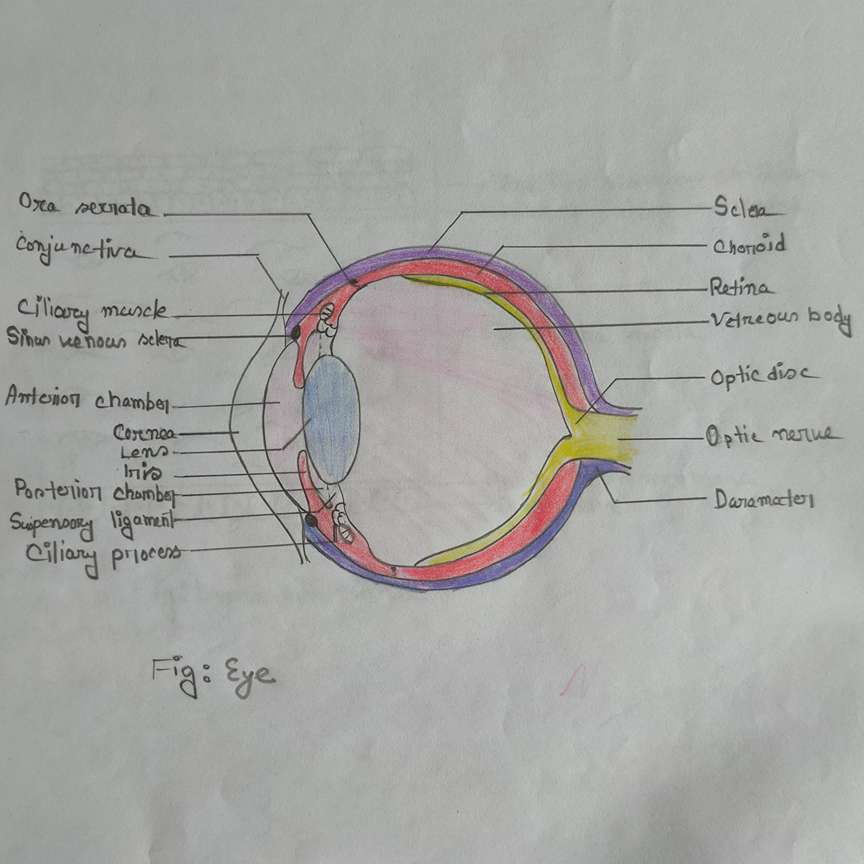
Eyeball
Layer of eyeball
- Outer fibrous coat
Contain sclera and cornea
- Middle vascular coat/uveal tract
Consists of
Choroid
Ciliary body
Iris
- Inner nervous coat
Consists of cornea
Refractive Media:
The structures which are responsible for the transmission of light up to the retina are called refractive media.
Components of refractive media
(From outer to inner)
- Cornea
- Aqueous humor
- The lens
- The vitreous body
Sclera:
* The junction between the cornea and sclera is called the sclerocorneal junction also known as the limbus
* Just posterior to the limbus, all recti muscles are inserted.
* The sclera is continuous anteriorly with the cornea at the sclerocorneal junction (limbus).
* Deep part of the limbus contains a canal called the canal of Schlemm, which drains aqueous humor into the anterior ciliary vein.
Outer Surface:
The outer posterior surface of the sclera which cannot be seen while looking through the eye is covered by the tenon’s capsule (Bulbar fascia).
Similarly, the outer anterior surface of the sclera which can be seen through the eye is covered by conjunctiva.
Inner Surface:
The inner surface of the sclera is brown as related to the choroid and grooved by ciliary nerves and vessels.
Conjunctiva:
Conjunctiva not only covered the anterior of the sclera but only covered the inner surface of the upper eyelid and lower eyelid.
Two types of conjunctiva
- Bulbar conjunctiva:
Around the anterior aspect of the sclera
- Palpebral conjunctiva:
Around the inner aspect of the eyelid
Conjunctiva is composed of non-keratinized stratified squamous epithelium.
Conjunctiva is vascular with a lot of microvessels.
But the cornea is avascular.
Structure piercing the sclera
- Optic nerve
- Ciliary nerves and arteries
- Anterior ciliary arteries
- Choroid veins or venue vorticosae
Note:
|
The sclera is almost avascular.
However, the loose connective tissue between the conjunctiva and sclera called episclera is vascular.
|
|
The cornea is avascular. It is nourished by
- Aqueous humor
- Lacrimal fluid
|
|
Similarly, the lens is also avascular.
It is nourished by aqueous humor.
|
The shape of the eyeball is maintained by
Sclera and vitreous body |
Cornea:
Sclera is replaced by the cornea over the anterior 1/6 part of the eyeball.
* The junction between the sclera and cornea is called the limbus/sclerocorneal junction.
* Highly sensitive and supplied by the ophthalmic nerve and the short ciliary nerve (arises from ciliary ganglion).
Histology of cornea:
(From outside to inward)
-
Corneal epithelium:
Consists of non-keratinized stratified squamous epithelium
- Bowman’s membrane / Anterior limiting membrane
- Substantial propria (Corneal stroma)
- Descemet’s membrane / Posterior limiting membrane
- Endothelium:
Simple squamous epithelium
Middle Vascular coat or Uveal tract:
Consists of most of the blood vessels of the eyeball.
Choroid:
* It is a thin brown pigmented layer.
* Anteriorly connected to the ciliary body at the level of Ora Serrata of the retina.
* The outer surface contains ciliary vessels and nerves.
Note:
| The inner surface of the choroid is firmly attached to the retina and nourishes the rods and cones of the retina by diffusion. |
|
Choroid is dark brown in color so that it can absorb light, decreasing the reflection of light.
|
Ciliary body:
It is continuous anteriorly with the iris and posteriorly with the choroid.
Part of the ciliary body:
1) Ciliary processes
- Which provides attachment of the suspensory ligament of the lens
- The suspensory ligament provides attachment to the lens and helps in accommodation for near vision.
- The ciliary processes are a complex of capillaries that secret aqueous humor.
2) Ciliary muscle (smooth/unstriped muscle) consists of two fibers.
- Outer radial fibers
- Inner circular fibers
Ciliary muscles are supplied by parasympathetic fibers arising from the Edinger-Westphal nucleus through the ciliary ganglion.
Iris:
From the anterior part of the middle vascular layer of the eyeball.
An opening in its center is called the pupil.
* By adjusting the size of the pupil, it controls the amount of light entering the eye and thus behaves like an adjusting diaphragm.
* It is placed between the cornea and the lens, thus dividing the eye's anterior segment into anterior and posterior chambers containing aqueous humor.
* The color of the iris is determined by the number of pigment cells. Iris is seen as blue in the absence of pigment cells.
Iris consists of two smooth muscles.
- Sphincter pupillae of iris-
Made of circular fibers
- Dilator pupillae of iris -
Made of radial fibers.
| Intraocular Muscle |
Nerve supply |
Function |
| Ciliary muscle |
Oculomotor (parasympathetic) through ciliary ganglion |
Control shapes of lens
Accommodation |
| Sphincter pupillae of iris |
Oculomotor (parasympathetic) through ciliary ganglion |
Constricts pupil |
| Dilator pupillae of iris |
Cervical sympathetic fibers that have comes along the internal carotid artery
|
Dilates the pupil |
Inner nervous coat of the eyeball (Retina):
Surfaces:
- The outer surface of the retina
Formed by pigment cells & is attached to the choroid.
- The inferior surface of the retina
Contact with the hyaloid membrane (of the vitreous body).
Parts of the retina:
1) Optic part of the retina:
* Extension from the optic disc to the posterior end of the ciliary body.
* Contain nervous tissue & sensitive to light
2) Ciliary part of the retina:
* Lie above at the level of the ciliary body.
* Non-nervous part and insensitive to light.
3) Iridial part of the retina:
* Non-nervous part and insensitive to light.
* The retina diminishes in thickness from behind forwards. The anterior margin of the optic part of the retina forms an irregular way line called Ora Serrata.
Demarcation created by Ora Serrata:
- Here, the optic part of the retina ends and the ciliary part of the retina begins.
- The Choroid part of the middle vascular layer end and the ciliary body begins.
Beyond the Ora Serrata, the retina is continued forwards as a thin, non-nervous insensitive layer that covers the ciliary body and iris, forming the ciliary and iridial parts of the retina.
Optic Disc & Blind Spot:
* Opposite the entrance of the optic nerve ( inferomedial to the posterior pole) there is a circular area known as the optic disc.
* Physiological cup- a depressed area of the optic disc.
* It contains no rods or cones and is therefore insensitive to light, ie it is the physiological blind spot.
Macula Lutea:
* At the posterior pole of the eye 3mm lateral to the optic disc, there is another depression called macula lutea.
* It is avascular and yellow in color.
* The center of the macula is further depressed to form the fovea centralis.
* It contains the maximum concentration of cones only and is the site of maximum acuity of vision (ability to see fine images).
Rods and cones - light receptors of the eye
- Cones - needed for bright light vision and color vision.
The visual pigment is iodopsin.
- Rods concerned with dim light vision
The visual pigment is rhodopsin.
Rods are absent in fovea centralis.
Ten layers of the retina:
- Outer pigmented layer
- Layer of rods and cones
- External limiting membrane
- Outer nuclear layer
- Outer plexiform layer
- Inner nuclear layer (bipolar cells)
- Inner plexiform layer
- Ganglion cell layer
- Nerve fiber layer
- The internal limiting membrane
Blood supply of retina:
By the central artery of the retina (end artery), a branch of the ophthalmic artery of the internal carotid artery.
Venous drainage:
The radicle of retinal veins - a central vein of the retina - cavernous sinus
| Artery supply of retina: |
|
The outer five layers of the retina are nourished by the diffusion from the capillaries of the choroid artery.
The inner five layers up to bipolar cells are supplied by the central artery of the retina.
|
|
The central artery of the retina on the reaching optic disc is divided into upper and lower branches.
- Superior nasal artery
- Superior temporal artery
- Inferior nasal artery
- Inferior temporal artery
|
Artery supply of eyeball:
The eyeball is supplied by branches from the ophthalmic artery.
Lens:
The lens is the transparent concave structure that is placed between the anterior & posterior segments of the eye.
Lens flexibility and its curvature is controlled by the ciliary muscle through the suspensory ligament of the lens.
Thus, by changing the focal length, the lens can focus on objects at various distances
Mechanism of lens functioning
(For far vision)
Parallel rays from the distant object
|
Relaxation of the ciliary muscle
|
Contraction of the suspensory ligament of the lens
|
Flattened the lens (decreases in the anteroposterior diameter of the lens) ie decreases the lens curvature
|
Decreases the refractive index
|
Less convergence of parallel rays
|
Focus the light on the retina for near vision
(For near vision)
Divergent rays coming from near objects
|
Contraction of the ciliary muscle
|
Relaxation of suspensory ligaments of lens
|
Increase in the curvature of the lens (ie increase in the anteroposterior diameter of the lens)
|
Highly converge the divergent ray coming from a near object
|
Focus the light on the retina
Note:
The function of the biconcave lens is to converge the rays of light.
Refractory errors of the eyeball:
1) Myopia (Short-sightedness)
Features
- A person can see near objects without difficulty
- But the difficulty in viewing the distant object
- Light is focused in front of the retina
- Corrected by a bi-concave lens
Causes
- Increase in the anteroposterior diameter of the eyeball
- The high refractive index of the lens
- Increase in curvature of the lens
2) Hypermetropia (Far-sightedness)
Features
- A person can see distant objects without difficulty.
- But the difficulty in seeing near objects.
- Light is focused behind the retina
- Corrected by Bi-convex lens
Causes:
- Decreases in the anteroposterior diameter of the eyeball
- The low refractive index of the lens
- Decrease in the curvature of the lens
3) Astigmatism:
In this condition, due to unequal curvature of the lens, refraction of the ray of light diffuses widely instead of being sharply focused on the retina.
4) Presbyopia
Defect in vision in older age.
The person feels difficulty in seeing near objects due to loss of accommodation.
Thus:
The anteroposterior diameter of the eyeball and the shape and curvature of the cornea determines the focal point. |
|
Changes in these result in myopia or short-sightedness, hypermetropia or long-sightedness.
|
Accommodation:
It is the process of adjustment of the optical apparatus for the near-vision.
Changes occur in accommodation
- Contraction of the pupil of both eye
- Increase curvature of the lens
- Medial convergence of eyeball
Nerve related accommodation
Parasympathetic Fibers from the Edinger-Westphal nucleus rely on the ciliary ganglion which supplies ciliary muscle and sphincter papillae of the iris
|
Contraction of the ciliary muscle
|
Relaxation of the suspensory ligament of lens
|
Increase in the anterior curvature of the lens and increase convergence power of the lens |
Sphincter pupillae of iris (smooth muscle)
|
Contraction
|
Making light wave passes through the central portion of the lens
|
|
The oculomotor nerve supplies the medial rectus, which causes the medial convergence of the eyeball.
|
Aqueous humor:
It is the clear fluid that fills the space between the cornea in front and the lens behind.
This space is divided by iris into
- Anterior chambers
- Posterior chambers
Which freely communicate with each other through the pupil
Circulation of Aqueous Humour:
Secreted into the posterior chamber from the capillaries in the ciliary processes.
|
Through pupil
|
The anterior chamber of the eye
|
Canal of scheme
|
Anterior ciliary vein
|
Ophthalmic vein
The function of aqueous humor:
- Acts as refractive media
- Rich in ascorbic acid, glucose & amino acid & nourishes the avascular tissues of the cornea and lens
Applied anatomy:
| Interference with the drainage of the aqueous humor into the canal of Schlemm results in an increase in intraocular pressure (glaucoma). |
| This produces cupping of the optic disc and pressure atrophy of the retina causing blindness. |
Vitreous body/Vitreous Humour:
It is a colorless, jelly-like transparent mass that fills the posterior segment of the eyeball.
* It is enclosed in the hyaloid membrane.
Development of eyeball:
The optic vesicle forms the optic cup.
It is an outpouching from the forebrain vesicle.
1) Lens from lens placode (ectodermal)
2) Retina
Pigment layer from the outer layer of the optic cup.
Nervous layers from the inner layer of the optic cup.
3) Choroid, sclera - from mesoderm
4) Cornea-surface ectoderm forms the epithelium, and other layers develop from mesoderm.
Note:
|
The eye begins to develop as a pair of shallow grooves on the sides of the forebrain.
These grooves form out-pocketing of the forebrain known as optic vesicles which later invaginate to form a double-walled optic cup.
|
|
All the body's muscles develop from mesoderm, except the muscle of the iris which develops from surface ectoderm.
|
The hyaloid canal extends from the optic disc to the lens.
The canal marks the site of the hyaloid artery in the fetus.
The hyaloid artery is a continuation of the central artery of the retina which disappears 6 weeks before birth. |
Importance of binocular vision in human
Helps in 3D vision.
One can determine the shape, and size and predict the distance of the object.
The optical defect of one eye is corrected by another eye. |
Clinical Anatomy:
|
Glaucoma:
Overproduction of aqueous humor or lack of drainage both could rise Intraocular pressure. This condition is called glaucoma.
|
|
Cataract:
The opacity of the lens is called a cataract.
|
|
The central artery of the retina is an end artery so, the blockage of the artery leads to sudden blindness because most of the inner nervous layer of the retina is supplied by this artery only.
|
|
Miosis -- a contraction of pupils (parasympathetic)
Mydriasis -- means the dilation of pupils (Sympathetic)
|
|
Ptosis means the dropping down of upper eyelids.
Oculomotor never paralysis or Horner’s syndrome causes partial ptosis.
Because the levator palpebrae superioris muscle which helps in the elevation of the upper eyelid is supplied by III cranial nerve and partially by sympathetic fibers arise from the cervical ganglion.
|
Argyll Robertson pupil:
It is the condition in which the light reflex is lost but the accommodation reflex is retained.
Causes can be a lesion of fibers from the pretectal nucleus to the Edinger Westphal nucleus.
|
The cornea can be grafted from one person another, as it is avascular.
The bulbar conjunctiva is vascular.
Inflammation of the conjunctiva leads to conjunctivitis.
|
While looking at an infinite far the light rays run parallel ciliary muscle is relaxed, the suspensory ligament is tense and the lens is flat.
While reading a book, the ciliary muscles contract
and the suspensory ligament is relaxed making the lens more convex. |
|
The palpebral conjunctiva is used to judge the hemoglobin levels for the diagnosis of jaundice.
Similarly, the inferior surface of the tongue (in the deep lingual vein) is also judged for the diagnosis of jaundice.
|
|
The congestion of the optic disc from the increased intracranial pressure is called papilledema.
As we know CSF present in subarachnoid space extends up to the posterior part of the eyeball through the optic nerve.
|
|
One can see the interior of the eye by an ophthalmoscope.
Through the ophthalmoscope, one can see the small vessels in the retina and judge the changes in diabetes and hypertension.
In addition, one can also examine the optic disc for evidence of papilloedema, caused by raised intracranial pressure.
|
|
Retinal detachment occurs between the outer single-pigmented layer and the inner nine nervous layers.
Actually, it is an inter-retinal detachment.
A silicone sponge is put over the detached retina, which is kept in position by a band.
Retinal detachment occurs as the outer layer and the inner nervous layer are developmentally different.
|
Horner’s syndrome:
It is the syndrome characterized by:
* Ptosis- dropping of the upper eyelid
* Miosis- excessive contraction of the pupil
* Anhydrosis- Loss of sweating on the sides of the face
* Enopthalmos- retraction of the eyeball (opposite of exophthalmos)
Causes of Horner’s syndrome:
Injury to the cervical sympathetic trunk
|
Comments (0)