Internal ear
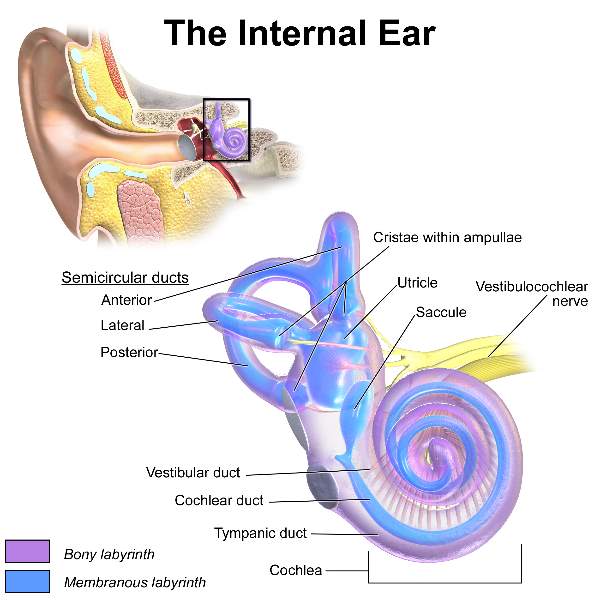
The internal ear is composed of a bony labyrinth within which a membranous labyrinth is present.
The membranous labyrinth is filled with endolymph.
And membranous labyrinth is separated from the bony labyrinth by another fluid called the perilymph.
Bony labyrinth
The bony labyrinth consists of three parts:
- Cochlea anteriorly.
- Vestibule, in the middle.
- Semicircular canals posteriorly
Cochlea:
Resembles the shell of a common snail.
The spiral ridge of bone (spiral lamina) which partially divides the cochlear canal into
- Scala vestibuli above
- Scala tympanic below
The division is completed by the basilar membrane.
The scala vestibuli communicates with scala tympani at the apex of the cochlea by a small opening called the helicotrema.
As a whole:
The bony cochlea has three compartments divided by a vestibular membrane (Reissner’s membrane) & basilar membrane.
- Scala vestibuli- above the vestibular membrane.
- Scala tympani below the basilar membrane.
- Scala media or spiral duct of the cochlea between two membranes. [ie. Spiral duct of the cochlea present between the scala vestibuli and scala tympani.]
Fenestra cochleae (Round window) is a round opening present in the cochlea that opens into the scala tympani of the cochlea.
And it is closed by the secondary tympanic membrane.
But Fenestra vestibuli (Oval Window) opens in the vestibule.
Scala vestibuli and scala tympani are filled with perilymph as they are part of the bony labyrinth (cochlea.)
Scala media/ Spiral duct of the cochlea is filled with endolymph as it is the part of the membranous labyrinth.
Tips
Summary Connection pathway
Stapes (from middle ear cavity)
|
Oval window (fenestra vestibuli), an opening on the vestibule
|
Vestibule
|
Scala vestibuli (of cochlea)
|
From the apex of the cochlea,
communicate with
Scala tympani (of cochlea)
|
Round window, a round opening present on the cochlea (lower part)
[Which is guarded by secondary tympanic membrane]
|
Thus, perilymph of scala tympani doesn’t escape into
|
Tympanic cavity (middle ear)
Tips
|
Vestibule communicates with cochlea through scala vestibule.
* But scala tympani communicate with the tympanic cavity (middle ear) through the round opening (Fenestra cochlea) which is closed by the secondary tympanic membrane.
|
|
Fenestra vestibuli is an oval opening in the vestibule.
* But Fenestra cochlea is round opening found on cochlea (lower part).
|
|
Scala vestibuli and scala tympani are continuous with each other through a narrow opening at the apex of the cochlear duct called helicotrema.
|
|
Perilymph presents within the space of the bony labyrinth that surrounds and protects the membranous labyrinth.
|
|
Just like the composition of other extracellular fluid-like CSF, the composition of perilymph is similar.
* Perilymph has a more concentration of Na+ & low concentration of K+.
|
Perilymph is probably formed by the blood plasma through the selective membrane transport mechanism allowing selectively substances to pass through walls of capillaries like CSF formation by choroid plexus.
* CSF also contributes to the formation of perilymph. |
|
But endolymph has low Na+ concentration and high K+ concentration.
|
Vestibule:
Opening present in vestibule
- Fenestra vestibuli (Oval window) is an oval opening that leads into the vestibule of the internal ear and is closed by the foot-plate of the stapes.
- Opening of aqueduct of vestibule through which endolymphatic duct passes.
- Three semicircular canal open into the vestibule by five opening.
Semicircular canals:
There are three bony semicircular canals
- Anterior semicircular canal
- Posterior semicircular canal
- Lateral semicircular canal
Above 3 canals open into the vestibule by five opening.
Dilated of each canal is called ampulla which corresponds with the ampulla of the semicircular duct of the membranous labyrinth.
Membranous labyrinth
It is present within the bony labyrinth.
- Cochlear duct lies within bony cochlea.
- Saccule & utricle within bony vestibule.
- Semicircular ducts within bony semicircular canals.
It has a continuous closed cavity that is filled by endolymph.
|
Same as the bony labyrinth, 3 main parts of the membranous labyrinth available:
|
|
a. Spiral duct of cochlea having an Organ of Corti.
|
|
b. Utricle and Saccule having maculae as the organs of static balance. (Within the vestibule)
|
|
c. Semicircular Ducts having cristae the organs of kinetic balance. (Posteriorly)
|
Spiral duct of the cochlea or Scala media
Scala media present between the scala vestibuli and the scala tympani.
Roof:
Formed by vestibular membrane which separates it from scala vestibule.
Floor:
Formed by basilar membrane (that separates it from scala tympani).
The basilar membrane of the spiral duct of cochlea contains the Spiral organ of Corti which is the end organ for hearing.
Posteriorly, the duct is connected to the saccule.
Spiral Organ Of Corti
It is an organ of hearing located on the basilar membrane of the cochlear duct (Spiral duct of cochlea).
Importance component:
- Inner & outer rod cells
- Outer and inner hair cells
- Tunnel of Corti
- Supporting cells
- Membrana tectoria
* Tunnel of rod is formed by the inner and outer rod cells and separates the inner and outer hair cells.
* Inner & outer hair cells - receptor cells of hearing, posses stereocilia & located on the basilar membrane and
* Membrana tectoria located above the hair cells and helps to stimulate hair cells.
* Hair cells are innervated by the process of bipolar cells of spinal ganglion from where cochlear nerve arises.
Note: Cochlear duct / spiral duct of cochlea containing endolymph lies in between the scala vestibuli and scala tympani containing perilymph.
Saccule and utricle
They are present within the vestibule.
Saccule - continue with the spiral duct of the cochlea anteriorly.
Utricle receives the end of three semicircular ducts through five opening.
Tips
Spiral duct of Cochlea
|
Utricle
|
Saccule
|
Semicircular ducts
The duct of saccule united with the duct of the utricle to forms the ductus endolymphaticus which passes through the aqueduct of the vestibule in the posterior part of the petrous part of the temporal bone.
The medial wall of saccule and utricle are thickened to form macula which is the static balance receptor.
- Saccule gets stimulated by linear motions (going in a lift).
- Utricle gets stimulated by horizontal linear motion (going in a car).
Mnemonic:
SUM, saccule and utricle has maculae as receptor.
Semicircular Ducts
They lie within the semicircular canal.
- Anterior semicircular duct
- Lateral semicircular duct
- Posterior semicircular duct
Dilated part of the semicircular duct called ampulla contains crista which is the kinetic balance receptor.
* Cristae respond to pressure changes in the endolymph caused by movements of the head.
Tips:
Maculae sense the position of the head in response to gravity and linear acceleration ie. static balance
Cristae respond to angular acceleration ie kinetic balance.
Summary
| Organ of Corti is the receptor of hearing present in the basilar membrane of the spiral duct of cochlea. |
| Maculae is the static balance receptor present in the utricle and saccule. |
| Cristae is the kinetic balance receptor present in the Ampulla of semicircular canal. |
| All part of membranous labyrinth is filled by endolymph. |
| Hair cells of the Organ of Corti is innervated by neuron of the spiral ganglion from where cochlear nerve begin. |
| Organ of equilibrium (maculae and cristae) both are innervated by neurons of vestibular ganglion from where vestibular nerve arises. |
|
Both vestibular nerve and cochlear nerve united and pass-through internal acoustic meatus as vestibulocochlear nerve.
|
Blood supply of external ear
- The outer part of the canal is supplied by the superficial temporal and posterior auricular arteries.
- Inner part, by the deep auricular branch of the maxillary artery.
Blood supply of tympanic membrane
- The outer surface is supplied by
Deep auricular branch of the maxillary artery
- The inner surface is supplied by
Anterior tympanic branch of the maxillary artery and
By the posterior tympanic branch of the stylomastoid branch of the posterior auricular artery.
Blood supply of middle ear
1) The anterior tympanic branch of the maxillary artery
2) The posterior tympanic branch of the stylomastoid branch of the posterior auricular artery
Veins from the middle ear drain into the superior petrosal sinus and the pterygoid plexus of the veins.
Blood supply of labyrinth
- Arterial supply
From labyrinthine artery, branch of basilar artery
- Venous supply
From labyrinthine vein drain into the superior petrosal sinus or transverse sinus
Note:
Maxillary artery and superficial temporal arteries are the terminal branches of the external carotid artery around the ear.
Lymphatic of ear:
Lymphatic of ear mainly drain into
- Preauricular lymph node
- Post auricular lymph node
- Retropharyngeal lymph node
Nerve supply of external acoustic meatus
- Roof & anterior wall
By the auriculotemporal nerve, branch of mandibular nerve
- Floor & Posterior wall
By the auricular branch of the vagus.
Nerve supply of tympanic membrane
Outer surface:
- Anterior half is supplied by the auriculotemporal nerve, branch of mandibular nerve.
- Posterior half by the auricular branch of the vagus nerve.
Inner surface
Supplied by the tympanic branch of the glossopharyngeal nerve.
Nerve supply of middle ear & auditory tube
Nerve supply of middle ear derived from tympani plexus which lie over the promontory.
Note:
|
Tympanic plexus is formed by
- Tympanic branch of glossopharyngeal nerve
- Sympathetic plexus around the internal carotid artery
|
|
Lesser petrosal nerve arises from tympanic plexus contain secretomotor fibers of the glossopharyngeal nerve to supply the parotid gland via otic ganglion.
|
Development of Ear
Auricle
From six mesodermal tubercles around the external opening of 1st pharyngeal cleft
External acoustic meatus
From 1st pharyngeal cleft (ectodermal)
Middle ear (Tympanic cavity) & Auditory tube
From tubotympanic recess which arises from 1st pharyngeal pouches (endodermal in origin)
Mastoid antrum
Develops as an extension of the middle ear cavity into mastoid antrum
Internal ear
From otic placode (an ectodermal thickening)
Ossicles
Malleus & incus
From the Cartilaginous component of 1st pharyngeal arch
Stapes
From the cartilaginous component of 2nd pharyngeal arch
Muscles
Tensor tympani
From 1st pharyngeal arch (mesodermal)
Stapedius
From 2nd pharyngeal arch (mesodermal)
The tympanic membrane comprises all three embryonic layers.
- Outer layer is ectodermal
- Middle layer in mesodermal
- The inner layer is endodermal in origin.
Development correlation:
| * External acoustic meatus along with outer cuticular layer develops from 1st pharyngeal cleft (ectodermal in origin). |
| * Middle fibrous layer from mesenchyme (mesodermal in origin). |
|
* Inner mucous layer along with middle ear and auditory tube develops from 1st pharyngeal pouch (endodermal in origin).
|
Clinical anatomy:
|
Infection of the middle ear (otitis media):
It is common especially in infants and children.
Infective agent reaches the middle ear from the upper respiratory tract through an auditory tube producing pus within the middle ear.
|
|
Infection of the middle ear (otitis media) is common in children due to the following peculiarities of auditory tubes of children.
- Shorter length
- Wider diameter
- More horizontal in direction
|
|
Inflammation of the auditory tube is often secondary to an attack of the common cold.
This causes pain in the ear which is aggravated by swallowing, due to blockage of the tube.
Pain is relieved by the installation of decongestant drops in the nose which helps to open the ostium.
|
|
Otosclerosis:
Sometimes bony fusion takes place between the footplate of the stapes and the margins of the fenestra vestibuli.
This leads to deafness.
|
|
Otitis externa:
Condition that causes inflammation redness & swelling of the outer ear canal.
|
|
Hyperacusis:
Both, tensor tympani and stapedius contract reflexly and simultaneously to dampen very loud sounds,
Thus preventing noise trauma to the internal ear.
The paralysis of stapedius results in hyperacusis (an abnormally increased power of hearing) where even whisper appears as noise.
|
|
Boils and infection of the outer ear canal cause a little swelling but are extremely painful, as skin is fixed to the underlying bone & cartilage.
|
|
Referred pain of ear:
Since the middle ear and external ear are supplied by the branches of trigeminal (CN V), glossopharyngeal (CN IX) and vagus (CN X) nerves, the pain in the ear (otalgia) is often referred to other areas supplied by these nerves, e.g., tongue, teeth, tonsil, and pharynx.
|
|
Endolymph is produced by striae vascularis. This process requires melanocytes.
The disorders of melanocytes (ie albinism) are associated with deafness.
|
External auditory tube is not a straight tube ie S-shaped course.
Therefore, to examine the tympanic membrane the pinna has to be pulled upwards, backward, and laterally, to bring the two parts in alignment.
While in infants it is pulled downwards and backward. This is because in infants the bony part of the external auditory meatus is not developed.
|
| The irritation of the auricular branch of the vagus nerve during syringing may reflexly produce persistent cough called ear cough, vomiting and even death due to sudden cardiac inhibition. |
|
On the other hand mild, mild stimulation of this nerve may reflexly produce increased appetite
(Syringing means pushing the water inside the ear to clean them.)
|
|
The Aldermen were the individuals in ancient Rome, who were very fond of excessive eating and used to stimulate their jaded appetite by dropping cold water or spirit behind the ear as this could reflexly stimulate gastric peristalsis due to supply of this area by the vagus nerve which also supplies motor innervation to the GIT.
|
Comments (0)