
Neoplasia
Some Terms Related to Neoplasia
|
Neoplasia means “new growth,” and the collection of cells and stroma composing new growths are referred to as neoplasms.
Tumor is originally described as swelling caused by inflammation. Cancer is the common term for all malignant tumors. Oncology (Greek oncos = tumor) is the study of tumors or neoplasms. |
Definition of Neoplasm:
According to British oncologist Sir Rupert Willis -
“A neoplasm is an abnormal mass of tissue, the growth of which exceeds and is uncoordinated with that of the normal tissues and persists in the same excessive manner after cessation of the stimuli which evoked the change.”
In the modern era, a neoplasm is defined as a genetic disorder of cell growth that is triggered by acquired or less commonly inherited mutations affecting a single cell and its clonal progeny. (Ref Robbin's 10th Edition)
Two components of neoplasm:
- Tumor parenchyma:
Formed by neoplastic cells - Reactive stroma:
Made up of connective tissue, blood vessels, and cells of the adaptive and innate immune system.
Note:
| Tumor classification and their biological behavior are based primarily on parenchymal components, but Growth and spread are depended on their stroma. |
Stromal Component of Neoplasm:
- Soft and fleshy:
Neoplasm is soft and fleshy when the stromal support is scant. - Desmoplasia:
When the parenchymal cells stimulate the formation of an abundant collagenous stroma, referred to as desmoplasia.
For example, some cancers of the female breast are stony hard or scirrhous (desmoplastic tumor).
Nomenclature of Tumor/Neoplasm
The nomenclature of tumors and their biological behavior are based primarily on - Parenchymal component.
Nomenclature of Benign Tumor:
1. Benign mesenchymal tumor:
Designated by attaching the suffix - oma to the cell from which the tumor arises.
Example of Benign mesenchymal tumor:
- Fibroma is a benign tumor arising in fibrous tissue (fibroblast).
- Lipoma is a benign tumor of fatty tissue.
- Chondroma is a benign cartilaginous tumor.
- Osteoma is a benign tumor arising from the bone.
Exception:
Example of malignant tumor with suffix Oma:
|
2. Benign epithelial tumor
They are classified based on their
- Cells of origin,
- Macroscopic architecture, and
- Microscopic pattern.
Example of Benign epithelial tumor:
- Adenoma
- Papilloma
- Polyp
Adenoma
An adenoma is a term applied to a benign epithelial neoplasm derived from glands, although they may or may not form glandular structures.
Example of adenoma:
- Adrenal adenoma
- Adenoma of renal tubular cells
- Pituitary adenoma
- Thyroid adenoma (Follicular adenoma)
- Hepatic adenoma
Papilloma:
Papilloma is a benign epithelial neoplasm producing finger-like or warty projections from epithelial surfaces are referred to as papilloma.
Example of papilloma:
- Squamous cell papilloma.
- Transitional cell papilloma
- Papillary cyst adenoma
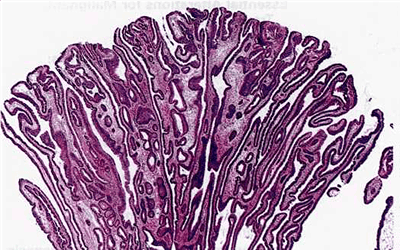
Figure: Papilloma of the colon with finger-like projections into the lumen
Polyp:
When a neoplasm, benign or malignant, produces a macroscopically visible projection above a mucosal surface and projects into the lumen, it is called a polyp.
Examples of polyp are Gastric polyp, Colonic polyp
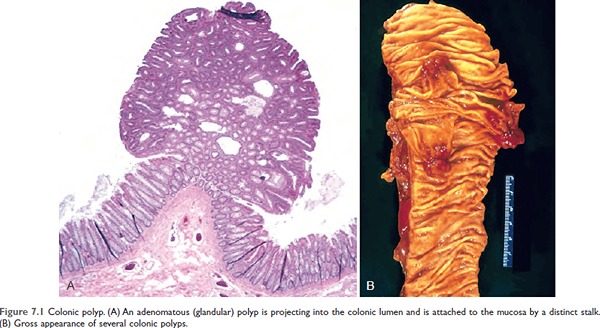
Figure 7.1 Colonic polyp. (A) An adenomatous (glandular) polyp is projecting into the colonic lumen and is attached to the mucosa by a distinct stalk.
(B) Gross appearance of several colonic polyps.
Nomenclature of Malignant Tumors
1. Sarcoma:
- Malignant tumors arising in solid mesenchymal tissue are usually called sarcomas (Greek sar = fleshy),
- They are fleshy as they have little connective tissue stroma.
Examples of sarcoma:
- Fibrosarcoma
- Liposarcoma
- Chondrosarcoma
- Osteosarcoma
- Whereas those arising from blood-forming cells are designated Leukemias (literally, white blood) or,
- Lymphomas (tumors of lymphocytes or their precursors).
2. Carcinoma:
Malignant neoplasms of epithelial cell origin, are called carcinomas.
Example of carcinoma:
- Adenocarcinoma (a malignant tumor of the glandular tissue)
- Squamous cell carcinoma
- Transitional cell carcinoma
| Carcinoma | Major Site Involved |
| Adenocarcinoma | Glands, stomach, intestine |
| Squamous cell carcinoma | Skin, esophagus, larynx |
| Transitional cell carcinoma | Urinary bladder, Renal pelvis |
Easy Naming Sequence
|
Benign
|
Malignant |
| Fibroma | Fibrosarcoma |
| Lipoma | Liposarcoma |
| Chondroma | Chondrosarcoma |
| Osteoma | Osteosarcoma |
| Benign | Malignant |
| Adenoma | Adenocarcinoma |
| Squmamos cell papilloma | Squamous cell carcinoma |
| Transitional cell papilloma | Transitional cell carcinoma |
Mixed tumor:
Divergent differentiation of a single neoplastic clone along two lineages creates a tumor called mixed tumors.
Example of mixed tumor:
Pleomorphic adenoma (Benign mixed tumor of the salivary gland) - which contains epithelial components scattered within a myxoid stroma that may contain islands of cartilage or bone.
| Benign | Malignant |
| Pleomorphic adenoma (Mixed tumor of the salivary gland) | Malignant mixed tumor of salivary gland |
Teratoma:
The tumor that arises from more than one germ layer, usually from all three germ layers is called a teratoma.
Example of Teratoma:
Ovarian cystic teratoma (Ovarian dermoid cyst), which differentiates principally along ectodermal lines to create a cystic tumor lined by skin, replete with hair, sebaceous glands, and tooth structures
| Site | Benign | Malignant |
| Totipotent cells in gonads | Mature Teratoma | Immature Teratoma |

Figure: Gross appearance of an opened cystic teratoma of the ovary. Note the presence of hair, sebaceous material, and a tooth.
Hamartomas:
Hamartomas are disorganized but benign-appearing masses composed of cells indigenous/native to the involved site.
An example of hamartoma is Pulmonary chondroid hamartoma (which contains islands of disorganized, but histologically normal cartilage, bronchi, and vessels).
Choristoma:
Heterotopic (misplaced) rest of cells producing tumor-like mass is called choristoma.
Choristoma is the ectopic island of normal tissue.
An example of choristoma is a small nodule of a well-developed and normally organized pancreatic substance, which may be found in the submucosa of the stomach, duodenum, or small intestine.
Difference between Hamartomas & Choristoma
| Hamartomas | Choristoma |
| Hamartomas are abnormally arranged tissue at the normal site. | Choristoma is normally arranged tissue at an abnormal site. |
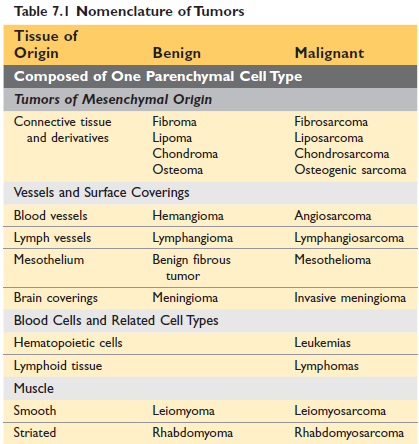
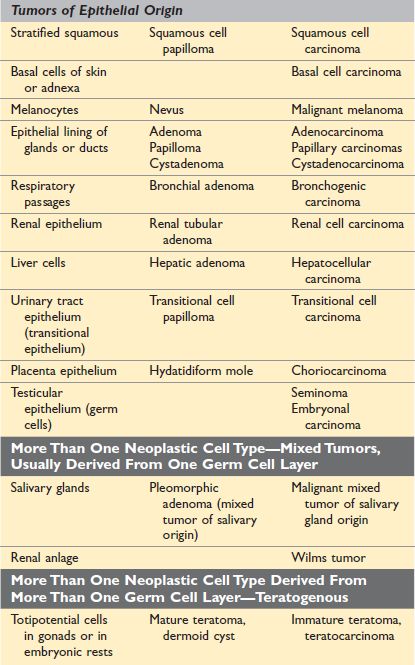
Figure: Nomenclature of tumor (Robbin's 10th Edition)
Basis of tumor classification
- Naked eye appearance and regional classification
- Histogenetic classification
- Histologic classification
- Classification according to behavior
- Aetiological classification
- Functional classification
A) Naked eye appearance and regional classification
- annular-like growth (ring-shaped)
- cauliflower-like growth
- tumor in the brain
- tumor in the intestine - scirrhous tumors are hard
- medullary tumors are soft
- mucoid tumors are mucin-like consistency
B) Histogenetic classification (i.e based on cell origin)
- Tumors of epithelial origin
- Tumors of connective tissue origin
Disadvantages of histogenetic classification
1. The nature of endothelium, mesothelium, and synovium – the endothelial and mesothelial cells although generally classified as connective tissue, may on occasion give rise to the tumor, which resembles those of epithelial origin.
2. Undifferentiated tumor - sometimes tumors are so poorly differentiated or undifferentiated that their cell of origin cannot be easily identified. (Now electron microscopy and immunohistochemistry solved this problem).
3. Tumor metaplasia - Adenosquamous carcinoma of the cervix.
4. Debatable origin of a tissue - when the precise origin of the cell is in doubt.
Example: Melanocytes of the skin
- Melanocytic sarcoma - neural origin
- Naevocarcinoma - epithelial origin
5. Origin from highly specialized tissue - though this is the mesenchymal origin, we don’t call them sarcoma.
- Hemopoietic tissue: Leukaemia, Lymphoma
- Glial tissue: Glioma
6. Origin from embryonic tissues - Some tumor arises from cells that are present during development but disappear in adult life.
Example: Embryonic tumors of infancy: Retinoblastoma, Neuroblastoma, Nephroblastoma
7. Origin from germ cells- Germ cells are totipotential and tumors derived from them can differentiate into any tissue of the body.
8. Origin from placental tissues- The Hydatidiform mole and choriocarcinoma are derived from chorionic tissue.
C) Histologic classification
A histological classification is used under the following conditions:
- When the tumor is so undifferentiated, as its site of origin is difficult to identify - small cell, large cell, giant cell, pleomorphic cell, and spindle cells are all self-explanatory.
- The occurrence of tumor metaplasia.
D) Classification according to behavior ***
- Benign
- Malignant
- Tumor of intermediate malignancy or locally malignant tumor
- Carcinoma in situ
- Latent cancer
- Dormant cancer
- Spontaneous regression
1. Benign tumor:
- These tumors are well differentiated,
- Do not invade surrounding tissue.
- They are usually capsulated and show expanding type of growth.
- Example: Fibroma, Lipoma, Adenoma, papilloma,
2. Malignant tumor:
- Some anaplasia is always present.
- Always invade surrounding tissue and metastasizes.
- Examples: Fibrosarcoma, Adenocarcinoma
|
Benign
|
Malignant |
| Fibroma | Fibrosarcoma |
| Lipoma | Liposarcoma |
| Chondroma | Chondrosarcoma |
| Osteoma | Osteosarcoma |
| Benign | Malignant |
| Adenoma | Adenocarcinoma |
| Squmamos cell papilloma | Squamous cell carcinoma |
| Transitional cell papilloma | Transitional cell carcinoma |
Differences between benign and malignant tumors:
| Characteristics | Benign | Malignant |
| Differentiation/anaplasia | Well-differentiated; structure sometimes typical of tissue of origin | Some lack of differentiation (anaplasia); the structure is often atypical |
| Rate of growth | Usually progressive and slow | Unpredictable and may be slow to rapid |
| Local invasion | Do not invade or infiltrate surrounding normal tissues | Locally invasive, and infiltrate & destroy surrounding tissue |
| Metastasis | Absent | Frequently present |
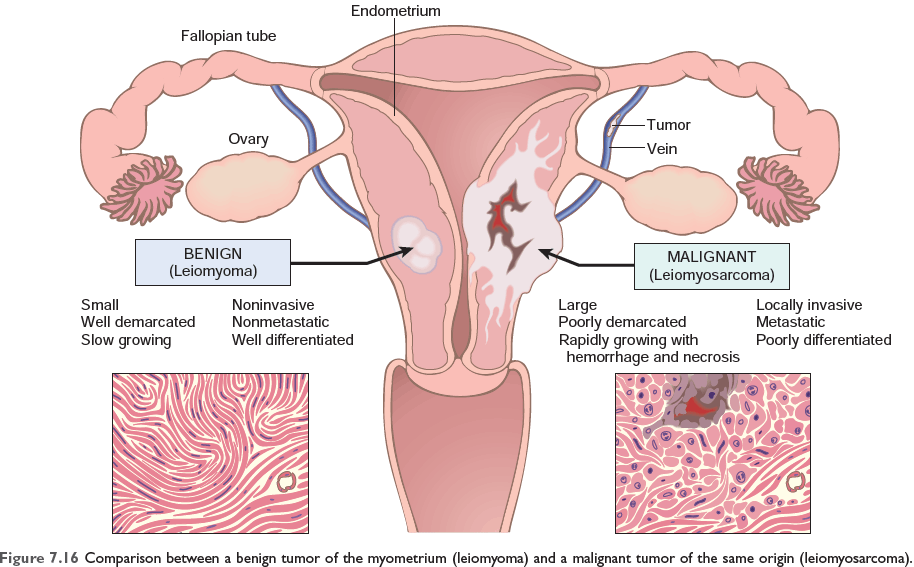
Figure 7.16 Comparison between a benign tumor of the myometrium (leiomyoma) and a malignant tumor of the same origin (leiomyosarcoma)
3. Tumor of intermediate malignancy or Locally malignant tumor:
They are locally invasive and therefore are not benign, but have little or no tendency to metastasize, so not malignant.
Example of locally malignant tumor:
- Ameloblastoma
- Basal cell carcinoma,
- Carcinoid tumor
- Craniopharyngeal tumor of the pituitary gland
- Glioma
- Giant cell tumor
4. Carcinoma in situ:
When dysplasia is severe and involves the full thickness of the epithelium but the lesion does not penetrate the basement membrane, it is referred to as carcinoma in situ.
The lesion has the cytological features of malignancy but does not penetrate the basement membrane.
Examples of carcinoma in situ are Carcinoma in situ of the skin, cervix, and breast.
5. Latent cancer:
The tumor which has all the histological characteristics of a malignant tumor, including sometimes lymphatic and vascular invasion but clinically remains silent is called latent cancer.
An example of latent cancer is Carcinoma of the prostate.
6. Dormant cancer:
This is the late appearance of metastasis after the primary tumor has been removed.
Example of dormant cancer:
- Carcinoma of breast
- Carcinoma of kidney
- Malignant melanoma
7. Spontaneous regression:
Cancer that has suddenly regressed spontaneously and permanently.
Example:
- Malignant melanoma
- Clear cell carcinoma of the kidney
- Choriocarcinoma
E) Aetiological classification:
- Viral origin
- Chemical origin
- Radiation origin
F) Functional classification:
According to the secretion of hormones:
Example: insulinoma (secrete insulin), glucagonoma
Favored classification
Based on:
- tissue of origin
- behavioral classification
Example:
- Lipoma (fat cell and benign)
- Liposarcoma (fat cell and malignant).
Biology of tumor growth:
The natural history of malignant tumors can be divided into four phases.
- Transformation: malignant change in target cells; differentiation and anaplasia
- Growth of transformed cells
- Local invasion
- Distant metastasis
Differentiation
Differentiation refers to the extent to which neoplastic parenchymal cells resemble the corresponding normal parenchymal cells both morphologically and functionally.
- Benign tumors are always well differentiated and
- Malignant tumors range from well to undifferentiated.
Anaplasia
Anaplasia means lack of differentiation; is a hallmark of malignancy.
Characteristics of anaplasia
A) Morphological point
1) Pleomorphism of cells and nucleus:
- Pleomorphism means, variation in size and shape.
- Cells are not uniform but range from the small cell with an undifferentiated appearance to tumor giant cells.
2) Abnormal nuclear morphology:
- The nuclei are disproportionately large for the cell,
- The nuclear-cytoplasmic ratio may approach to 1:1 instead of the normal 1:4 to 1:6.
- The nuclear shape is variable and often irregular
- The coarsely clumped nuclear chromatin is distributed along the nuclear membrane, or more darkly stained (hyperchromatic).
- Large nucleoli are usually present.
3) Mitosis: atypical & bizarre mitotic figures are present
- Frequent and abnormal. The nucleus is tripolar, quadripolar, or multipolar instead of normal bipolar.
4) Loss of polarity: Orientation is lost and grows in a disorganized haphazard fashion.
5) Other changes: Rapidly growing large tumors develop large areas of ischaemic necrosis.
B) Functional point:
Better differentiated tumor retains the functional capabilities.
Example:
- Well-differentiated Hepatocellular carcinoma elaborate bile,
- Well-differentiated Squamous cell carcinoma of the skin produces keratin.
- Some tumor cell produces ectopic hormones,
- Some produce fetal proteins.
Dysplasia
Dysplasia means disordered growth characterized by loss of uniformity as well as loss of architectural orientation of cells.
- It may progress to cancer or regress to a normal cell.
- It commonly occurs in the epithelium.
Sites of dysplasia are the Cervix of the uterus, the epidermis of the skin, the epithelium of the respiratory tract
- Dysplasia of cervix
- Dysplasia of skin
- Dysplasia of the urinary bladder
Carcinoma in situ:
When dysplastic changes are marked or severe and involve the entire thickness of the epithelium, the lesion is considered a preinvasive neoplasm and is called carcinoma in situ.
When it penetrates the basement membrane it becomes an invasive neoplasm.
Example of Carcinoma in situ: In Cervix, Breast, Skin
- Cervical Intraepithelial Neoplasia (CIN)
- Atypical endometrial hyperplasia
- Carcinoma in situ of the breast (Intraductal or Lobar CIN)
- Solar keratosis of the skin
- Leukoplakia of oral cavity, valva, penis
- Chronic atrophic gastritis of pernicious anemia
- Chronic ulcerative colitis
- Villous adenoma of the colon
- Cirrhosis of liver
Dysplasia to invasive carcinoma:
Example: In long-term cigarette smokers
Metaplasia of the bronchial epithelium (columnar to squamous)
↓
Dysplasia
↓
Carcinoma in situ
↓
Invasive squamous cell carcinoma.
Growth of transformed cells (rate of growth):
It is determined by 3 factors:
- the doubling time of tumor cells
- the fraction of dividing cells
- the rate of cell loss.
So, growth occurs if there is excess cell production over cell loss.
Local invasion:
The growth of cancers is accompanied by progressive infiltration, invasion, and destruction of the surrounding tissue, whereas nearly all benign tumors grow as cohesive expansile masses that remain localized to their site of origin and lack the capacity to infiltrate, invade or metastasize to distant sites.
Most benign tumors grow as cohesive expansile masses and develop a connective tissue capsule, so localized to their site of origin. They do not penetrate the capsule or the surrounding normal tissue so do not metastasize to distant sites.
Malignant neoplasms are invasive, infiltrating in a crab-like pattern and destroying surrounding normal tissues. Usually, capsules are absent.
Metastasis:
Metastasis is the tumor implant to the sites that are physically discontinuous with the primary tumor.
Metastasis can be defined as the spreading of the tumor to the sites that are physically discontinuous with the primary tumor.
- A benign tumor never metastasizes
- Metastasis is the hallmark of malignancy.
Routes of metastasis:
- Direct seeding of body cavities or surfaces
- Lymphatic spread
- Haematogenous spread
- Direct implantation
1. Seeding of body cavities and surfaces
- Occurs whenever a malignant neoplasm penetrates into a natural ‘open field’ lacking physiological barriers.
- Most often involve the peritoneal cavity. Pleural, pericardial, and subarachnoid spaces are also involved.
Example:
Sometimes mucus-secreting appendiceal carcinomas or ovarian carcinoma fill the peritoneal cavity with a gelatinous neoplastic mass referred to as pseudomyxoma peritonei.
Krukenberg's tumor is metastasis of carcinoma of the stomach to both ovaries transperitoneally.
2. Lymphatic spread
The Most common pathway for the initial dissemination of carcinoma is the lymphatic route.
The pattern of lymph node involvement follows the natural route of drainage.
Example of lymphatic spread of carcinoma
Carcinoma of the upper outer quadrant (UOQ) of the breast spread through the axillary lymph node (UOQ) and from the Inner quadrant of the breast, it spread through internal mammary lymph nodes.
Exception:
- Renal cell carcinoma (renal vein),
- Hepatocellular carcinoma (Hepatic artery)
Sentinel lymph node:
A sentinel lymph node is defined as the first node in a regional lymphatic basin that receives lymph flow from the primary tumor.
3. Haematogenous spread
Typically sarcoma but carcinoma also follows this route.
Veins are more commonly involved than arteries due to thinner walls.
The lung and liver are the sites of hematogenous metastasis because they receive systemic venous outflow.
4. Direct implantation:
Rarely occurs during surgical operation by the surgical instrument.
Epidemiology:
There are a number of factors relating to the patient and environment that influence predisposition to cancer.
- Cancer incidence
- Geographical and environmental factors
- Occupational factors
- Heredity factor
- Acquired preneoplastic disorder
- Age
The global impact of cancer
In 2018, it was estimated that number of new cases was about 9.5 million worldwide, leading to 7.6 million deaths (21,000 death /day). By 2030 it is projected that the number of cancer cases and cancer–related deaths will be increased to 21.4 million and 13.2 million respectively.
A) Cancer incidence:
An individual likelihood of developing cancer is expressed by the national incidence of mortality rate.
Common cancers based on incidence & mortality rate
| By incidence | By Mortality rate |
| 1. Breast/Prostate cancer | 1. Lung cancer |
| 2. Lung cancer | 2. Breast/Prostate cancer |
| 3. Colorectal cancer | 3. Colorectal cancer |
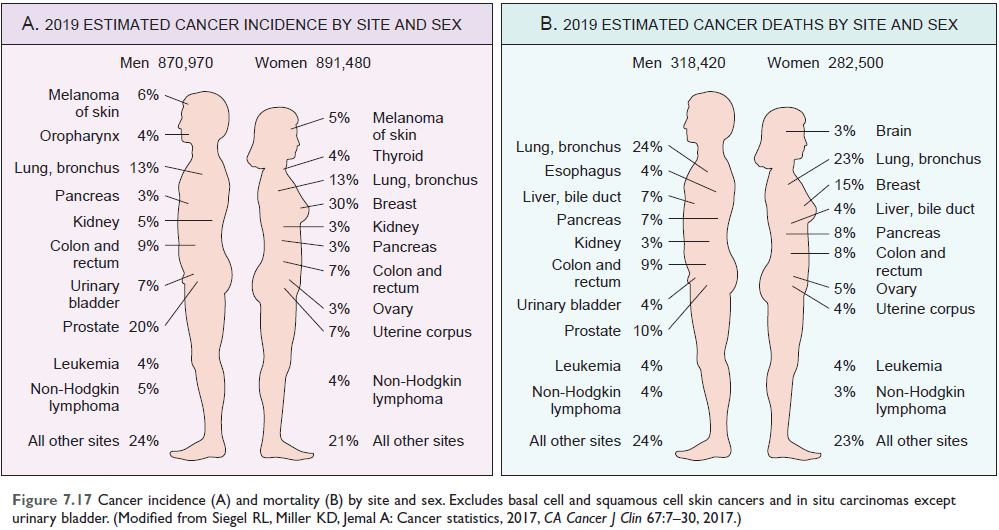
Figure: Cancer incidence and mortality by site and sex (Ref Robbin’s 10th Edition Page 277)
B) Environmental factors:
Although both genetic and environmental factors contribute to the development of cancer, environmental influences appear to be the dominant risk factors for most cancers.
Among the best-established environmental factors affecting cancer risk are the following:
- Infectious agents eg. Human Papilloma Virus (HPV)
- Smoking
- Alcohol consumption
- Diet
- Obesity
- Reproductive history
- Environmental carcinogens
Smoking:
Cigarettes have been implicated in cancer of the mouth, pharynx, larynx, esophagus, pancreas, bladder and most significantly, about 90% of lung cancer deaths.
Alcohol consumption:
Increase the risk of carcinoma of the oropharynx (excluding lip), larynx, and esophagus and hepatocellular carcinoma,
Alcohol and tobacco together increase the risk of cancer in the upper airway and digestive tract.
Reproductive history:
Life-long exposure to estrogen unopposed by progesterone, increase the risk of breast and endometrial cancer.
Geographical:
- Stomach cancer in Japan is 7-8 times higher than that in the USA
- Lung cancer in USA is more than twice as in Japan
- Skin cancer is 6 times more frequent in New Zealand than in Iceland
The change in the incidence of various cancers with migration from Japan to the United States
C. Occupational factors:
- In sun exposure – skin cancer (malignant melanoma)
- Smoker- cancer in airway tract including lung, digestive tract (mouth, pharynx, esophagus, pancreas), UB
- Alcoholic - GIT cancer
Occupational cancers:
- Arsenic and arsenic compound: Lung carcinoma, skin carcinoma
- Asbestos labor: Bronchogenic carcinoma
- Benzene: AML
- β-naphthalene labor: Urinary bladder cancer
- Cadmium: Prostate cancer
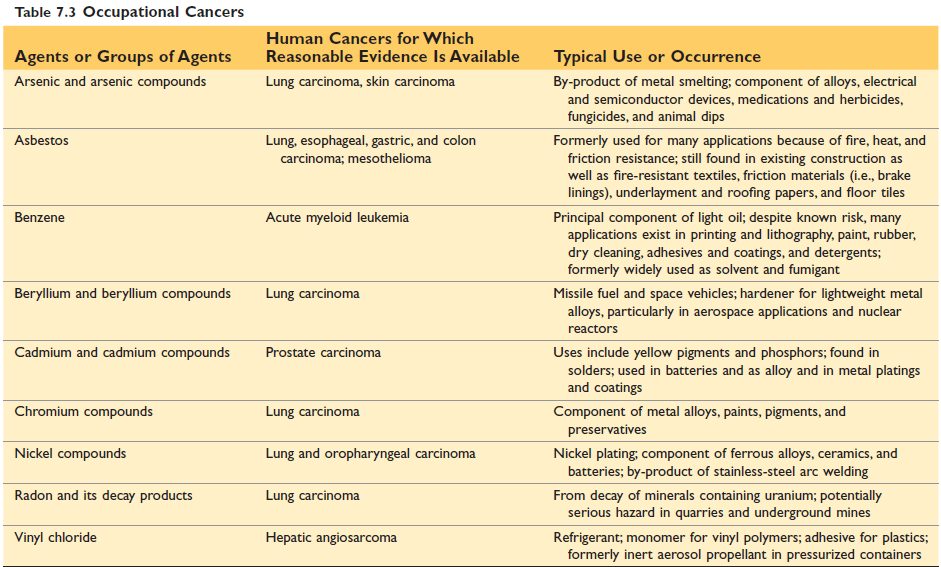
Figure: Occupational cancers (Ref Robbin’s 10th Edition Page 280)
Genetic predisposition and interactions between environmental and Heredity factors:
Genetic predisposition can be divided into three categories:
- Autosomal dominant inherited cancer syndrome
- Familial cancer
- Autosomal recessive syndrome of defective DNA repair
D. Heredity factors:
a) Autosomal dominant inherited cancer syndromes - inheritance of a single mutant gene increases the risk of cancer.
Example:
- Familial retinoblastoma
- Familial adenomatous polyps of the colon
- Multiple endocrine neoplasia syndromes
- Neurofibromatosis type1 &2
- Von- Hippel - Lindau syndrome.
b) Familial cancer are Breast cancer, Ovarian cancer, Pancreatic cancer, colon cancer, Brain cancer,
c) Autosomal recessive syndromes of defective DNA repair-
- Xeroderma pigmentosum
- Ataxia telengiectasia
- Bloom’s syndrome
- Fanconi anemia
Acquired predisposing condition:
Acquired conditions that predispose to cancer can be divided into
- chronic inflammations,
- precursor lesion, and
- immunodeficiency states.
Acquired preneoplastic disorder:
1) Non-neoplastic disorders-
- Chronic atrophic gastritis of pernicious anemia
- Solar keratosis of the skin
- Chronic ulcerative colitis
- Leukoplakia of the oral cavity, vulva, and penis
2) Benign tumors-
- Villous adenoma of colon
- Neurofibroma, Leiomyoma
- Pleomorphic adenoma
3) Dysplasia-
- Dysplasia of cervix
- Dysplastic changes of skin and urinary bladder
- Dysplasia of bronchial epithelium
4) Metaplasia: Columnar metaplasia of the esophagus
5) Hyperplasia
- Endometrial Hyperplasia
- Lobular and ductal Hyperplasia of the breast, Cirrhosis of the liver.
Chronic inflammatory States & Cancer
| Pathological condition | Associated neoplasm | Etiological agent |
| Asbestosis, silicosis | Mesothelioma, lung carcinoma | Asbestos fibers, silica particles |
| Inflammatory bowel disease | Colorectal carcinoma | |
| Lichen sclerosis | Vulvar squamous cell carcinoma | |
| Pancreatitis | Pancreatic carcinoma | Alcoholism, germline mutations (e.g in trypsinogen gene) |
| Chronic cholecystitis | Gall bladder cancer | Bile acids, bacteria. Gall stones |
| Reflux esophagitis, Barrett esophagus |
Esophageal carcinoma | Gastric acid |
| Sjogren syndrome, Hashimoto thyroiditis |
MALT lymphoma | |
| Opisthorchis, cholangitis | Cholangiocarcinoma, Colon carcinoma |
Liver flukes (opisthorchis viverrini) |
| Gastritis/Ulcers | Gastric adenocarcinoma, MALT Lymphoma |
Helicobacter Pylori |
| Hepatitis |
Hepatocellular carcinoma | Hepatitis B And/or C virus |
| Osteomyelitis | Carcinoma in draining sinuses | Bacterial infection |
| Chronic cervicitis | Cervical carcinoma | HPV |
| Chronic cystitis | Bladder carcinoma | Schistosomiasis |
(Ref Robbin’s 10th Edition (Table 7.4) Page 281)
F) Age:
Cancer is more common after 55 years of age.
Certain cancers are particularly common in children under 15 years of age.
- Retinoblastoma
- Neuroblastoma,
- Nephroblastoma or Wilm’s tumor of kidney
- Hepatoblastoma
- Acute leukemia,
- Lymphoma
- Osteosarcoma
- Embryonal rhabdomyosarcoma
0 to 4 Years
- Leukemia
- Retinoblastoma
- Neuroblastoma
- Wilms tumor
- Hepatoblastoma
- Soft-tissue sarcoma (especially rhabdomyosarcoma)
- Teratomas
- Central nervous system tumors
5 to 9 Years
- Leukemia, Retinoblastoma, Neuroblastoma
- Hepatocellular carcinoma
- Soft-tissue sarcoma
- Central nervous system tumors
- Ewing sarcoma
- Lymphoma
10 to 14 Years
- Hepatocellular carcinoma
- Soft-tissue sarcoma, Osteogenic sarcoma
- Thyroid carcinoma,
- Hodgkin's disease

Comments (0)