Colles fracture
Colles Fracture is the fracture of the distal end of the radius 2.5 cm proximal from the radio-carpal joint with or without fracture of the ulnar styloid process.
Colles fracture was described by Abraham Colles in 1814. It is the transverse fracture radius at 2 cm proximal to the distal articular surface of the radius with dorsal displacement of the distal fragments.
The ICD 10 Code for colles fracture is S52.53. Moreover, the ICD 10 code for colles fracture of the right radius is S52.531 (i.e. S52.531A for colles fracture of right radius, initial encounter for closed fracture). The ICD 10 code for colles fracture of left radius is S52.532 (i.e. S52.532A for colles fracture of left radius, initial encounter for closed fracture).
Mechanism of Colles fracture
The mechanism of colles fracture is people fall on outstretched hand with the wrist in extensions and force is applied in the length of the forearm and wrist. This leads to compression and bending of the distal radius, ultimately resulting in the fracture of the distal radius with dorsal displacement of the distal fragment of the radius. The bone fracture at the corticocancellous junction of the distal end of the radius.
Colles fracture commonly occurs in older adults especially postmenopausal women, with decreased bone density (osteoporosis) because their bones are more brittle and prone to fracture with less force.
Patient profile in Colles Fracture
Colles fracture is the most common fracture in older people, the high incidence being related to the onset of postmenopausal osteoporosis. The common age group in which the colles fracture occurs is elderly postmenopausal women. Colles fractures commonly occur due to a fall in an outstretched hand.
Symptoms of Colles fracture
The common symptoms of Colles Fracture are
- History of Trauma or fall on outstretched hand
- Pain, Swelling around the wrist joint
- Unable to move the wrist joint
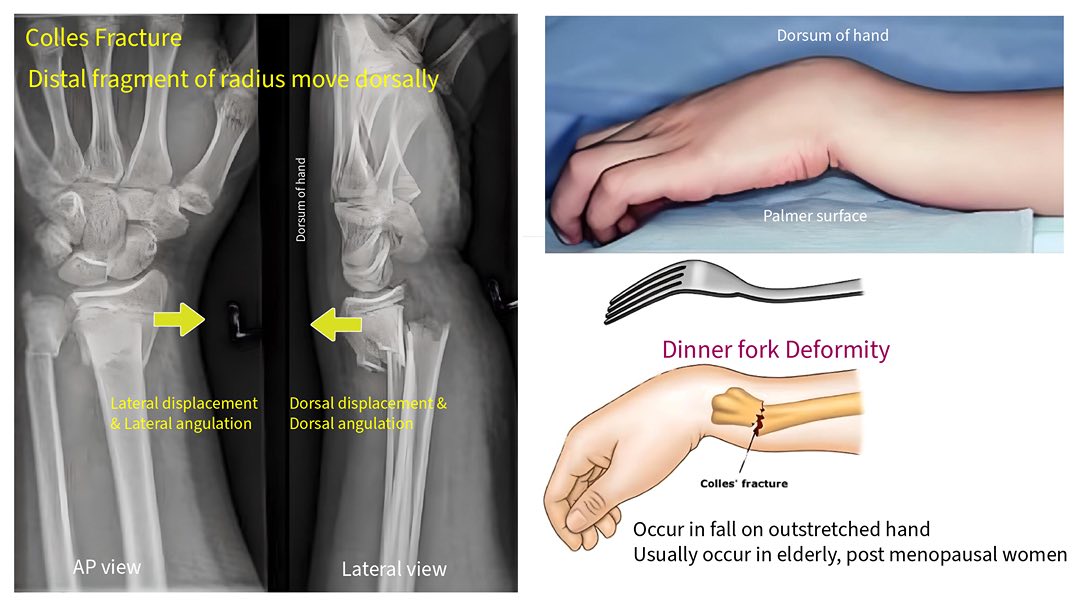
- Dinner fork deformity
Clinical Features of Colles Fracture
The clinical features of Colles Fracture are
- Raised Temperature
- Local Tenderness around the wrist joint
- Swelling
- Painful & restricted movement of the wrist and fingers
- Dinner fork deformity with bony prominence on the back of the wrist
Deformity/Displacement of Colles fracture
A Colles fracture is often associated with a specific type of deformity known as a "dinner fork" deformity due to the way the wrist appears after the fracture due to the dorsal displacement of the distal end of the radius. This deformity typically includes the following characteristics. The common displacement/deformity of colles fracture are:
- Dorsal displacement, Dorsal angulation
- Lateral displacement, Lateral angulation
- Pronation
- Impaction of the fragments

Figure: Dinner Fork Deformity in Colles fracture
Investigation done in colles fracture
To investigate a suspected Colles fracture and confirm the diagnosis, medical professionals typically use a combination of clinical examination and imaging studies. The commonly done investigation for Colles fracture is an X-ray of the wrist joint.
Colles fracture is confirmed by X-ray of wrist joints including the distal part of the radius & ulna in the Anterior Posterior (AP view) and Lateral view.
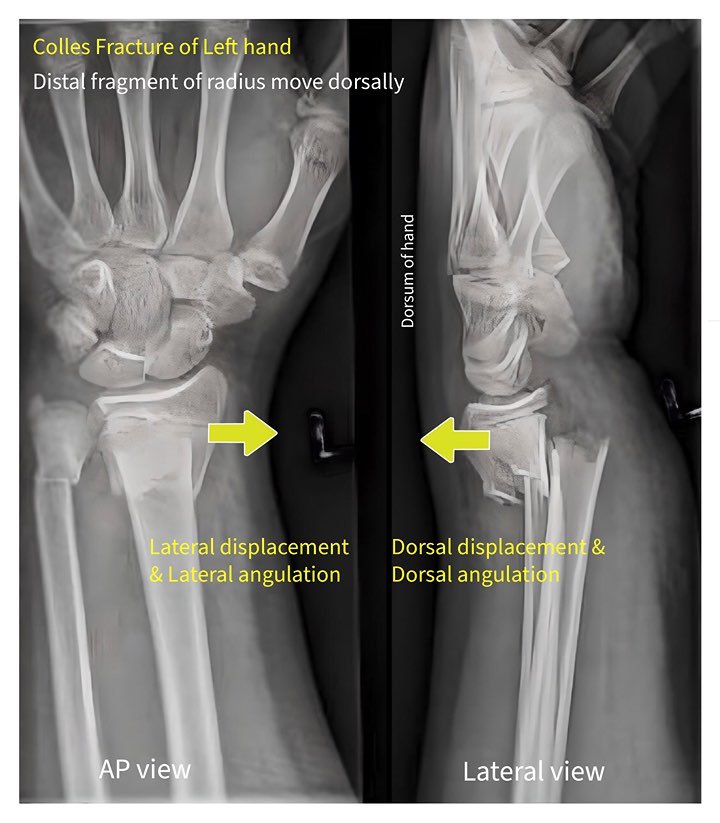
Figure: Colles fracture X ray
Treatment of Colles Fracture
Treatment of colles fracture typically involves immobilizing the wrist with a colles cast or splint and in some cases, surgical intervention might be needed to realign and stabilize the fractured bones.
In case of undisplaced colles fracture, a dorsal splint is applied for a day or two until the swelling has resolved, then the colles cast is completed. An X-ray is taken after 2 weeks to ensure that the fracture has not slipped. If not slipped, the cast can usually be removed after 6 weeks to allow mobilization. If slipped, surgery may be required.
In case of displaced colles fracture, displaced fractures of the distal fragment of the radius must be reduced under anesthesia (hematoma block, Bier's block, axillary block, or general anesthesia) by traction and counter traction followed by Colles cast for 6 weeks.
Colles Fracture Reduction Steps:
Colles Fracture reduction steps involve:
- Closed reduction by traction & counter-traction
- Palmer flexion
- Ulnar Deviation at 15 - 20°
- Immobilization by colles cast (from knuckle to below elbow)
Management of Colles fracture
In most of cases, Colles fractures are managed by Closed reduction by traction & counter traction & immobilization by colles cast with palmer flexion, and ulnar deviation 20 ° each under hematoma block. Colles cast is given colles fracture from knuckle to below the elbow with palmer flexion & ulnar deviation 20 ° each for 6 weeks. Normally it takes around 6 weeks for bone union in Colles fracture. Thus, the normal healing time in colles fracture is around 5- 6 weeks.
Follow up in Colles fracture
2 weekly X-rays & follow-ups are required for up to 6 weeks in case of Colles fracture.
Advice after giving Colles cast
- The patient is asked to make finger movements, and elbow and shoulder movements to prevent joint stiffness.
- Weight-bearing work is avoided.
- If any intense pain or swelling is noticed, visit the doctor as soon as possible.
Advice after removal of plaster:
- No massages
- If the patient complaints of pain and swelling of the wrist and hand then Analgesic
- Active exercise of the fingers
- Physiotherapy
- Crepe bandage
Complications of Colles fracture:
Early complications of Colles fracture are
- Radial artery injury
- Median nerve injury (Carpal tunnel syndrome)
- Extensor pollicis longus injury
Late complications of Colles fracture are
- Malunion
- Joint stiffness
- Volkman ischemic contracture
- Osteoarthritis
- Sudeck's osteodystrophy (CRPS: Complex regional pain syndrome)
- Shoulder hand syndrome
Differential Diagnosis of Colles Fracture
The differential diagnosis of Colles' fracture are
- Smith's fracture
- Barton's fracture
- Fracture radial styloid (Chauffeur's Fracture)
- Scaphoid fracture
What are the fractures that can occur due to falling on an outstretched hand?
- Fracture of clavicle
- Fracture neck of the humerus
- Fracture shaft of humerus
- Supracondylar fracture of humerus
- Fractures of the radius and ulna
- Colles fracture
- Scaphoid fracture
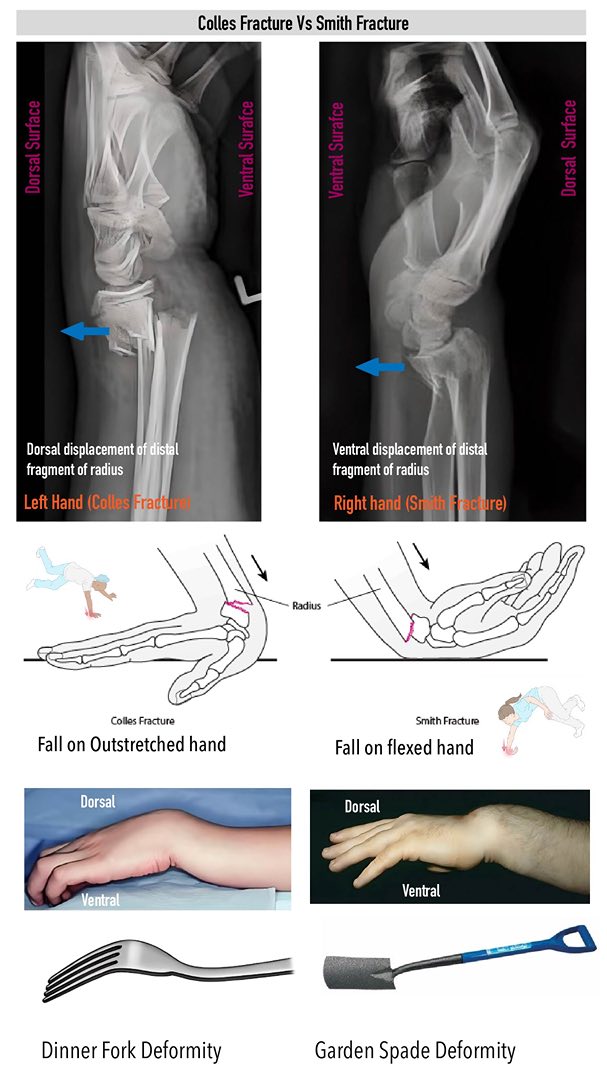
Smith's fracture: Smith fracture also called reserved colles fracture in which transverse fracture occurs at the lower end of radius 2.5 cm proximal of the articular surface with anterior displacement of distal fragment of radius (garden spade deformity).

Figure: Garden spade deformity in Smith fracture
Colles vs Smith fracture
The main difference between Colles fracture and Smith fracture is in Colles fracture there is the dorsal displacement of the distal fragment of the radius but in Smith fracture, there is ventral displacement of the distal fragment of the radius. Colles fracture occurs after a fall on an outstretched hand whereas Smith fracture occurs on an inward flexed hand at the wrist joint.
| Colles fracture | Smith’s Fracture |
| Dorsal displacement & dorsal angulation of distal fragment of radius | Ventral displacement & ventral angulation of distal fragment of radius |
| Lateral displacement & lateral angulation of distal fragment of radius | Medial displacement & medial angulation of distal fragment of radius |
| Supination | Supination |
| Dinner fork Deformity | Garden Spade Deformity |
| Occurs on outstretched hand (Extension) | Occurs on inward flexed hand (Flexion) |
Difference between Colles fracture and Smith fracture
Barton Fracture: Colles fracture or Smith’s fracture with intra-articular surface involvement is called Barton Fracture.
Monteggia's fracture: It is a fracture of the upper third of the ulna with anterior displacement of the upper fragment of the ulna and anterior dislocation of the radius. In short, Monteggia’s fracture is the proximal ulnar fracture with superior radio-ulnar joint dislocation.
Galeazzi fracture: It is a fracture of the distal 1/3rd end of the radius with dislocation or subluxation of the inferior radioulnar joint. It is due to rotational force causing swelling of the lower forearm; prominent head of ulna; and ulnar nerve injury.
Bennet's fracture: It is an oblique fracture occurring at the base of 1st metacarpal bone with subluxation of the carpometacarpal joint. A triangular fragment of fractured bone remains in position. If the fracture is T or Y-shaped it is called Rolando's fracture.

Comments (0)