due to nondisjunction of autosome.
It is Down’s syndrome or mongolism.
Q.10 What do you mean by male pseudohermaphroditism?
If the female internal genital organs develop in genital male due to less secretion of androgen by defective testis, it is known as pseudohermaphroditism
Q.11 What are seminiferous tubules?
Seminiferous tubules are coiled tubular structures in the testes containing two types of cells, the spermatogenic cells and Sertoli cells.
Q.12 What are the spermatogenic cells?
Spermatogenic cells are the cells producing sperms in the testes. In children, only one type of spermatogenic cells is present called spermatogonia. After puberty, different stages of spermatogenic cells (spermatogonia, primary spermatocytes, secondary spermatocytes, and spermatids) are found in the testes.
Q.13. What are Sertoli cells?
Sertoli cells are the supporting cells present in seminiferous tubules of testes.
Q.14 What are the functions of Sertoli cells?
Sertoli cells:
- Support and nourish the germ cells
- Provide necessary substances like hormones for spermatogenesis
- Convert androgens into estrogen.
- Secrete androgen binding protein, inhibin and Müllerian regression factor.
Q.15 What are the functions of testes?
- Gametogenic function – production of sperms
- Endocrine function – secretion of male sex hormones.
Q.16 What is spermatogenesis?
The production of sperms is known as spermatogenesis.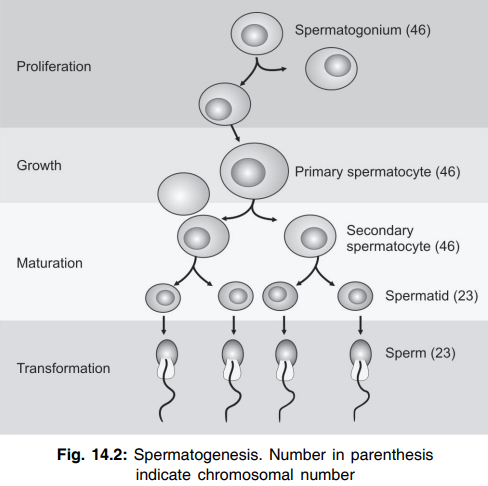
Q.17 Name the stages of spermatogenesis.
- Stage of proliferation
- Stage of growth
- Stage of maturation
- Stage of transformation.
Q.18 At what stage of spermatogenesis the number of chromosomes becomes haploid?
At the stage of maturation, i.e. in the spermatids.
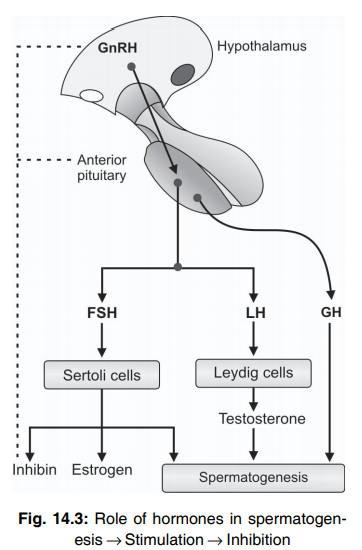
Q.19 Name the hormones necessary for spermatogenesis.
The following hormones are necessary for spermatogenesis :
- Testosterone
- FSH
- LH
- Estrogen
- Growth hormone
Q.20 Name some factors which inhibit spermatogenesis.
- Increase in temperature
- Infectious diseases such as mumps.
Q.21 What are the hormones secreted by testes?
The androgens or male sex hormones – testosterone, dihydrotestosterone, and androstenedione.
Q.22 What is the source of secretion of testosterone?
Testosterone is secreted by the interstitial cells of Leydig present in testes. It is also secreted in small quantities in the adrenal cortex.
Q.23 What is the period of life during which testosterone is not secreted?
During the period between birth and puberty.
Q.24 What are the functions of testosterone in fetal life?
Testosterone helps in:
- Sex differentiation
- Development of sex organs
- Descent of testes.
Q.25 What are the functions of testosterone in adult life?
Testosterone:
- Increases the size of sex organs
- Causes the development of secondary sexual characters such as muscular growth, bone growth, changes in skin, hair distribution, voice, BMR, blood, electrolyte concentration, and water content in the body.
Q.26 How is testosterone secretion regulated?
In a fetus, testosterone secretion is stimulated by human chorionic gonadotropin secreted from the placenta. After puberty, testosterone secretion is stimulated by interstitial cell stimulating hormone (ICSH) secreted by the anterior pituitary. The regulation is by negative feedback mechanism that involves ICSH and LH releasing hormone.
Q.27 What are the effects of extirpation of testes before puberty?
- The infantile sexual characters remain throughout life (eunuchism)
- Height is slightly more
- Bones are weak and thin
- Muscles are weak
- Sex organs do not increase in size and male secondary sexual characters do not develop
- Feminine distribution of fat occurs.
Q.28 What are the effects of extirpation of testes immediately after puberty?
- Functions of sex organs are depressed
- Seminal vesicles and prostate gland undergo atrophy
- Penis remains smaller in size
- Many of the secondary sexual characters such as male distribution of hair, musculature, and thickness of bones are lost
- There is a loss of sexual desire and sexual activities.
Q.29 What are the effects of the extirpation of testes in adults?
- Accessory sex organs such as seminal vesicle and prostate gland degenerate
- Penile erection may occur but there is no ejaculation
- The secondary sexual characters and sexual desire may not be affected much.
Q.30 What is hypergonadism? What is its cause in males?
The condition characterized by hypersecretion of sex hormones from gonads is known as hypergonadism. In males, it is due to the tumor of Leydig cells.
Q.31 What are the effects of hypergonadism in males?
- Rapid growth of muscles, bones, sex organs, and secondary sexual characters
- Height of the person is less because of early closure of the epiphysis
- Development of gynecomastia.
Q.32 What is hypogonadism? What are its causes in males?
The condition characterized by a reduction in the functional activity of gonads is known as hypogonadism.
Causes in males:
- Congenital non-functioning testes
- Underdeveloped testes
- Cryptorchidism
- Castration
- Absence of androgen receptors in testis
- Disorder of gonadotropes
- Hypothalamic disorder.
Q.33 What are the effects of hypogonadism in males?
Effects are similar to the effects of the removal of testes before puberty.
- The infantile sexual characters remain throughout life (eunuchism)
- Height is slightly more
- Bones are weak and thin
- Muscles are weak
- Sex organs do not increase in size and male secondary sexual characters do not develop
- Feminine distribution of fat occurs.
Q.34 What are the functions of fluid secreted from seminal vesicles?
- It provides nutrition to the sperms
- The fibrinogen present in this fluid causes coagulation of semen
- Prostaglandin of the fluid enhances the fertilization of the ovum by increasing the receptivity of cervical mucosa for the sperms and by increasing the rate of transport of sperms through reverse peristaltic movements of the uterus and fallopian tube.
Q.35 What are the functions of prostatic fluid?
- Prostatic fluid provides optimum pH for motility of sperms
- The clotting enzymes in this fluid cause coagulation of semen
- Fibrinolysin present in this fluid causes lysis of coagulum.
Q.36 What is the nature of semen?
At the time of ejaculation, semen is liquid in nature. Immediately it is coagulated and the coagulated semen is known as coagulum. Finally, it undergoes a secondary liquefaction.
Q.37. What are the properties of semen?
Specific gravity : 1.028
Volume : 4 to 6 ml/ejaculation
Reaction: Alkaline with a pH of 7.5
Q.38. What is the composition of semen?
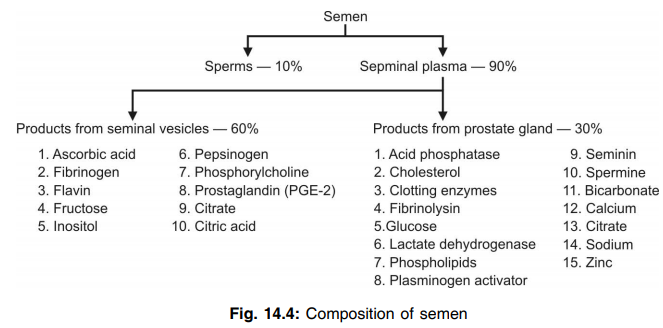
Q.39 What is the normal sperm count?
100 to 150 million/ml of semen
Q.40 At what level of sperm count does the sterility occur in males?
When the sperm count is below 20 million/ ml of semen.
Q.41 What is the blood-testis barrier? What is its function?
In between the Sertoli cells and other cells lining the seminiferous tubular wall, there are tight junctions that prevent the free movement of substances across it. This is known as the blood-testis barrier. Its functions are:
- Helps in maintaining the composition of the fluid in the lumen of the seminiferous tubule.
- It helps to prevent the entry of sperm into the blood and also protects the sperm from blood-borne noxious agents.
Q.42 What is the survival time of sperms after ejaculation?
About 24 to 48 hours at a temperature equivalent to body temperature.
Q.43 Why is scrotal temperature less than the body temperature?
A slightly lower scrotal temperature than the body temperature is essential for the normal production of spermatozoa.
Q.44 Explain the condition of cryptorchidism.
If the tested remains undescended, the seminiferous tubules do not develop due to the higher temperature in the abdominal cavity and subsequently degenerate. Thus, there is no spermatogenesis resulting in sterility. However, the Leydig cells are unaffected and secrete testosterone at puberty, so that all the male secondary sex characters are normally present.
Q.45. Why is scrotal temperature less than the body temperature?
A slightly lower scrotal temperature than the body temperature is essential for the normal production of spermatozoa.
Q.46 Explain the condition of cryptorchidism.
If the tested remains undescended, the seminiferous tubules do not develop due to the higher temperature in the abdominal cavity and subsequently degenerate. Thus, there is no spermatogenesis resulting in sterility. However, the Leydig cells are unaffected and secrete testosterone at puberty, so that all the male secondary sex characters are normally present.
Q.47 Name the sex organs in females.
- The primary sex organs – ovaries
- The accessory sex organs – fallopian tubes, uterus, cervix, vagina, and external genitalia such as labia majora, labia minora, and clitoris.
Q.48 Name the hormones secreted by ovaries.
- Female sex hormones – estrogen and progesterone
- Inhibin
- Relaxin
- Small quantities of androgens.
Q.49 What are the sources of estrogen?
In a nonpregnant female: Follicles of ovaries
During pregnancy: Corpus luteum and placenta A small quantity of estrogen is secreted from the adrenal cortex throughout life.
Q.50 What are the actions of estrogen on the uterus?
Estrogen causes:
- Enlargement of uterus
- Increase in blood supply to the uterus
- Deposition of glycogen and fats in endometrium
- Proliferation and dilatation of endometrial blood vessels
- Proliferation and dilatation of endometrial glands
- Increase in spontaneous activity of uterine muscles and sensitivity to oxytocin
- Increase in the contractility of uterine muscles.
Q.51 What are the actions of estrogen on fallopian tubes?
Estrogen:
- Increases the number and size of ciliated epithelial cells lining the fallopian tubes
- Increases the activity of cilia that facilitates the movement of the ovum through the fallopian tube
- Enhances the proliferation of glandular tissues in fallopian tubes.
Q.52 What are the actions of estrogen on the vagina?
Estrogen:
- Changes the cuboidal epithelium of the vagina into stratified epithelium, which has more resistance to trauma and infection
- Increases the number of layers of vaginal epithelium by proliferation
- Reduces the pH of the vagina causing more acidity.
Q.53 What are the actions of estrogen on mammary glands?
Estrogen increases the size of mammary glands by causing:
- Development of stromal tissues
- Extensive growth of ductile system
- Deposition of fat in the ductile system.
Q.54 What are the female secondary sexual characters influenced by estrogen?
- Hair growth in the pubic region and axilla and profuse hair growth in the scalp
- Softness, smoothness, and increased vascularity of the skin
- Narrow shoulders, broad hip, converged thighs and diverged arms, and deposition of fat in breasts and buttocks
- Retention of prepubertal voice with high pitch.
Q.55. What are the actions of estrogen on bones?
Estrogen increases osteoblastic activity that accelerates the height at the time of puberty. At the same time, it causes early closure of epiphysis.
Q.56 What are the actions of estrogen on metabolism?
Estrogen increases the protein synthesis and causes deposition of fat in the subcutaneous tissues, breasts, buttocks, and thighs.
Q.57 How is the secretion of estrogen-regulated?
The secretion of estrogen is regulated by FSH secreted from the anterior pituitary through a negative feedback mechanism. The secretion of FSH, in turn, is under the control of gonadotropic releasing hormone secreted from the hypothalamus.
Q.58 What are the sources of progesterone?
In a nonpregnant female: Small quantity of progesterone is secreted from theca cells of the ovary during the follicular phase and a large quantity is secreted from the corpus luteum of the ovary during the luteal phase of the menstrual cycle.
In the first trimester of pregnancy: the Corpus luteum and placenta secrete a large quantity of progesterone. A small quantity is secreted from the adrenal cortex throughout life.
Q.59 What are the actions of progesterone on the uterus?
Progesterone increases:
- Thickness of endometrium
- Size of the uterine glands
- Secretory activities of glandular epithelial cells
- Deposition of lipid and glycogen in the stromal cells
- Blood supply to endometrium. It decreases the frequency of uterine contractions, which favor the implantation and continuation of pregnancy.
Q.60 What is the action of progesterone on fallopian tubes?
Progesterone increases the secretion from the mucosa of the fallopian tube that is essential for the nutrition of the fertilized ovum.
Q.61 What are the actions of progesterone on mammary glands?
Progesterone:
- Promotes the development of lobules and alveoli of mammary glands
- Makes the mammary glands secretory in nature.
- Increases the size of mammary glands by increasing the secretory activity and fluid accumulation in the subcutaneous tissue.
Q.62 Define the menstrual cycle.
The cyclic event which takes place in a rhythmic fashion during the reproductive period of a women’s life is called the menstrual cycle.
Q.63 What is the normal duration of the menstrual cycle?
The normal duration of the menstrual cycle is 28 days. Under normal conditions, it ranges between 20 and 40 days.
Q.64. What is menarche? At what age does it occur?
The commencement of the menstrual cycle is known as menarche. It occurs at the age of 12 to 15 years that marks the onset of puberty.
Q.65. Enumerate the changes taking place during the menstrual cycle.
- Ovarian changes
- Uterine changes
- Vaginal changes
- Changes in cervix uteri.
Q.66 Name the phases of ovarian changes during the menstrual cycle.
- Follicular phase – there is development of Graafian follicle and secretion of large amount of estrogen
- Luteal phase – there is development of corpus luteum and secretion of large amounts of progesterone.
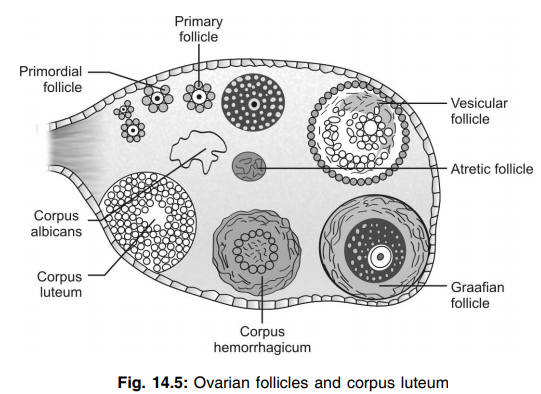
Q.67 Name the different ovarian follicles.
The different ovarian follicles are
- Primordial follicle
- Primary follicle
- Vesicular follicle
- Graafian follicle
Q.68. What is ovulation? When does it occur?
The process by which the ovum is released by the rupture of the Graafian follicle is known as ovulation. It occurs on the 14th day of the menstrual cycle in a normal 28 days cycle.
Q.69 How does ovulation occur?
Ovulation occurs because of the rupture of stigma which is a protrusion developed on the surface of the Graafian follicle. Rupture of the Graafian follicle releases ovum into the abdominal cavity.
Q.70 What are the different phases of the menstrual cycle and what is its cause?
There are 4 phases:
- Menstrual phase: It is due to the withdrawal of progesterone secretion.
- Proliferative phase: It is due to estrogen secretion.
- Ovulatory phase: It is due to the LH surge.
- Secretory or luteal phase: It is due to an increase in the secretion of progesterone.
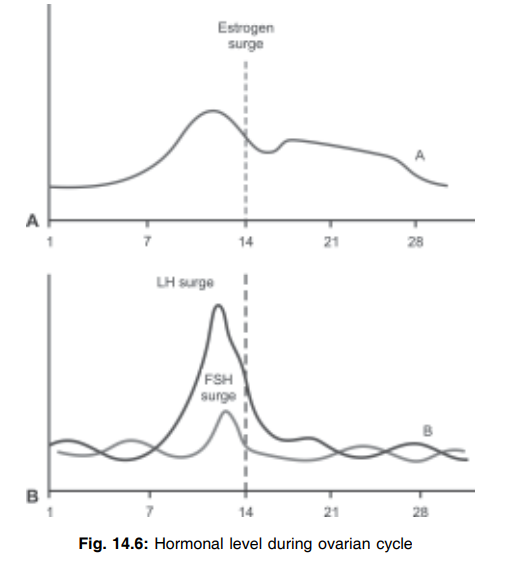
Q.71 What is estrogen surge, FSH surge, and LH surge?
In the preovulatory phase of the menstrual cycle rise of FSH concentration increases the serum concentration of estradiol to reach a peak at 12-13 days (in case of 28 days cycle), called estrogen surge
Within 24 hours of estrogen surge, the increased level of estrogen augments the responsiveness of the pituitary to GnRH which induces a burst of LH secretion. This peak rise of LH in serum just prior to ovulation is known as LH surge.
At the same time when LH peak occurs serum concentration of FSH also increases suddenly to a peak level called FSH surge.
Q.72 What do you mean by withdrawal bleeding?
If no fertilization takes place, the corpus luteum regresses by the process known as luteolysis resulting in a sharp fall of estrogen and progesterone secretion. This inturn causes spasm in spiral arteries and thereby ischemia of the superficial layer of endometrium. This ultimately leads to the shedding of the superficial layer of endometrium and thereby release of blood and mucous through the vagina known as withdrawal bleeding.
Q.73 How is ovulation time determined?
- By determining basal body temperature
- By determining the hormonal excretion in urine
- By determining hormonal level in plasma
- By ultrasound scanning.
Q.74 What is the physiological basis of BBT as an indicator of ovulation?
At the time of ovulation, body temperature rises by 0.3 to 0.5°C than the temperature at the preovulatory phase. This increase in temperature is due to the increase of progesterone level in the blood which is thermogenic.
Q.75 What is the importance of knowing ovulation time?
Determination of ovulation time is necessary to adopt the rhythm method (safe period) of family planning.
Q.76 What is corpus luteum?
The glandular yellow body that develops from the remaining cells of the Graafian follicle after the release of an ovum (after ovulation) is known as corpus luteum.
Q.77 Name the types of cells present in corpus luteum.
- Lutein cells derived from granulosa cells
- Cells of theca interna. The lutein cells are surrounded by cells of theca externa.
Q.78 What is the function of corpus luteum?
Corpus luteum:
- Functions as a temporary endocrine gland and secretes large amounts of progesterone and a small amount of estrogen.
- Helps to maintain the pregnancy in the first trimester (till the placenta starts secreting the hormones).
Q.79 What is the fate of corpus luteum?
The fate of the corpus luteum depends on whether pregnancy occurs or not.
If pregnancy does not occur: It involutes and degenerates into corpus luteum menstrualis or spurium. The corpus luteum menstrualis is transformed into a whitish scar called corpus Albicans.
If pregnancy occurs: It increases in size and remains for 3 to 4 months. During this period, it secretes a large amount of progesterone and a small amount of estrogen, which are essential to maintain pregnancy
Q.80 Name the phases of uterine changes during the menstrual cycle.
- Menstrual phase
- Proliferative phase
- Secretory phase.
Q.81 What are the uterine changes during the menstrual phase?
The endometrium becomes involuted and desquamated. It is followed by vasoconstriction and hypoxia leading to necrosis and bleeding.
Q.82 What are the causes of uterine changes during the menstrual phase?
At the end of the menstrual cycle, there is a sudden decrease in the level of estrogen and progesterone. This leads to sudden involution of endometrium at the beginning of the next cycle. Since estrogen and progesterone are vasodilators, the lack of these hormones causes severe vasoconstriction. Prostaglandin secreted by the involuted endometrium also causes vasoconstriction. Due to severe vasoconstriction, hypoxia and necrosis occur in the endometrium. Necrosis causes the rupture of blood vessels leading to bleeding.
Q.83 What is the composition of menstrual fluid?
- Blood (about 35 ml)
- Serous fluid (about 35 ml)
- Desquamated endometrial tissues.
Q.84 How much of blood is lost during the menstrual phase?
About 35 ml
Q.85 Why the menstrual blood does not clot?
During menstruation, blood clots as soon as it oozes into the uterine cavity. Fibrinolysin released from the endothelium of damaged blood vessels causes lysis of the clot in the uterine cavity itself so that the menstrual blood does not clot.
Q.86 What are the uterine changes during the proliferative phase?
- Endometrial cells proliferate
- Epithelium reappears on the surface of the endometrium
- Uterine glands start developing
- Blood vessels also appear in stroma
- Endometrium reaches a thickness of 3-4 mm.
Q.87 What are the uterine changes during the secretory phase?
- The uterine glands increase in size and become more tortuous
- Cytoplasm of stromal cells increases due to the deposition of glycogen and lipids
- New blood vessels appear in endometrium
- Blood supply to the endometrium increases
- Thickness of the endometrium increases to about 5 – 6 mm.
Q.88 What are vaginal changes during the menstrual cycle?
During the proliferative phase, the vaginal epithelium is cornified because of the influence of estrogen. During the secretory phase, there is a proliferation of vaginal epithelium because of the action of progesterone. There is an infiltration of leukocytes in the vaginal epithelium during this phase.
Q.89 What are the changes, which occur in the cervix during the menstrual cycle?
During the menstrual phase, under the influence of estrogen, the mucus membrane of the cervix becomes thin and alkaline. This helps for the survival and motility of sperms. During the secretory phase, because of the action of progesterone, the mucus membrane of the cervix becomes thick and adhesive.
Q.90 Name the hormones, which influence the ovarian changes during the menstrual cycle.
During follicular: FSH, LH, and phase estrogen
During ovulation: LH
During the luteal phase: FSH and LH.
Q.91 Name the hormones, which influence the uterine changes during the menstrual cycle.
During proliferative: Estrogen phase
During secretory: Progesterone phase
During menstrual: Sudden withdrawal phase of estrogen and progesterone.
Q.92 What are the abnormal types of menstruation?
- Amenorrhea – Absence of menstruation during the reproductive period of females
- Hypomenorrhea – decreased menstrual fluid
- Menorrhagia – excessive menstrual bleeding
- Oligomenorrhea – decreased frequency of menstrual bleeding
- Polymenorrhea – increased frequency of menstrual bleeding
- Dysmenorrhea – menstruation with pain
- Metrorrhagia – uterine bleeding in between menstruations.
Q.93 What is an anovulatory cycle?
The menstrual cycle without ovulation is called an anovulatory cycle.
Q.94 What is menopause?
In females, the permanent stoppage of menstruation in old age is known as menopause.
Q.95 What is the cause of menopause?
Throughout life, there is a degeneration of primordial follicles in the ovary. At the age of 45 years and above, the number of primordial follicles reduces leading to a decrease in the secretion of estrogen by the ovary. When all the primordial follicles are atrophied estrogen secretion stops completely. This period is called menopause.
Q.96 What is postmenopausal syndrome?
After the onset of menopause, the woman develops certain physical, physiological, and psychological changes, which are collectively known as postmenopausal syndrome.
Q.97 How is postmenopausal syndrome treated?
Postmenopausal syndrome can be treated by psychotherapy and hormone therapy. In hormone therapy, estrogen and progesterone are administrated with careful adjustment of dose.
Q.98 What are the causes of male infertility?
- Decrease in sperm count to about 20 million/ml
- Presence of abnormal sperms like tailless sperms, two-headed sperms, and nonmotile sperms
- Obstruction of reproductive ducts like vas deferens.
Q.99 Where does fertilization of the ovum occur?
Fertilization of the ovum occurs in the fallopian tube.
Q.100 When does the zygote get implanted in the uterus?
After fertilization, the zygote takes 3 to 5 days to reach the uterus. In the uterus, the zygote remains freely in the uterine cavity for 2 to 4 days and then gets implanted. So, it takes about one week for the zygote to get implanted.
Q.101 What is the duration of pregnancy (gestation period)?
280 days (40 weeks) from the date of the last menstrual period.
Q.102 What are the changes taking place in the ovary during pregnancy?
When pregnancy occurs, follicular growth does not occur in the ovary because of a lack of FSH and LH. The Corpus luteum grows in size and remains for three months and secretes a large amount of progesterone and a small amount of estrogen. After the third month of pregnancy, when the placenta starts secreting the hormones, the corpus luteum degenerates.
Q.103 What are the changes taking place in the uterus during pregnancy?
- Increase in the volume (from 0 to 5 – 7 liters), size, and weight (from 30 – 50 gm to 1000 – 1200 gm) of the uterus
- Shape of the uterus changes from pyriform to globular
- Histological changes also occur with the development of decidua.
Q.104 What are the changes taking place in the vagina during pregnancy?
- Size increases
- Violet coloration due to increase in blood supply
- Epithelial cells become less cornified
- Glycogen deposition increases in epithelial cells
- pH decreases to less than 3.5.
Q.105 What are the changes taking place in the cervix during pregnancy?
- Increase in number of cervical glands
- Hypertrophy of endocervix which gives honeycomb appearance
- Increase in blood supply
- Increase in mucus secretion
- Softening of cervix
- Formation of the mucus plug, which closes the cervical canal.
Q.106 What are the changes taking place in mammary glands during pregnancy?
- Development of new ducts
- Formation of new alveoli
- Deposition of fat
- Increase in size
- Increase in vascularization
- The pigmentation of nipple and areola.
Q.107 How much is the weight gain of the body during pregnancy?
The average weight gain of the body during pregnancy is about 12 kg
Fetal weight : 3.5 kg
Amniotic fluid weight : 2.0 kg
Placental weight : 1.5 kg
Increase in maternal body weight: 5.0 kg
Q.108 What are the metabolic changes during pregnancy?
- Increase in BMR
- Increase in protein synthesis
- Increase in blood glucose level that may lead to diabetes in pregnancy
- Deposition of fat in maternal body with increased blood cholesterol level and ketosis
- Retention of water, sodium, calcium, and phosphorus.
Q.109 What are the changes taking place in blood during pregnancy?
- Blood volume increases by about 20% (1 liter) mainly because of the increase in plasma volume
- Hemodilution occurs
- Anemia may develop.
Q.110 What are the cardiovascular changes during pregnancy?
- Cardiac output increases
- Blood pressure decreases slightly in the second trimester
- Hypertension may develop later if proper prenatal care is not taken.
Q.111 What are the changes taking place in the excretory system during pregnancy?
- Increase in renal blood flow, glomerular filtration rate, and urine formation
- Formation of dilute urine
- Increase in frequency of micturition.
Q.112 What are the changes taking place in the digestive system during pregnancy?
- Morning sickness involving nausea, vomiting, and giddiness occurs during the initial stage of pregnancy
- Movement of the gastrointestinal tract decreases resulting in constipation
- Indigestion and hypochlorhydria may occur.
Q.113 What are the changes taking place in endocrine glands during pregnancy?
Generally, all the endocrine glands increase in size with increased hormonal secretion.
Q.114 What are the changes taking place in the nervous system during pregnancy?
During the early stages of pregnancy, there is excitement of the nervous system leading to psychological imbalance such as change in the moods, excitement, and depression.
Q.115 What is preeclampsia?
Toxemia of blood characterized by elevated blood pressure is known as preeclampsia.
Q.116 What is parturition?
Expulsion or delivery of the fetus from the mother’s body at the end of pregnancy is known as parturition.
Q.117 Enumerate the hormones involved in the process of parturition.
- Maternal hormones – oxytocin, prostaglandins, cortisol, catecholamines, and relaxin
- Fetal hormones – oxytocin, cortisol, and prostaglandins
- Placental hormones – estrogen, progesterone, and prostaglandins.
Q.118 What is the role of estrogen in parturition?
Estrogen increases the force of uterine contractions and the number of oxytocin receptors in the uterine wall. It also accelerates the synthesis of prostaglandins.
Q.119 What is the role of progesterone in parturition?
Progesterone does not play any role in parturition. But, it is responsible for the suppression of uterine contractions throughout the period of gestation. So, it is essential for the maintenance of pregnancy. At the end of the gestation period, progesterone secretion decreases suddenly and parturition is induced.
Q.120 What is the role of oxytocin in parturition?
Oxytocin causes contraction of the uterus and enhances labor through positive feedback mechanisms and neuroendocrine reflex.
Q.121 What is double Bohr’s effect?
Reduction in the affinity of hemoglobin for oxygen due to increased carbon dioxide tension is known as Bohr’s effect. On the other hand, when the carbon dioxide tension decreases, the affinity for oxygen is increased. In a fetus, along with metabolic end products, carbon dioxide is completely excreted from fetal blood into the mother’s blood. This develops low partial pressure of carbon dioxide in the fetal blood. So, the affinity of fetal hemoglobin for oxygen increases resulting in the diffusion of more amount of oxygen from the mother’s blood into fetal blood.
Simultaneously, the partial pressure of carbon dioxide increases in the mother’s blood. This reduces the affinity of hemoglobin in the mother’s blood for oxygen resulting in the diffusion of more amount of oxygen from the mother’s blood into fetal blood. This type of operation of Bohr’s effect in both fetal blood and mother’s blood is known as double Bohr’s effect.
Q.122 What are the hormones secreted by the placenta?
- Human chorionic gonadotropin (hCG)
- Estrogen
- Progesterone
- Human chorionic somatomammotropin (HCS)
- Relaxin.
Q.123 What are the actions of hCG?
- hCG is responsible for the preservation and maintenance of secretory activity of corpus luteum
- In a male fetus, it stimulates the interstitial cells of Leydig and causes secretion of testosterone.
Q.124 What are the actions of human chorionic somatomammotropin (HCS)?
HCS:
- Causes enlargement of mammary glands in animals. But, in human beings, its action on mammary glands is not known
- Causes synthesis of proteins
- Reduces peripheral utilization of glucose in the mother resulting in the availability of more glucose for the fetus
- Causes mobilization of fat from fat depots, thus making the availability of a large quantity of free fatty acids for energy production in the mother’s body.
Q.125 What is the fetoplacental unit?
The fetus and placenta are together called the fetoplacental unit because of their interaction during the synthesis of steroid hormones.
Q.126 Explain the function of the fetoplacental unit briefly.
Cholesterol, the precursor for steroid hormones enters the placenta from the mother’s blood. From cholesterol, the placenta synthesizes pregnenolone. From pregnenolone, progesterone is synthesized. Some amount of pregnenolone enters the fetus from the placenta. The fetal liver also produces a small amount of pregnenolone. From pregnenolone, dehydroepiandrosterone sulfate (DHEAS) and 16–hydroxy dehydroepiandrosterone sulfate (16 DHEAS) are formed. DHEAS and 16 – DHEAS enter the placenta from the fetus to form estrogen. Some amount of progesterone enters the fetus from the placenta to form cortisol and corticosterone in the fetal adrenal gland.
Q.127 What do you mean by double Bohr’s effect?
In the fetoplacental unit while flowing through the placenta the PCO2 of fetal blood decreases due to pressure gradient. This shifts the O2 - Hb dissociation curve to the left to cause increased loading of O2 by the fetal blood. Whereas PCO2 of maternal blood increases as it picks up the CO2 from fetal blood. This shifts O2–Hb dissociation curve to the right and causes increased unloading of O2. This event is known as double Bohr’s effect.
Q.128 What is the basis for pregnancy tests?
Determination of presence or absence of the hormone called human chorionic gonadotropin (hCG) in the urine of women suspected of pregnancy.
Q.129 What is the principle of immunological test for pregnancy?
The principle of the immunological test is to determine the presence or absence of agglutination of sheep’s red blood cells or latex particles coated with hCG. The presence of agglutination indicates that the woman is not pregnant. And the absence of agglutination indicates that the woman is pregnant.
Q.130 What are the advantages of immunological tests for pregnancy?
- Immunological test is accurate
- The result is obtained within a few minutes
- Procedure of the tests is easy to perform
- Test can be performed within the first few days of conception.
Q.131 Name the hormones involved in the growth of mammary glands.
Estrogen, progesterone, prolactin, growth hormone, thyroxine, cortisol, and placental hormones.
Q.132 What are the processes involved in lactation?
- Milk secretion
- Milk ejection.
Q.133 What are the phases of milk secretion?
- Initiation of milk secretion or lactogenesis
- Maintenance of milk secretion or galactopoiesis.
Q.134 What are the hormones involved in milk secretion?
Prolactin is necessary for the initiation of milk secretion. Growth hormone, thyroxine, and cortisol are necessary for the maintenance of milk secretion.
Q.135 What are the contraceptive methods in females?
- Rhythm method
- By using mechanical barriers like cervical cap or diaphragm
- Pill method (oral contraceptives)
- By using intrauterine contraceptive devices (IUCD)
- Tubectomy.
Q.136 What is a safe period? When does it exist?
The period of the menstrual cycle during which there is no danger of pregnancy after sexual intercourse is known as a safe period. It is 4 to 5 days after menstrual bleeding and 5 to 6 days before the onset of the next menstrual cycle.
Q.137 What is the disadvantage of the rhythm method of conception?
The knowledge of determining the time of ovulation is difficult for uneducated or less educated women. So, it is not a successful method among such women. Also, there must be an understanding between the couples regarding this, and self restrain is essential. Otherwise, it cannot be practiced.
Q.138 What are oral contraceptives?
The oral pills containing synthetic estrogen and progesterone are known as oral contraceptives.
Q.139 What is the mechanism of action of oral contraceptive pills?
Oral contraceptive pills prevent the maturation of follicles and ovulation by suppressing the secretion of gonadotropins from pituitary. Thus, the menstrual cycle becomes anovulatory in nature under the influence of these pills.
Q.140 Name the types of oral contraceptives.
- Classical pills
- Sequential pills
- Mini pills.
Q.141 What are the disadvantages of using oral contraceptive pills?
- Regular intake of pills without fail is difficult
- Long term use of these pills results in inhibition of synthesis of anticoagulants and clotting factors and endometrial carcinoma.
Q.142 What is the mechanism of action of intrauterine contraceptive device (IUCD)?
The IUCD prevents fertilization and implantation of the ovum. The IUCD with copper content has got spermicidal action also.
Q.143 Name the commonly used IUCD.
Lippe’s loop and copper T.
Q.144 What are the disadvantages of using IUCD?
- It causes heavy bleeding in some women
- It has the tendency to cause infection
- It may come out of the uterus accidentally.
Q.145 What is the medical termination of pregnancy? How is it done?
Abortion during the first few months of pregnancy is called medical termination of pregnancy (MTP).
There are three ways of doing MTP:
• Dilatation and curettage (D and C)
• Vacuum aspiration
• Administration of prostaglandin.
Q.146 What is the permanent method of sterilization in females?
The permanent method of sterilization in females is tubectomy. In this, the fallopian tubes are cut and the cut ends are ligated so that, the entry of the ovum into the uterus is prevented. Though this can cause permanent sterility, if necessary, recanalization of the fallopian tube can be done using a plastic tube.
Q.147 Name the contraceptive methods in males.
- Using condoms
- Vasectomy.
- Coitus interruptus
- Drugs which inhibit spermatogenesis (under research)
Q.148 What is the permanent method of sterilization in males?
The permanent method of sterilization in males is vasectomy. In this, the vas deferens is cut and the cut ends are ligated so that, the entry of sperms into the ejaculatory duct and into semen is prevented. Though vasectomy causes permanent sterility, if necessary recanalization of vas deferens can be done.
Q.149 What are the differences between human's milk and cow’s milk?

Q.150 When does the heartbeat begins in the fetus?
It begins by 4th week of pregnancy.
Q.151 When does GIT develop in the fetus?
It starts to develop by 4th month and by the 7th month it grows almost up to the normal stage.
Q.152 When do the kidney develops in the fetus?
These develop mostly by 3rd trimester of pregnancy but normal functioning becomes complete only a few months before birth.
Q.153 What is the main source of energy in fetal metabolism?
Glucose is the main source of energy for the fetus.
Also read: Physiology Questions & Answers

Comments (0)