
Lymphoma
Lymphomas are malignant neoplasms characterized by the proliferation of cells native to the lymphoid tissues, that is, lymphocytes, histiocytes, and their precursors and derivatives.
Broad groups of malignant lymphomas
- Hodgkin’s lymphoma.
- Non-Hodgkin’s lymphomas.
Diseases of the lymph node Causes
A. Inflammatory/ hyperplastic diseases
|
1) Infective: Bacterial:
Viral:
Fungal:
Parasite:
|
|
2. Others:
|
B. Neoplastic cause:
- Malignant lymphoma
-
- Hodgkin’s lymphoma.
- Non-Hodgkin’s lymphoma.
- Leukemia: ALL; CLL
- Histiocytosis – X
- Angio-immunoblastic lymphadenopathy
- Metastatic carcinoma.
.
Tumors of lymph nodes:
- Primary Tumor:
-
- Hodgkin’s lymphoma.
- Non-Hodgkin’s lymphomas
- Secondary tumor:
More common
Metastatic carcinoma - Lung, Breast, Thyroid, Stomach
LYMPHOMA:
Lymphomas are malignant neoplasms characterized by the proliferation of cells native to the lymphoid tissues, that is, lymphocytes, histiocytes, and their precursors and derivatives.
Broad groups of malignant lymphomas
- Hodgkin’s lymphoma.
- Non-Hodgkin’s lymphomas.
Classification of lymphoid neoplasms
- Revised European-American Classification of Lymphoid neoplasms (REAL), 1994.
- The WHO Classification of the Lymphoid neoplasms, (Updated REAL) 1997.
WHO Classification of the Primary Lymphoid neoplasms:
- Nodular sclerosis
- Mixed cellularity
- Lymphocyte rich
- Lymphocyte depletion.
- Lymphocyte predominance.
Classifications of Non-Hodgkin’s lymphoma
- Rappaport classification- based on morphology and cytologic character.
- Lukes-Collins Classification-Based on cell origin.
- Keil classification.
- Working formulation- Based on clinical course and morphology.
Working Formulation of Non-Hodgkin’s Lymphomas for Clinical Usage, 1982
|
Low-grade
|
|
Intermediate-grade
|
|
High-Grade
|
|
Miscellaneous
|
Burkitt Lymphoma
Burkitt lymphoma occurs in three different settings, although they are histologically identical-
- African (endemic) Burkitt lymphoma
- Sporadic (non-endemic) Burkitt lymphoma
- A subset of aggressive lymphomas occurs in patients infected with HIV.
Morphology of Burkitt Lymphoma:
- Loss of nodal architecture.
- There is the proliferation of a striking monotonous cell (intermediate size, 10 to 20 mm) with round to oval nuclei containing two to five nucleoli and a moderate amount of faintly basophilic cytoplasm.
- A high mitotic index is typical, as is apoptotic tumor cell death, accounting for the presence of numerous tissue macrophages with ingested nuclear debris.
- Because these benign macrophages, which are diffusely distributed among the tumor cells, are often surrounded by a clear space, they create a characteristic starry sky pattern.
Clinical features of Burkitt Lymphoma:
- Both African and sporadic Burkitt lymphoma occurs largely in children and young adult.
- Most arise in extranodal sites.
- African Burkitt lymphoma often presents in the mandible whereas non-endemic Burkitt lymphoma most commonly occurs as an ileocaecal or peritoneal mass.
- Immunophenotype- Tumors comprise relatively mature B cells expressing surface IgM, monotypic k and l light chains, and CD 19, CD 20, and CD 10.
Prognosis of Burkitt Lymphoma:
Very aggressive. Respond well to chemotherapy in children and young adults.
Mycosis fungoides and Sezary syndrome:
These tumors of peripheral CD+ T cells are characterized by the involvement of skin and therefore belong to the group of cutaneous T cell lymphomas. Median survival 8-9 years.
Mycosis Fungoides
Clinically presents in three cutaneous lesions
- Inflammatory premycotic phase.
- Plaque phase.
- Tumor phase.
Histologically:
There is infiltration of the epidermis and upper dermis by neoplastic T cells, which have cerebreform nucleus, characterized by marked infolding of the nuclear membrane.
Sezary syndrome
It is a variant in which skin involvement is manifested as a generalized exfoliation erythroderma associated with leukemia of Sezary cells.
Hodgkin’s Lymphoma:
Historical Background
First described by Thomas Hodgkin (1832). However, it was named after him by Samuel Wilks in 1865
Classification of Hodgkin’s lymphoma:
The WHO recognizes five subtypes of Hodgkin’s lymphoma.
- Nodular sclerosis. (65%-70%)
- Mixed cellularity. (20%-25%)
- Lymphocyte rich. (Rare)
- Lymphocyte depletion. (<5%)
- Lymphocyte predominance. (5%)
Morphology of Hodgkin’s lymphoma:
- Identification of Reed-Sternberg cells (RS cells) and their variants is essential for the histologic diagnosis of HL.
- They must be present in an appropriate background of non-neoplastic inflammatory cells (lymphocytes, plasma cells and eosinophils).
Reed-Sternberg cell (RS cell):
A distinctive tumor giant cell known as the Reed-Sternberg cell (RS cell) is considered to be the essential element in all forms of Hodgkin’s disease.
|
Classic RS cells are: • Quite large (15-45mm in diameter) cell. • Binucleate or bilobed, with the two halves appearing as mirror images of each other, there are multiple nuclei or the single nucleus is multilobed. • The nucleus is enclosed within an abundant amophophilic cytoplasm and contains large, inclusion-like, owl-eyed nucleoli, generally surrounded by clear halo, that are about the size of a small lymphocyte (5-7mm). |
Other Several morphologic variants of Reed-Sternberg cells are recognized.
- Mononuclear variants:
Contain only a single round nucleus with a large inclusion like the nucleolus. - Lacunar cells:
Seen predominantly in the nodular sclerosis subtype, have more delicate folded or multilobate nuclei surrounded by abundant pale cytoplasm that is often disrupted during cutting of sections, leaving the nucleus sitting in an empty hole (the lacune). - Lymphohistiocytic variants (L&H cells):
Contain polypoid nuclei resembling popcorn kernels, inconspicuous nucleoli, and moderately abundant cytoplasm are specific to the lymphocytic predominance subtype.
Morphology of Hodgkin’s lymphoma:
In classical forms of Hodgkin’s lymphoma, Reed-Sternberg cells undergo a peculiar form of cell death in which the cells shrink and become pyknotic, a process described as “mummification”.
Reed-Sternberg like cells may be present in other conditions like,
- Infectious mononucleosis,
- Solid tissue cancers
- NHL.
- Mycosis fungoides
WHO classification of Hodgkin’s lymphoma:
|
1. Hodgkin lymphoma, Nodular sclerosis type This is the most common form of HL, constituting 65-70% of cases, and occurs with equal frequency in males and females. The prognosis is excellent. Histology:
|
|
2. Hodgkin Lymphoma, Mixed Cellularity type This form of HL constitutes about 20-25% of cases. More common in males and strongly associated with EBV. The prognosis is very good. Histology:
|
|
3. Hodgkin Lymphoma, Lymphocyte rich type This is an uncommon form of classical HL. It is associated with EBV in about 40% of cases and has a very good to excellent prognosis. Histology:
|
|
4. Hodgkin Lymphoma, Lymphocyte Depletion type This least common form (<5%cases) of HL. Observed predominantly in
Histology:
|
|
5. Hodgkin Lymphoma, Lymphocyte Predominance type
Histology:
|
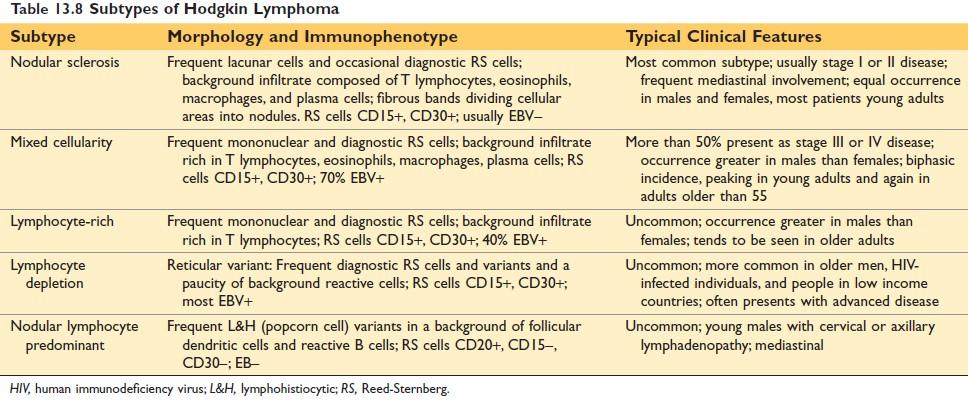
Figure: Subtypes of Hodgkin Lymphoma Robbin’s Page 611
Differences between Hodgkin Lymphoma and Non-Hodgkin Lymphoma
| Hodgkin lymphoma | Non-Hodgkin Lymphoma |
| More often localized to a single axial group of nodes (cervical, mediastinal, and paraaortic | More frequent involvement of multiple peripheral nodes. |
| Orderly spread by contiguity. | Noncontiguous spread. |
| Mesenteric nodes and Waldeyer ring are rarely involved | Waldeyer ring and mesenteric nodes are commonly involved. |
| Extranodal involvement - uncommon. | Extranodal involvement - common. |
| RS giant cells are always present | RS giant cells are absent. |
| Pleomorphic infiltration by lymphocytes, histiocytes, neutrophils, plasma cells, and eosinophils. | Monomorphic infiltration is usual |
Laboratory diagnosis of Lymphoma:
1. FNAC from enlarged lymph node: Monotonous population of lymphoid cells having a large hyperchromatic nucleus and scanty cytoplasm.
2. Histopathology:
- Loss of nodal architecture.
- Proliferation of lymphoid cells having a large hyperchromatic nucleus and scanty cytoplasm.
- RS cells are present in HD and absents in NHL.
3. Routine blood examination
- Hemoglobin: Normal or reduced.
- ESR: Increased.
- PBF: Spillage of the immature lymphoid cells may occur.
Differences between follicular lymphoma and reactive follicular hyperplasia
| Follicular non-Hodgkin’s Lymphoma | Reactive Follicular Hyperplasia |
| Complete effacement of normal architecture | Preservation of nodal architecture |
| Slight or moderate variations in size and shape of follicles. | Marked variations in size and shape of follicles. |
| Lymphomatous follicles tend to be monomorphic | A mixed population of lymphocytes in different stages of differentiation and histiocytes within the germinal center (Pleomorphic follicles). |
| Lack of phagocytosis. | Prominent phagocytic activity in the germinal center |
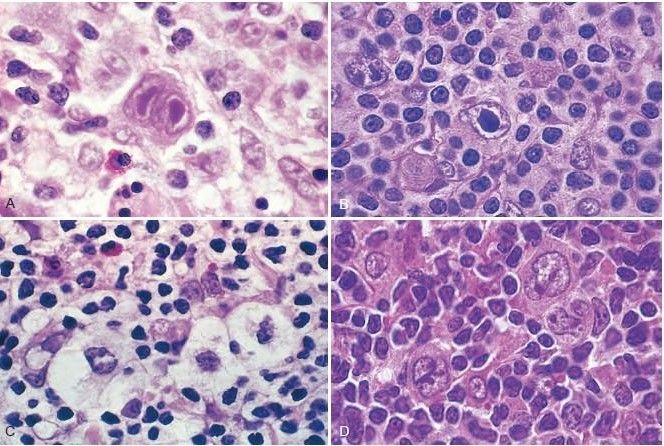
Figure: Reed-Sternberg cells and variants (Robbin’s Page 613)
(A) Diagnostic Reed-Sternberg cell, with two nuclear lobes, large inclusion-like nucleoli, and abundant cytoplasm, surrounded by lymphocytes, macrophages, and an eosinophil.
(B) Reed-Sternberg cell, mononuclear variant.
(C) Reed-Sternberg cell, lacunar variant. This variant has a folded or multilobated nucleus and lies within an open space, which is an artifact created by disruption of the cytoplasm during tissue sectioning.
(D) Reed-Sternberg cell, lymphohistiocytic variant. Several such variants with multiply infolded nuclear membranes, small nucleoli, fine chromatin, and abundant pale cytoplasm are present.
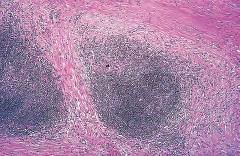
Figure: Hodgkin lymphoma, nodular sclerosis type. Low-power view shows well-defined bands of pink, acellular collagen that subdivide the tumor into nodules. Robbin’s Page 613
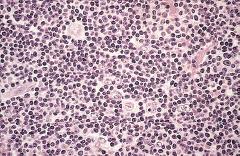
Figure: Hodgkin lymphoma, lymphocyte predominance type. Numerous mature-looking lymphocytes surround scattered, large, pale-staining lymphohistiocytic variants (popcorn cells). Robbin’s Page 613
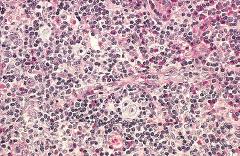
Figure: Hodgkin lymphoma, mixed-cellularity type. A diagnostic, binucleate Reed-Sternberg cell is surrounded by reactive cells including eosinophils (bright red cytoplasm), lymphocytes, and macrophages. Robbin’s Page 613
| Click here to Download the pdf version of Lymphoma |

Comments (0)