Important viva collections
What is a hormone?
The hormone is a chemical messenger that is secreted usually by a ductless (endocrine) gland and also by some other structures like the kidney and heart.
Classify the chemical messengers.
- Endocrine messengers – classical hormones secreted by endocrine glands
- Neurocrine messengers – neurotransmitters released from nerve endings
- Paracrine messengers which diffuse from control cells to target cells
- Autocrine messengers which control the source cells which secrete them.
Classify the classical hormones.
Classical hormones are classified by their chemical nature:
- Steroid hormones
- Protein hormones
- Hormones that are derived from the amino acid tyrosine.
Classify the hormones by citing examples of each.
Hormones are classified into 3 major classes:
- Steroids - Like adrenocortical hormones, sex hormones, and Vit-D3
- Proteins and polypeptides - Like anterior and posterior pituitary hormones,
- Hypothalamic hormones, parathyroid hormones, calcitonin, insulin, glucagon, gastrin, secretin, and angiotensin.
- Amino acid derivatives - Epinephrine, norepinephrine, thyroxine.
Name the hormones secreted by the following organs.
- Hypothalamus - Releasing hormones, like GnRH, TRH, CRH, etc.
- Anterior pituitary - TSH, ACTH, GH, FSH, LH, prolactin.
- Posterior pituitary - ADH and oxytocin.
- Thyroid - thyroxin, Triiodothyronine, and thyrocalcitonin
- Parathyroid - Parathormone (PTH)
- Adrenal cortex - Cortisol, corticosterone, aldosterone, androgens, estrogens and progesterone.
- Adrenal medulla - Adrenaline and noradrenaline.
- Testis - Testosterone
- Ovary - Estrogen and progesterone
- Placenta - HCG, estrogen, progesterone, HPL
- GIT - Gastrin, secretin, motilin, substance-P, cholecystokinin
- Kidney - Erythropoietin, Vit-D3, Renin
- Heart - ANF (Atrial natriuretic factor)
What do you mean by long loop feedback, short loop feedback, and ultrashort loop feedback?
- When peripheral gland hormones or substances from tissue metabolism exert negative feedback control on both the hypothalamus and anterior pituitary hormones, it is known as a long-loop feedback mechanism.
- When anterior pituitary hormones exert negative feedback control over the synthesis and release of hypothalamic releasing hormones, it is known as a short-loop feedback mechanism.
- When hypothalamic-releasing hormones after its secretion inhibits their own synthesis further and release it is known as an ultrashort loop.
What do you mean by hypothalamohypophyseal portal vessels and the hypothalami-hypophyseal fiber tract?
The glandular part of the pituitary gland has vascular connections with the hypothalamus through a set of portal vessels through which hypothalamic-releasing hormones enter into adenohypophysis to regulate their secretion. These portal blood vessels are known as the hypothalami-hypophyseal portal tract.
Whereas the neurohypophysis is connected with the hypothalamus by hypothalami-hypophyseal fiber tracts from supraoptic and paraventricular nuclei of the anterior hypothalamus. These tracts are known as the hypothalamohypophyseal fiber tract through which those above-mentioned nuclei pass the oxytocin and vasopressin into the posterior pituitary gland for storage.
How do you classify anterior pituitary gland cells histologically?
Anterior pituitary gland cells are classified list logically.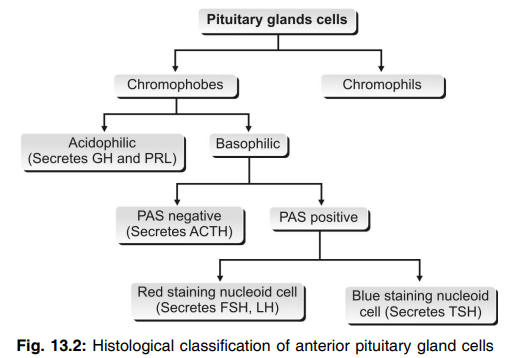
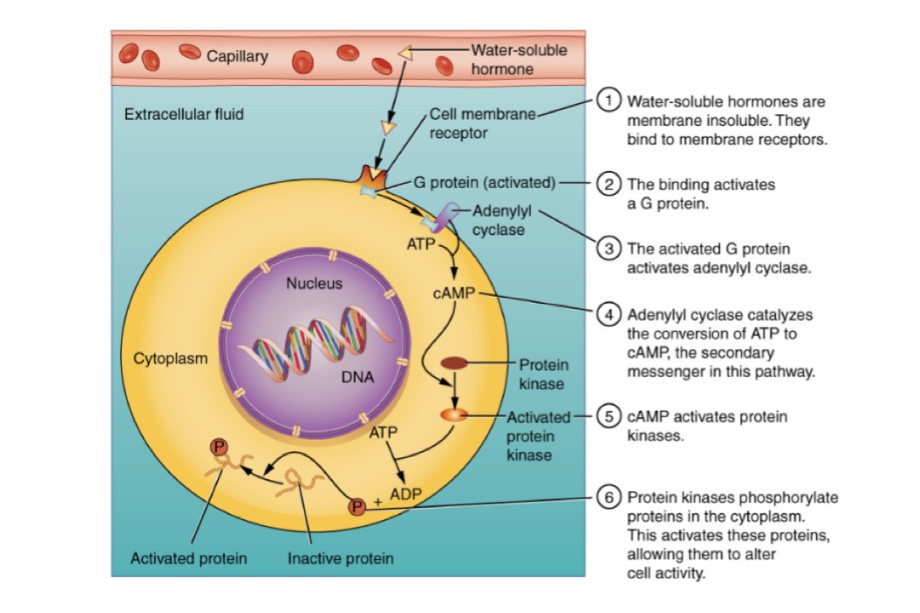
Where are the hormonal receptors situated in the target cell?
The receptors of catecholamines and protein hormones are situated in the cell membrane. The receptors of steroid hormones are in the cytoplasm. And, the receptors of thyroid hormones are situated in the nucleus.
Name the mechanism of action of different types of hormones.
Hormones act by any of the following mechanisms:
- By altering the permeability of the cell membrane – neurotransmitters
- By activating the intracellular enzymes and formation of second messenger–protein hormones and catecholamines
- By activating the genes – thyroid and steroid hormones.
What is the second messenger?
The substance through which the hormonal actions are executed is known as the second messenger.
Name some second messengers.
Cyclic AMP, calcium, calmodulin, inositol triphosphate (IP3), diacylglycerol (DAG), and cyclic GMP are second messengers.
What are G proteins?
G proteins or guanosine nucleotide-binding proteins are the membrane proteins to which the receptor proteins are attached in most of the target cells.
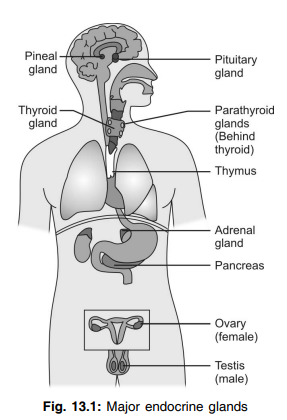
Name the major endocrine glands in the body.
Pituitary gland, thyroid gland, parathyroid gland, adrenal glands, islets of Langerhans in the pancreas, and gonads (ovaries in females and testes in males).
Where is the pituitary gland (hypophysis) situated?
The pituitary gland (hypophysis) is situated at the base of the brain in sella turcica.
What are the two parts of the pituitary gland?
- Anterior pituitary or adenohypophysis
- Posterior pituitary or neurohypophysis.
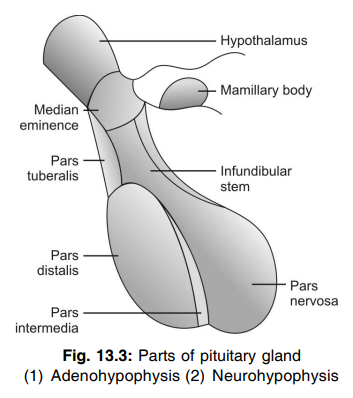
Name the parts of the anterior pituitary.
- Pars distalis
- Pars tuberalis
- Pars intermedia.
Name the types of cells in the anterior pituitary.
- Somatotropes
- Corticotropes
- Thyrotropes
- Gonadotropes
- Lactotropes
Enumerate the hormones secreted by the anterior pituitary.
- Growth hormone
- Thyroid-stimulating hormone
- Adrenocorticotropic hormone
- Follicle-stimulating hormone
- Luteinizing hormone
- Prolactin
What are the gonadotropic hormones?
Follicle-stimulating hormone and luteinizing hormone are together called gonadotropic hormones or gonadotropins because of their action on gonads.
How is the anterior pituitary regulated?
The anterior pituitary is regulated by the hypothalamus by the secretion of releasing and inhibitory hormones, which reach the anterior pituitary through hypothalamic hypophyseal portal vessels.
Name the releasing hormones, which regulate the anterior pituitary.
- Growth hormone-releasing hormone
- Growth hormone-releasing polypeptide
- Thyrotropic releasing hormone
- Corticotropin-releasing hormone
- Gonadotropin-releasing hormone
Name the inhibitory hormones, which control the anterior pituitary.
- Growth hormone inhibitory hormone or somatostatin
- Prolactin inhibitory hormone.
What are the metabolic effects of growth hormones?
Growth hormone acts on protein, carbohydrate, and fat metabolism.
- On protein metabolism – it increases protein synthesis
- On carbohydrate metabolism – it increases the conservation of sugar
- On fat metabolism – it increases the mobilization of fat from fat depots and utilization of fat.
How does growth hormone increase protein synthesis?
Growth hormone increases protein synthesis by
- Increasing amino acid transport through the cell membrane
- Increasing RNA translation
- Increasing transcription of DNA to RNA
- Decreasing the catabolism of proteins.
How does growth hormone act as a protein sparer?
Growth hormone acts as a protein sparer by mobilizing fats from fat depots and making them available for energy production so that the proteins are not broken down.
How does growth hormone increase the blood sugar level?
Growth hormone increases the blood sugar level by:
- Decreasing the peripheral utilization of glucose
- Increasing the deposition of glycogen in the cells and saturating the cells with glycogen
- Decreasing the uptake of glucose by the cells.
What is the effect of growth hormones on bones?
In a fetus, the growth hormone is responsible for the differentiation and development of bone cells. During childhood till puberty, growth hormone increases the length and thickness of bone. After puberty when the head of the bone fuses with the shaft, the growth hormone increases the thickness of the bones.
How is the secretion of growth hormone regulated?
Growth hormone secretion is regulated by hormones secreted by the hypothalamus:
- Growth hormone-releasing hormone
- Growth hormone-releasing polypeptide
- Growth hormone inhibitory hormone (somatostatin).
Whenever the blood level of growth hormone decreases, the hypothalamus secretes growth hormone releasing hormone, and growth hormone releasing polypeptide which in turn acts on the pituitary and increases the secretion of growth hormone. When the blood level of growth hormone increases, it is controlled by a negative feedback mechanism. Hypothalamus secretes growth hormone inhibitory hormone which decreases or stops the secretion of growth hormone.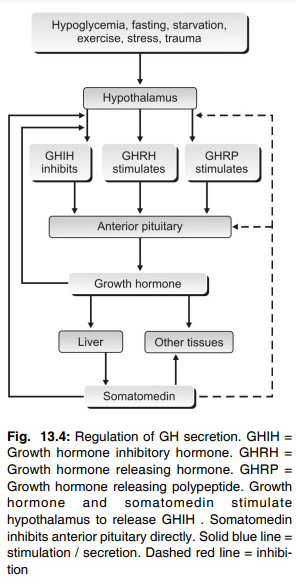
Differentiate somatotropin, somatostatin, and somatomedins.
Somatotropin is the growth hormone (GH) secreted by somatotroph cells of the anterior pituitary.
Somatostatin is the growth hormone inhibiting hormone released from the hypothalamus and also found in nerve endings of the brain, cells of the antrum of the stomach, and in cells of pancreatic islets of Langerhans.
Somatomedins are growth factors, synthesized and released from the liver (mainly), kidneys, muscle, etc. in response to growth hormones and play a role in skeletal growth mainly.
Why GH is known as a protein sparer?
It decreases protein and amino acid catabolism by increasing fat catabolism. This is why it is known as a “protein sparer”.
Why does the growth stop after adolescence?
At the time of adolescence, there is a fusion between the shaft and each end of the epiphysis and thus GH cannot promote the increase of growth of long bone at the epiphyseal endplate. This results in no growth of long bones after adolescence.
What are the actions of follicle-stimulating hormone (FSH)?
In females: FSH causes the development of the Graafian follicle and activates the theca cells in the follicle to secrete estrogen.
In males: It acts along with testosterone to accelerate the process of spermiogenesis.
What are the actions of the luteinizing hormone (LH)?
In females: LH causes maturation of the vesicular follicle into the Graafian follicle along with FSH. It also causes ovulation and is responsible for the formation and secretory activity of the corpus luteum.
In males: This hormone is known as interstitial cell-stimulating hormone (ICSH) because it stimulates the interstitial cells of Leydig in the testes and causes the secretion of testosterone.
What are the actions of prolactin?
Prolactin acts on the mammary gland and prepares it for the production and secretion of milk.
What is β-lipotropin?
It is a polypeptide hormone found recently to be secreted from the anterior pituitary. It mobilizes fat from adipose tissue and promotes lipolysis. It also forms the precursor of endorphins.
Name the hormones of the posterior pituitary.
- Antidiuretic hormone (ADH)
- Oxytocin.
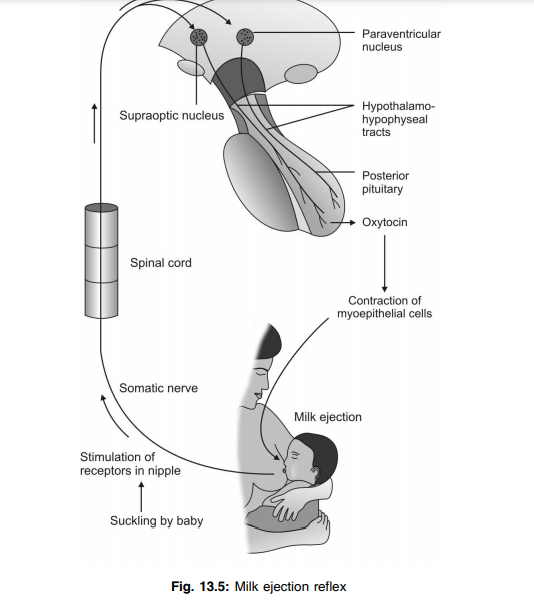
What is the source of secretion of posterior pituitary hormones?
Posterior pituitary hormones are secreted from the hypothalamus. ADH is secreted mainly from the supraoptic nucleus and oxytocin is secreted mainly from the paraventricular nucleus of the hypothalamus.
How do ADH and oxytocin reach the posterior pituitary from the hypothalamus?
ADH and oxytocin, which are secreted from hypothalamic nuclei, reach the posterior pituitary through the nerve fibers of the hypothalamic hypophyseal tract.
What are the actions of ADH?
- It increases the water reabsorption from the distal convoluted tubule and collecting duct and helps in the final concentration of urine
- In higher doses, ADH causes vasoconstriction and increases blood pressure.
Why ADH is called so?
Since this hormone prevents diuresis by reabsorption of water from the distal convoluted tubule and collecting duct, it is called antidiuretic hormone (ADH).
How is ADH secretion regulated?
ADH secretion is regulated by the volume and osmolar concentration of ECF. ADH secretion is stimulated by a decrease in ECF volume and an increase in the osmolar concentration of ECF.
Which are the sites of action of oxytocin?
Mammary glands and uterus.
What is the action of oxytocin on mammary glands?
Oxytocin causes the ejection of milk by contracting the myoepithelial cells of mammary glands.
What is the milk ejection reflex? Why is it called neuroendocrine reflex?
When the infant suckles the mother’s nipple, the impulses produced from the touch receptors on and around the nipple pass through somatic afferent nerve fibers and reach the paraventricular and supraoptic nuclei of the hypothalamus via the cerebral cortex. Now, oxytocin is released into the blood. When the hormone reaches the mammary glands, it causes the ejection of milk. As this reflex is initiated by nervous factors and completed through hormonal action, it is called the neuroendocrine reflex. During this reflex, a large quantity of oxytocin is secreted by a positive feedback mechanism.
What is the action of oxytocin on the pregnant uterus?
Oxytocin causes contraction of the uterus and helps in the expulsion of the fetus during labor. Due to the movement of the fetus through the cervix during the onset of labor, the receptors on the cervix are stimulated and discharge the impulses. These impulses are carried to the cerebral cortex by somatic nerve fibers. The cerebral cortex sends impulses to the hypothalamus causing the release of oxytocin into the blood. And oxytocin enhances labor by causing contraction of the uterus. This is a neuroendocrine reflex. During labor, a large quantity of oxytocin is released by means of a positive feedback mechanism.
What is the action of oxytocin on the nonpregnant uterus?
On the nonpregnant uterus, oxytocin increases uterine contractions during sexual intercourse and facilitates the transport of sperm through the uterine cavity towards the fallopian tube.
What is gigantism?
An abnormal increase in the height of the body in children due to hypersecretion of growth hormone (before the closure of epiphysis) is called gigantism.
What is acromegaly?
Acromegaly is the enlargement, thickening, and broadening of bones due to the hypersecretion of growth hormone in adults (after the closure of epiphysis).
What are the important features of acromegaly?
- Facial features:
Acromegalic face or guerrilla face with protrusion of supraorbital ridges, broadening of the nose, thickening of lips, wrinkles on the forehead, and protrusion of lower jaw (prognathism) - Enlargement of hands and feet with kyphosis
- Bulldog scalp and overgrowth of body hair
- Enlargement of visceral organs
- Hyperactivity of other endocrine glands
- Hyperglycemia and glycosuria resulting in diabetes mellitus
- Hypertension
What is acromegalic gigantism?
If the hypersecretion of growth hormone starts in children resulting in gigantism and if it continues after puberty leading to acromegaly, the condition is known as acromegalic gigantism.
What is Cushing’s disease?
It is a disease characterized by obesity. It is due to the hypersecretion of ACTH.
What is dwarfism?
The stunted growth in children due to lack of secretion of growth hormone is known as dwarfism.
What are the important features of dwarfism?
Stunted growth is the prominent feature of dwarfism. The different parts of the body are almost proportionate. Only the head becomes slightly longer. All other functions including mental activity are normal.
What is Laron dwarfism?
The stunted growth in children because of the lack of somatomedin is known as Laron dwarfism. The secretion of growth hormone is normal.
What is psychogenic dwarfism?
Dwarfism due to exposure to extreme emotional deprivation or stress is called psychogenic dwarfism.
What are the important features of acromicria?
- Atrophy and thinning of hands and feet
- Hypothyroidism
- Hyposecretion of adrenocortical hormones
- Lethargy and obesity
- Loss of sexual functions.
What is Simmond’s disease or pituitary cachexia?
It is a pituitary disease that occurs mostly in panhypopituitarism (hyposecretion of all the anterior pituitary hormones due to atrophy or degeneration of the gland).
What are the features of Simmond’s disease?
- Rapid development of senile decay and appearance of old age
- Loss of hair and teeth
- The skin over the face becomes dry and wrinkled.
What is Laurence-Moon-Biddle syndrome?
It has the following characteristics:
- Physical and mental retardation in growth
- Subnormal intelligence.
- Infantile gonads.
- Obesity with polydactylism
- Retinitis pigmentosa
All these are due to the hypofunction of the pituitary gland as a result of the tumor of chromophobe cells or lesions in the hypothalamus in the young.
Name the nuclei secreting ADH and Oxytocin.
- Supraoptic nuclei – ADH
- Paraventricular nuclei – Oxytocin.
What is the syndrome of inappropriate hypersecretion of antidiuretic hormone (SIADH)?
SIADH is a disease due to the excessive secretion of ADH.
What are the features of SIADH?
- Decrease in urine output
- Increased water retention and ECF volume
- Secondary increase in urine output with more sodium ions
- Decreased sodium concentration in ECF
- Convulsions and coma in severe condition.
What is diabetes insipidus?
Excessive excretion of water through the urine due to lack of ADH is known as diabetes insipidus.
Name the hormones secreted by the thyroid gland.
- Triiodothyronine (T3)
- Tetraiodothyronine (T4 or thyroxine)
- Calcitonin.
Which is more potent, T3 or T4? Why it is so?
T3 is more potent than T4 because T3 is found freely in the plasma and can act immediately. But T4 is bound with plasma proteins, so it takes time for it to be released and then to act.
What are the substances necessary for the synthesis of thyroid hormones?
- Amino acid tyrosine
- Inorganic ion iodine.
How much iodine is required for the synthesis of the normal quantity of thyroid hormones?
One mg of iodine per week or 50 mg per year.
Name the stages in the synthesis of thyroid hormones.
The following are the stages in the synthesis of thyroid hormones
- Thyroglobulin synthesis
- Iodide trapping and iodide pump
- Oxidation of iodide into elemental iodine
- Iodination of tyrosine
- Coupling reactions.
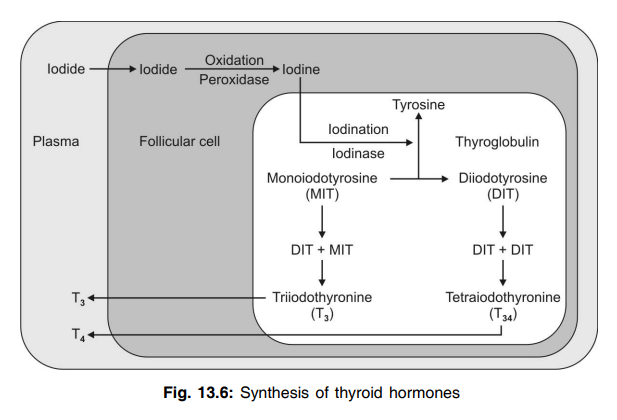
What are the enzymes involved in the synthesis of thyroid hormones?
- Peroxidase converts iodide into elemental iodine
- Iodinase accelerates the iodination of tyrosine.
What is thyroglobulin?
Thyroglobulin is a large glycoprotein secreted by the endoplasmic reticulum and Golgi apparatus of follicular cells and stored in the follicles of the thyroid gland.
How are thyroid hormones released from thyroglobulin?
The follicular cells form pinocytic vesicles around the thyroglobulin–hormone complex. Then the digestive enzymes like proteinase present in lysosomes of the follicular cells digest the thyroglobulin and release the hormones.
How are the thyroid hormones transported in the blood?
Thyroid hormones are transported in the blood in combination with plasma proteins called thyroxine-binding globulin (TBG), thyroxine-binding prealbumin (TBPA), and albumin.
What is the normal plasma level of T3 and T4?
T3 =0.12 μg/dl
T4 =8 μg/dl.
What are the actions of thyroxine on protein metabolism?
Thyroxine increases:
- Translation of RNA
- Transcription of DNA into RNA
- Activity of cellular enzymes
- Mitochondrial activity.
What are the actions of thyroxine on carbohydrate metabolism?
Thyroxine is a diabetogenic hormone.
It increases:
- Glucose absorption from the gastrointestinal tract
- Transport of glucose into the cells
- Breakdown of glycogen (glycogenolysis) into glucose
- Gluconeogenesis.
What are the actions of thyroxine on fat metabolism?
- Mobilizes fat from fat depots and increases free fatty acids in the blood
- Increases deposition of fat in the liver causing fatty liver
- Decreases the level of cholesterol, phospholipids, and triglycerides in plasma.
What are the actions of thyroxine on the cardiovascular system?
Thyroxine increases the overall activity of the cardiovascular system.
- Increases the heart rate
- Increases force of contractions of the heart
- Causes vasodilatation and increases blood flow
- Increases systolic blood pressure and decreases diastolic pressure leading to an increase in pulse pressure.
What is the action of thyroxine on the respiratory system?
Thyroxine increases the rate and force of respiration.
What are the actions of thyroxine on the GI tract?
Thyroxine increases the secretions and movements of the GI tract. It also increases appetite and intake of food.
What are the actions of thyroxine on the central nervous system (CNS)?
Thyroxine is necessary for the development of CNS during fetal life. In adult life, it stimulates and maintains the normal function of CNS.
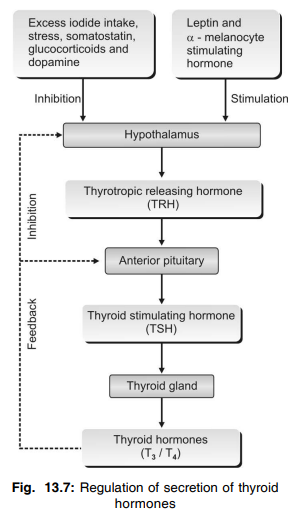
Name the factors increasing the secretion of thyroid hormones.
- Low basal metabolic rate
- Leptin
- Alpha melanocyte-stimulating hormone
Name the factors decreasing the secretion of thyroid hormones.
- Excess iodide intake
- Stress
- Somatostatin.
What are the actions of thyroid-stimulating hormone (TSH)?
TSH increases:
- Number and size of thyroid cells
- Secretory activity of thyroid cells
- Iodide pump and iodide trapping in thyroid cells
- Thyroglobulin secretion
- Iodination of tyrosine and coupling to form thyroid hormones
- Proteolysis of the thyroglobulin by which the thyroid hormones are released into the blood. illustrates the regulation of the secretion of
What are the causes of hyperthyroidism?
- Presence of TSH-like substances in the blood
- Thyroid adenoma
- Grave’s disease.
What are the important features of hyperthyroidism?
- Intolerance to heat
- Increased sweating
- Loss of weight
- Diarrhea
- Muscular weakness
- Nervousness
- Toxic goiter
- Oligomenorrhea or amenorrhea
- Exophthalmos
- Polycythemia
- Tachycardia and atrial fibrillation
- Systolic hypertension
- Cardiac failure
What is exophthalmos?
The protrusion of eyeballs is known as exophthalmos.
What are the causes of exophthalmos in hyperthyroidism?
In hyperthyroidism, there is edema of the retro-orbital tissues and degenerative changes in the extraocular muscles. These two changes are responsible for the protrusion of the eyeballs.
What are the effects of hypothyroidism?
Hypothyroidism leads to myxedema in adults and cretinism in children.
What are the features of myxedema?
- Swelling of the face
- Bagginess under the eyes
- Non-pitting edema
- Atherosclerosis leading to arteriosclerosis and hypertension
- Anemia
- Fatigue and muscular sluggishness
- Somnolence
- Menorrhagia and polymenorrhea in females
- Decreased cardiovascular functions
- Increased body weight
- Constipation
- Mental sluggishness
- Depressed hair growth
- Scaliness of the skin
- Frog like husky voice
- Cold intolerance.
What are the features of cretinism?
- Sluggish movements
- Croaking sound while crying
- Mental retardation
- Stunted growth
- Bloated body
- Protrusion of tongue with dripping of saliva
- Potbelly
All these symptoms give idiotic look to the baby.
What are the major differences between cretinism and pituitary dwarfism?
- In cretinism, there is mental retardation and in dwarfism, the development and functions of the nervous system are normal
- The different parts of the body are disproportionate in cretinism but, in dwarfism, the different parts of the body are proportionate
- In cretinism, the reproductive function is abnormal whereas, it may be normal in dwarfism.
What is a goiter?
Enlargement of the thyroid gland is known as goiter.
How do you classify goiter?
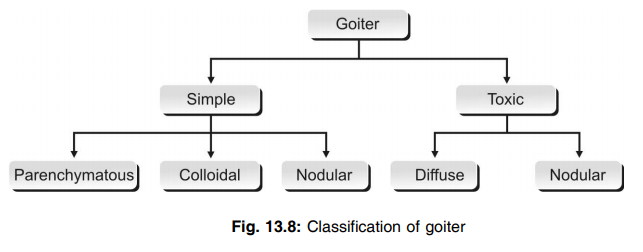
What is a toxic goiter?
Enlargement of the thyroid gland with hypersecretion of hormones is known as toxic goiter.
What is a nontoxic goiter and what are the types of nontoxic goiter?
Enlargement of the thyroid gland with hyposecretion of hormones is known as nontoxic goiter.
It is of two types:
- Endemic colloidal goiter that is due to lack of iodine
- Idiopathic nontoxic goiter that is due to thyroiditis or the presence of goitrogenic factors in foodstuffs.
Name some antithyroid substances.
- Thiocyanate
- Thyourylenes
- Inorganic iodides in high concentration.
Name the thyroid function tests.
- Measurement of T3 and T4 in blood
- Measurement of basal metabolic rate
- Measurement of TRH and TSH in blood.
What is the important function of parathyroid glands in the body?
Parathyroid glands secrete parathormone which is very essential to maintain the blood calcium level.
Why should the blood calcium level be maintained?
Because calcium is very essential for many important activities in the body such as:
- Neuronal activity
- Muscular activity
- Cardiac function
- Secretory activities of the glands
- Coagulation of blood.
What is the normal daily requirement of Calcium and Phosphate and what is their normal blood level?
| Substance | Daily requirement | Blood level |
| Calcium | 0.8 - 1 gm | 9 - 11 mg% |
| Phosphate | 1 - 1.4 gm | 2.5 - 4 mg% |
Name the hormones which regulate Calcium metabolism and their source.
- Vitamin D - Diet mainly and also skin by UV radiation.
- PTH - Chief cells of the parathyroid gland.
- Calcitonin - Parafollicular cells (C-cells) of the thyroid gland.
What are the main signs and symptoms of hypoparathyroidism?
Hypocalcemia, hyperphosphatemia, increase in blood pH, neuromuscular hyperirritability causing tetany.
What are the common signs present in tetany? Explain each of them.
Trousseau’s sign or carpopedal spasm. It is manifested in the upper limb as flexion at the wrist and thumb with hyperextension of remaining fingers called obstetric hand/Accoucheur’s hand or carpopedal spasm. If this is demonstrated by occluding the blood supply to a limb through a sphygmomanometer cuff, it is known as Trousseau’s sign.
Chvostek’s sign: If the skin in front of the ear is tapped, there is a contraction or spasm of facial muscle.
Erb’s sign: It is depicted by the enhanced motor excitability of galvanic current.
Name the hormones involved in the regulation of blood calcium levels.
The hormones involved in the regulation of blood calcium levels are:
- Parathormone secreted from parathyroid glands
- 1, 25 dihydroxy cholecalciferol synthesized in the kidney from vitamin D that is released from the liver
- Calcitonin is secreted from parafollicular cells of the thyroid gland.
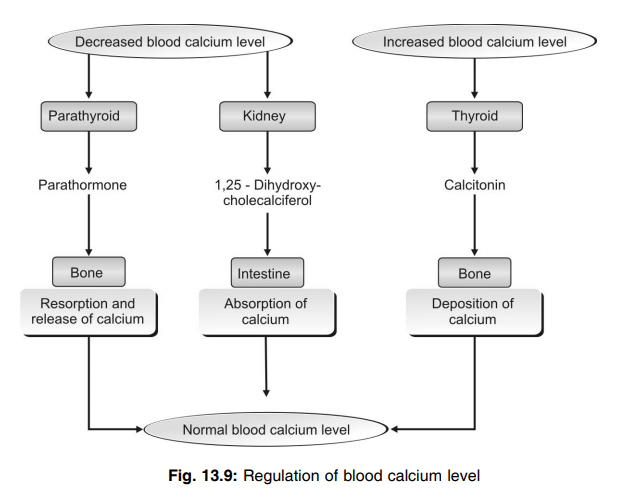
What are the actions of parathormone?
Parathormone increases the blood calcium level by increasing:
- Resorption of calcium from bones
- Reabsorption of calcium from renal tubules
- Absorption of calcium from the intestine by activating vitamin D.
How is 1, 25 dihydroxycholecalciferol (an active form of vitamin D) formed?
1, 25 dihydroxycholecalciferol (an active form of vitamin D) is formed from vitamin D3 (an inactive form of vitamin D), which is also called cholecalciferol. Vitamin D3 is converted into 25 hydroxycholecalciferol in the liver and this is converted into 1, 25 dihydroxycholecalciferol in the kidney in the presence of parathormone.
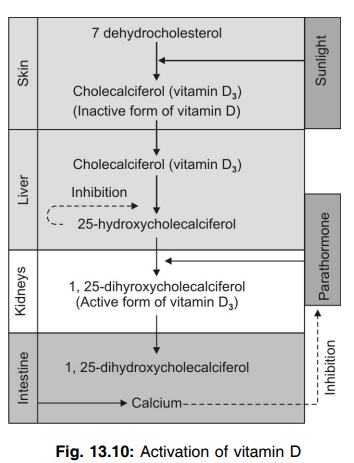
What are the actions of 1, 25 dihydroxycholecalciferol?
It increases:
- Absorption of calcium from the intestine
- Synthesis of ATPase in the intestinal epithelium
- Alkaline phosphatase in the intestinal epithelium.
How is the secretion of parathormone regulated?
By the blood calcium level through a negative feedback mechanism.
What are the actions of calcitonin?
Calcitonin decreases blood calcium levels by:
- Increasing deposition of calcium in bones
- Increasing excretion of calcium through urine
- Decreasing the absorption of calcium from the intestine.
Q.112 What is tetany?
Repeated convulsive muscular contractions, which occur due to hypoparathyroidism and hypocalcemia is known as tetany.
Q.113 What are the important features of tetany?
- Carpopedal spasm
- Laryngeal stridor
- Cardiovascular changes like dilatation of heart, prolonged duration of ST-segment and QT interval in ECG, arrhythmias, hypotension, and heart failure.
Q.114 What are the important features of hypercalcemia?
- Depression of neuronal activities
- Sluggishness of reflex activities
- Reduction in the duration of ST-segment and QT interval in ECG
- Lack of appetite
- Constipation.
Q.115 What are the major types of cells in bone? Mention their functions.
Osteoblasts – concerned with bone formation that involves the formation of bone matrix and deposition of calcium (osteoblastic activity)
Osteocytes – concerned with maintenance of bone
Osteoclasts – concerned with bone resorption that involves the destruction of bone matrix followed by the removal of calcium (osteoclastic activity).
Q.116 What do you mean by osteomalacia, osteoporosis, and osteosclerosis?
Osteomalacia is the adult ricket characterized by:
- Decrease in mineral in bone/unit of bone matrix
- Generally limited to females usually after multiple pregnancy and lactation
Causes:
- Dietary deficiency of vit-D
- Malabsorption of Vit -D
- Chronic renal failure
- Inadequate exposure to sun
Characteristic features:
- Bone pain and tenderness
- Fracture may occur
- Proximal myopathy
- Deformed bone with bowing legs
- Retarded growth In children
- Thickening of wrists and ankle.
Osteoporosis: It is the clinical condition characterized by;
- Increase in all constituents of bone due to an increase in bone resorption and decrease in bone formation.
- Causes
– Postmenopausal women (due to low estrogen level resulted from an increase in sensitivity of PTH to bone)
– Hyperparathyroidism
– Hyperthyroidism
– Calcium deficiency
Osteosclerosis:
Increased calcified bone in patients with metastatic tumors, lead poisoning, and hypothyroidism.
Q.117 What is rickets? What is its cause?
It is a bone disease in children characterized by the collapse of the chest wall and curvature of the spine. It is due to the inadequate mineralization of the bone matrix.
Q.118 What is the endocrine part of the pancreas?
Islets of Langerhans form the endocrine part of the pancreas.
Q.119 Name the types of cells in islets of Langerhans.
- A or alpha cells which secrete glucagon
- B or beta cells which secrete insulin
- D or delta cells which secrete somatostatin
- F or PP cells which secrete pancreatic polypeptide.
Q.120 What are the actions of insulin?
- Insulin is the antidiabetogenic hormone, i.e. it decreases the blood sugar level by acting on carbohydrate metabolism
- It increases synthesis and storage of proteins
- It increases the synthesis and storage of fat
- It promotes the growth of the body along with growth hormones.
Q.121 What are the actions of insulin on carbohydrate metabolism?
Insulin:
- Facilitates the transport of glucose into the cells
- Increases peripheral utilization of glucose
- Increases the conversion of glucose into glycogen in liver and muscle
- Inhibits glycogenolysis
- Inhibits gluconeogenesis. By all these actions, insulin acts as an antidiabetogenic hormone, i.e. it decreases blood sugar level.
Q.122 What is the effect of insulin on growth?
Insulin promotes growth of the body by its anabolic effects on proteins and by its protein-sparing effects.
Q.123 What is Houssay animal? What is its importance?
Houssay animal is the one in which both pancreas and anterior pituitary are removed. This preparation proves the importance of insulin in the growth of the animal along with growth hormones. When growth hormone alone or when insulin alone is administered to a Houssay animal, growth is not accelerated. But, when both growth hormone and insulin are given together, growth is accelerated very much.
Q.124 How is insulin secretion regulated?
Insulin secretion is regulated mainly by blood glucose levels. When the blood sugar level is more, insulin secretion increases. And, when the blood glucose level is less, insulin secretion decreases.
Q.125 Name the stimuli for insulin secretion.
- Increase in blood sugar level
- Increase in amino acid level in blood
- The β ketoacids in blood
- Gastrointestinal hormones like gastrin, secretin, cholecystokinin, and GIP
- Other endocrine hormones like glucagon, growth hormone, and cortisol
- Stimulation of parasympathetic nerve fibers (right vagus) to the pancreas.
Q.126 What are the actions of glucagon?
Glucagon:
- Increases the blood sugar level
- Increases the transport of amino acids into the liver cells leading to gluconeogenesis
- Shows lipolytic and ketogenic actions
- Inhibits gastric secretion and increases bile secretion.
Q.127 How does glucagon increase the blood sugar level?
Glucagon increases the blood sugar level by increasing glycogenolysis and gluconeogenesis.
Q.128 Name the factors which increase the secretion of glucagon.
- Reduction in blood glucose level
- Increase in amino acid level
- Exercise
- Stress
- Some hormones such as gastrin, cholecystokinin, and cortisol.
Q.129 Name the factors which inhibit the secretion of glucagon.
- Increase in blood glucose level
- Somatostatin
- Insulin
- Free fatty acids
- Ketone bodies.
Q.130 What are the sources of secretion of somatostatin?
- Hypothalamus
- D cells present in islets of Langerhans
- D cells present in stomach and upper part of small intestine.
Q.131 What are the actions of somatostatin?
Somatostatin:
- Inhibits the secretion of insulin and glucagon
- Decreases the motility of the stomach and small intestine
- Decreases the secretion of CCK, GIP, and VIP
- Decreases the secretion of growth hormone (hypothalamic somatostatin).
Q.132 What is the action of pancreatic polypeptide?
Pancreatic polypeptide is believed to increase the secretion of glucagon.
Q.133 What is the necessity for regulation of blood sugar levels?
Glucose is the only nutrient that can be utilized by the tissues like the brain, retina, and germinal epithelium of gonads. So, the blood sugar level has to be regulated within normal limits.
Q.134 What is the normal blood sugar level?
Fasting blood sugar = 80 to 90 mg%
Postprandial blood = 120 to 140 mg% sugar
Q.135 How is the blood sugar level maintained?
Blood sugar level is maintained by a regulating mechanism that is operated through the liver and muscle under the influence of insulin and many other hormones like thyroxine, cortisol, glucagon, and adrenaline.
Q.136 What are the hormones that regulate blood glucose levels? Which one is the most important?
Insulin, glucagon, epinephrine, hydrocortisone, ACTH, growth hormone, and thyroxin, out of which insulin is most important.
Q.137 Name the hormones which are antagonistic to the insulin?
GH, thyrotrophic hormone, ACTH, and glucagon.
Q.138 What is the role of the liver in the maintenance of blood sugar levels?
The liver acts as an important glucose buffer system. When blood sugar level increases after meals, the excess glucose is converted into glycogen and stored in the liver. Afterward, when the blood sugar level decreases, liver glycogen is broken into glucose that is released into the blood. These actions are brought about under the influence of insulin and glucagon.
Q.139 What is diabetes mellitus?
Persistent increase in blood sugar level with other clinical manifestations is known as diabetes mellitus.
Q.140 What are the types of diabetes mellitus?
- Type I diabetes mellitus or insulin-dependent diabetes mellitus (IDDM) – due to deficiency of insulin
- Type II diabetes mellitus or non-insulin-dependent diabetes mellitus (NIDDM) – due to the absence or reduced number of insulin receptors in the cells of the body.
Q.141 What is juvenile diabetes?
Juvenile diabetes is a type of IDDM that occurs in infancy or childhood.
Q.142 What are the causes of Type I diabetes mellitus?
- Degeneration of beta cells in islets of Langerhans
- Destruction of beta cells by viral infection
- Congenital disorder of beta cells
- Autoimmunity against beta cells.
Q.143 What are the causes of Type II diabetes mellitus?
- Hereditary disorders
- Endocrine disorders.
Q.144 Name the endocrine disorders in which diabetes mellitus is common.
Gigantism, acromegaly and Cushing’s syndrome.
Q.145 What are the features of diabetes mellitus?
- Glucosuria
- Osmotic diuresis
- Polyuria
- Polydipsia
- Polyphagia
- Asthenia
- Acidosis
- Acetone breathing
- Kussmaul breathing
- Circulatory shock
- Coma.
Q.146 What is the cause of hyperinsulinism?
Tumor of beta cells of islets of Langerhans.
Q.147 What do you understand by the glucose tolerance test (GTT)?
It is a common clinical laboratory method to investigate the cases of diabetes mellitus and certain other conditions. The patient is kept on about 300 gm carbohydrate diet daily for 3 days. Fasting sample is collected in the morning after which the patient is administered glucose by oral route (1 gm/ kg of b.w). The blood and urine samples are collected ½, 1, 1 ½ and 2 hours interval. The blood glucose values are estimated and urine is tested for the presence of glucose. The values of glucose are plotted in a graph paper to obtain a characteristic graph.
Q.148 What are the types of GTT graph curves?
Three types:
- Normal curve,
- Lag curve and
- Diabetic curve. The lag curve is seen in early diabetic patients.
Q.149 Differentiate between hyperglycemic and hypoglycemic coma?
| Parameter | Hyperglycemic coma | Hypoglycemic coma |
| Cause | Due to an increase in blood glucose level (>400 mg%) | Due to the fall of blood glucose level (< 40 mg%) and more severe. |
| Rate of onset | Slow | Rapid |
| Signs and symptoms | ||
| Breathing | Deep and rapid breathing | Labored breathing called air hunger or Kussmaul breathing. |
| Sweating | Absent | Usually marked. |
| Hydration | Marked dehydration | Normal |
| Urine exam | Marked glycosuria | Not specific, and ketonuria |
Q.150 What are the features of hyperinsulinism?
- Hypoglycemia
- Manifestations of CNS like nervousness, tremor, and excessive sweating. If not treated immediately, hyperinsulinism leads to clonic convulsions and unconsciousness leading to coma.
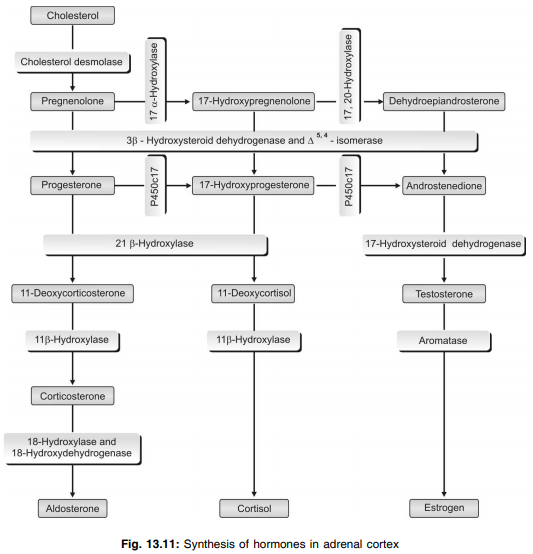
Q.151 Name the hormones secreted by the adrenal cortex.
The adrenal cortex secretes three groups of hormone:
- Mineralocorticoids – aldosterone and 11 deoxycorticosterone
- Glucocorticoids – cortisol and corticosterone
- Sex hormones (androgens) – dehydroepiandrosterone, androstenedione and testosterone and small quantity of estrogen and progesterone.
Q.152 What are the hormones secreted by different parts of the adrenal cortex?
Mineralocorticoids are secreted by zona glomerulosa.
Glucocorticoids are secreted mostly by zona fasciculata and a small quantity is secreted by zona reticularis.
Sex hormones are secreted mostly by zona reticularis and a small quantity by zona fasciculata.
Q.153 What do you mean by primary aldosteronism (Conn’s syndrome)?
It is due to aldosterone oversecretion mainly due to adenoma in the adrenal cortex which ultimately results:
- Sodium retention and K+ depletion.
- Alkalosis—that causes muscular weakness and tetany.
- Hypertension and congestive heart failure without edema.
- Polyuria and polydipsia.
Q.154 What is secondary aldosteronism?
When aldosterone secretion is increased not due to adrenal cortical change but due to other factors like severe hemorrhage, diarrhea, dehydration, sweating, nephrosis, congestive heart failure it is known as secondary aldosteronism.
Q.155 What is the glucose fever?
The patient with adrenal cortex insufficiency if suffers from circulatory collapse, glucose infusion may cause high fever known as glucose fever.
Q.156 What do you mean by Addisonian or adrenal crisis?
This is an acute form of adrenal cortex insufficiency which occurs after the removal of the adrenal cortex or withdrawal of therapeutically administered glucocorticoids or the patients with reduced basal secretion of cortisol and exposed to a sudden stress or infection.
Q.157 In Cushing’s syndrome why the patient appears a moon like face and buffalo like hump?
In Cushing syndrome, there is increased secretion of glucocorticoids which promote the deposition of fat in unusual sites on the body to result moon like face and buffalo hump.
Q.158 What is Conn’s syndrome?
Primary aldosteronism or Conn’s syndrome is the clinical condition due to excess aldosterone secretion due to tumor or hyperplasia of Z.
Glomerulosa of the adrenal cortex which is characterized by:
- Muscular weakness (due to prolonged hypokalemia)
- Hypokalemic nephropathy
- Increase in plasma Na+,
- Increase in plasma aldosterone level without oedema due to aldosterone escape
- Increase in urinary aldosterone level
- Decrease in plasma K+
- Decrease in plasma renin
- Albuminuria
Q.159 What are the actions of aldosterone (mineralocorticoids)?
Aldosterone increases:
- Reabsorption of sodium ions
- ECF volume
- Blood pressure i
- Excretion of potassium
- Excretion of hydrogen ions
- Reabsorption of sodium from sweat and salivary glands
- Absorption of sodium from the intestine.
Q.160 What are the stimuli for the secretion of aldosterone?
- Increase in potassium ion concentration in ECF
- Decrease in sodium ion concentration in ECF
- Decrease in ECF volume
- ACTH.
Q.161 How is aldosterone secretion regulated?
An increase in potassium ion concentration in ECF directly acts on the zona glomerulosa of the adrenal cortex and increases the secretion of aldosterone. Reduction in sodium concentration and volume of ECF causes the release of renin from the juxtaglomerular apparatus of the kidney. Renin converts angiotensinogen into angiotensin I. Angiotensin I is converted into angiotensin II by converting enzyme. Angiotensin II stimulates zona glomerulosa of the adrenal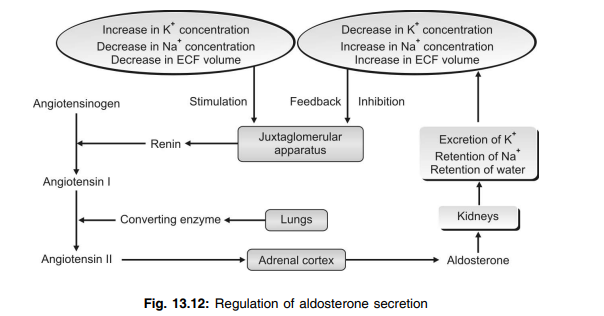
Q.162 What are the actions of cortisol on carbohydrate metabolism?
Cortisol is a diabetogenic hormone and it increases the blood sugar level by:
- Increasing gluconeogenesis.
- Decreasing glucose uptake and utilization by peripheral cells (anti-insulin action).
Q.163 What are the actions of cortisol on protein metabolism?
Cortisol causes catabolism of proteins by:
- Increasing the breakdown of proteins
- Decreasing the synthesis of proteins.
Q.164 What are the actions of cortisol on fat metabolism?
Cortisol increases:
- Mobilization and redistribution of fats
- Fatty acids in the blood
- Utilization of fat for energy.
Q.165 What are the actions of cortisol on mineral metabolism?
Cortisol increases the retention of sodium and water and excretion of potassium.
Q.166 What are the non-metabolic actions of cortisol?
- On blood cells – cortisol decreases the circulating eosinophils, basophils, and lymphocytes and increases neutrophils, red blood cells, and platelets
- On vascular system – cortisol is essential for vasoconstrictor action of adrenaline and noradrenaline
- On the nervous system – it is essential for the normal functioning of the nervous system
- Permissive action – it is essential for the execution of actions of some hormones
- Antistressor effects – it increases the resistance to stress
- Antiinflammatory effects – cortisol prevents inflammatory changes in cells caused by injury or infection
- Antiallergic actions – it prevents reactions in allergic conditions
- Immunosuppressive effect – cortisol suppresses the immune system.
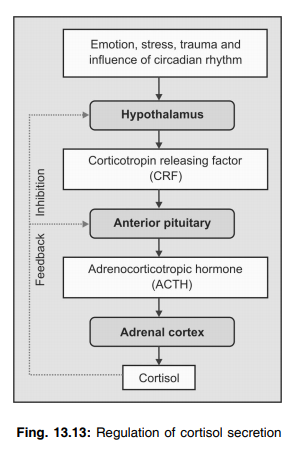
Q.167 How is the secretion of cortisol regulated?
By negative feedback mechanism through ACTH secreted by anterior pituitary and corticotropin-releasing hormone by hypothalamus
Q.168 What are the actions of adrenocorticotropic hormone (ACTH)?
- Adrenal actions (on adrenal cortex):
- Maintains the structural integrity and vascularization of gland
- Converts cholesterol into pregnenolone from which the glucocorticoids are synthesized
- Causes release of glucocorticoids
- Prolongs the glucocorticoid action.
- Non-adrenal actions:
- Mobilizes the fats from fat tissues
- Melanocyte stimulating effect.
Q.169 What are the effects of hyperactivity of the adrenal cortex?
- Cushing’s syndrome
- Hyperaldosteronism and adrenogenital syndrome.
Q.170 List the features of Cushing’s syndrome.
- Abnormal distribution of body fat resulting in moon face, torso, buffalo hump, and pot belly
- Purple striae
- Thinning of extremities
- Thinning of skin and subcutaneous tissues
- Darkening of skin in neck
- Hyperpigmentation
- Facial redness
- Facial hair growth
- Muscular weakness
- Bone resorption and osteoporosis
- Hyperglycemia
- Hypertension
- Immunosuppression
- Poor wound healing.
Q.171 What is hyperaldosteronism?
Excessive secretion of aldosterone is known as hyperaldosteronism.
Q.172 Name the types and causes of hyperaldosteronism.
- Primary hyperaldosteronism (Conn’s syndrome) – due to tumor in zona glomerulosa
- Secondary hyperaldosteronism – extra adrenal causes like congestive cardiac failure, nephrosis, toxemia of pregnancy and cirrhosis of liver.
Q.173 What are the features of hyperaldosteronism?
- Increase in ECF volume and blood volume
- Hypertension
- Polyuria
- Polydipsia
- Muscular weakness
- Metabolic alkalosis.
Q.174 What is an escape phenomenon in primary hyperaldosteronism?
In primary hyperaldosteronism, there is retention of sodium and water leading to an increase in ECF volume. When ECF volume increases to a certain level, atrial natriuretic peptide (ANP) is released from atrial muscles. ANP causes excretion of sodium and water from the kidney in spite of increased aldosterone secretion. This is known as the escape phenomenon. Because of this, edema is not developed in primary hyperaldosteronism.
Q.175 What is adrenogenital syndrome?
Adrenogenital syndrome is the condition with increased activity of sex organs due to excessive secretion of sex hormones from the adrenal cortex.
Q.176 What is virilism? What are its features?
Virilism is the development of male secondary sexual characters in females due to increased secretion of androgens.
Features:
- Increase in muscle bulk
- Deepening of voice
- Amenorrhea
- Enlargement of clitoris
- Male type of hair growth.
Q.177 What are the features of adrenogenital syndrome in males?
- Feminization
- Gynecomastia (enlargement of breast)
- Atrophy of testes
- Loss of interest in women.
Q.178 What are the effects of hypoactivity of the adrenal cortex?
- Chronic adrenal insufficiency or Addison’s disease
- Acute adrenal insufficiency or Addisonian crisis or adrenal crisis
- Congenital adrenal hyperplasia.
Q.179 What is the cause of Addison’s disease?
Failure of the adrenal cortex to secrete corticosteroids.
Q.180 What are the features of Addison’s disease?
- Hyperpigmentation of skin and mucus membrane
- Muscular weakness
- Dehydration
- Hypotension
- Decreased cardiac output
- Hypoglycemia
- Nausea, vomiting, and diarrhea
- Susceptibility to infections
- Inability to withstand stress.
Q.181 What is the Addisonian crisis? When does it occur?
The sudden collapse of the person due to severe and acute need for a large quantity of glucocorticoids is known as an Addisonian crisis.
- It occurs in conditions like exposure to even mild stress.
- Hypoglycemia due to fasting
- Trauma
- Surgical operation
- Sudden withdrawal of glucocorticoid treatment.
Q.182 What is congenital adrenal hyperplasia?
It is the disease that develops due to the congenital absence of enzymes necessary for the synthesis of cortisol, particularly 21– hydroxylase. Since cortisol secretion is decreased, secretion of ACTH increases by feedback mechanism. ACTH acts on the adrenal glands and increases the number of cells leading to hyperplasia. Since, cortisol cannot be synthesized due to lack of enzymes, the synthesis of androgens increases leading to sexual abnormalities.
Q.183 What are the hormones secreted by adrenal medulla?
Adrenal medullary hormones are collectively known as catecholamines. Catecholamines are adrenaline or epinephrine, noradrenaline or norepinephrine and dopamine.
Q.184 What is General Adaptation Syndrome? What is it’s role in combating stress?
The general manifestation of stress is called the general adaptation syndrome which is contributed by sympatho-adrenal medullary system in which adrenal medullary hormones contribute to the Fight or Flight response by following ways:
- Allows more light to enter into eyes by relaxing accommodation and producing pupillary dilatation.
- Provides better perfusion of vital organs and muscles.
- Shortens the bleeding time (if wounded).
- Reinforcing the alert and arousal state by decreasing the threshold in reticular formation.
- Increasing glycogenolysis in liver and lipolysis in adipose tissue to increase energy supply.
Q.185 What is general adaptive syndrome?
General manifestation of stress is called general adaptive syndrome. It occurs in 3 stages:
- Stage of alarm—No adaptation takes place.
- Stage of resistance—Optimum adaptation occurs due to the interaction of the adrenal cortex and adrenal medulla.
- Stage of exhaustion—Due to continued stress.
Q.186 What is the mode of action of catecholamines?
The actions of catecholamines are exerted through some receptors present in the target organs called adrenergic receptors.
Q.187 What are the types of adrenergic receptors?
- Alpha adrenergic receptors, which are divided into alpha1 and alpha2 receptors
- Beta adrenergic receptors, which are divided into beta1and beta2 receptors.
Q.188 What is the difference in the response of adrenergic receptors to adrenaline and noradrenaline?
Alpha receptors give more response to noradrenaline than for adrenaline. Beta1 receptors have equal response to both adrenaline and noradrenaline. Beta2 receptors give more response to adrenaline than to noradrenaline.
Q.189 What are the actions of adrenaline and noradrenaline on metabolism?
Adrenaline has metabolic actions but noradrenaline does not have metabolic effects. Adrenaline is a calorigenic hormone and it increases the basal metabolic rate. It increases blood glucose level by increasing glycogenolysis. On fats, it causes the mobilization of fatty acids from adipose tissues.
Q.190 What is the action of adrenaline and noradrenaline on blood?
Adrenaline increases the red blood cell count and hemoglobin content of the blood by causing contraction of the spleen. Noradrenaline does not show this action.
Q.191 What is the action of adrenaline and noradrenaline on heart?
Adrenaline increases the overall activity of the heart, i.e. it increases the rate and force of contraction and excitability of the cardiac muscle. Noradrenaline has mild effect on heart.
Q.192 What are the actions of adrenaline and noradrenaline on blood vessels?
Noradrenaline has got stronger action on blood vessels. It causes vasoconstriction throughout the body thus, increasing the total peripheral resistance. So noradrenaline is called general vasoconstrictor. Adrenaline also causes vasoconstriction. But it causes the dilatation in some areas like skeletal muscle, liver, and heart. So, adrenaline decreases the total peripheral resistance.
Q.193 What are the actions of adrenaline and noradrenaline on blood pressure?
Adrenaline increases systolic blood pressure by increasing the rate and force of contraction of the heart and cardiac output. But, it decreases diastolic blood pressure by reducing the total peripheral resistance. Noradrenaline increases diastolic blood pressure to a greater extent because of its general vasoconstrictor action that increases the total peripheral resistance. It increases systolic pressure to a lesser extent.
Q.194 What are the actions of adrenaline on the respiratory system?
Adrenaline increases the rate and force of respiration. When injected, it produces adrenaline apnea. It also causes bronchodilatation.
Q.195 What are the stimuli for the secretion of catecholamines?
Exposure to stress, cold, and hypoglycemia are the stimuli for the secretion of catecholamines.
Q.196 What is pheochromocytoma?
Pheochromocytoma is a condition characterized by hypersecretion of catecholamines. It is caused by a tumor of chromophil cells in the adrenal medulla. Hypertension, hyperglycemia, and glucosuria are the important features of this condition.
Q.197 What is the function of the pineal gland?
The pineal gland secretes the hormonal substance melatonin. In some animals, melatonin stimulates gonads and in some animals, it inhibits the gonads. In humans, it inhibits the onset of puberty by inhibiting the gonads.
Q.198 What are the functions of the thymus gland?
- It plays an important role in cellular immunity by processing the T lymphocytes
- It secretes thymosin (that helps in the proliferation of T lymphocytes) and thymin (that suppresses neuromuscular activity by inhibiting the release of acetylcholine).
Q.199 Mention the hormones secreted by the kidney.
- Erythropoietin
- Thrombopoietin
- Renin
- 1, 25 dihydroxy cholecalciferol
- Prostaglandins.
Q.200 Name the hormones secreted by heart. What is their action?
Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) are the hormones secreted by the heart. These hormones:
- Increase sodium excretion through urine (escape phenomenon)
- Decrease blood pressure.
Q.201 What are local hormones? What are the types of local hormones?
Local hormones are the hormonal substances, which execute their actions in the same area of secretion or in the immediate neighborhood.
Types:
- Hormones synthesized in tissues
- Hormones synthesized in the blood.
Q.202 Name the local hormones synthesized in the tissues.
- Prostaglandins and related substances like thromboxanes, prostacyclin, leukotrienes, and lipoxins.
- Other local hormones like acetylcholine, serotonin, histamine, substance P, heparin, and GI hormones.
Q.203 Name the local hormones synthesized in the blood.
Serotonin, angiotensin, and kinins.
Q.204 What is APUD cells?
GIT contains some cells which can take up amine precursors and decarboxylate them to convert it as amines. Therefore these cells are known as Amino Precursor Uptake and Decarboxylation (APUD) cells. Similar types of cells are also present in the brain normally and also in some cases of lung cancer. G cell is one type of APUD cells.
Read Also
Delta 8 Wax Dabs are for sale online at D8 Super Store. The wax is derived from legal hemp and comes in different forms and flavors. The product is marketed as safe and beneficial, with FDA approval. Customers can enjoy a 15% discount on their first order of concentrated CBD products.
Also read: Physiology Questions & Answers

Comments (0)