Mediators of Inflammation
Inflammatory mediators are the substances that initiate and regulate inflammatory reactions.
Chemical mediator:
General Principles
- Mediators originate from plasma or from cells
- Production of active mediators is triggered by microbial products or by host proteins, such as complement, kinin, and coagulation systems.
- Mediate activity by
-
- Binding to specific receptors on target cells.
- Direct enzymatic activity.
- Oxidative damage
- Chemical mediators can stimulate the release of other mediators by target cells themselves.
- Once activated and released from the cell the mediators are short-lived.
- Mediators have the potential to cause harmful effects.
Classification of Chemical mediators:
A) According to the source:
- Cell-derived
-
- Pre-formed
- Newly synthesized
- Plasma-derived
B) According to chemical nature:
1. Vasoactive Amines: Histamine and serotonin
2. Plasma protease:
- Clotting system
- Complement system
- Kinins: Bradykinin (principle vasoactive amine)
3. Arachidonic acid metabolites (Eicosanoids)
- Leukotrienes LTB4, LTC4, LTD4, LTE4.
- Prostaglandins
- Lipoxin
4. Platelet Activating Factor (PAF)
5. Cytokines & chemokines
- Interleukin 1 (IL-1)
- Tumor necrosis factor (TNF)
6. NO
7. Lysosomal enzymes
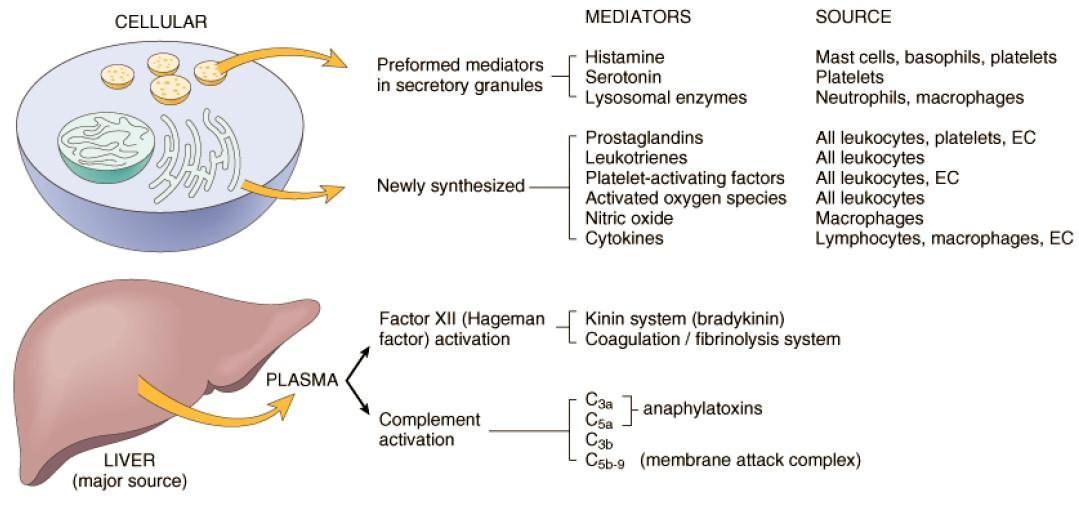
FIGURE: Chemical mediators of inflammation (According to source) [Source: 7th edition, Robbin’s]
Principle mediators of inflammation:
CELL-DERIVED mediators of inflammation
| Mediator | Principal Sources | Actions |
| Histamine | Mast cells, basophils, platelets | Vasodilation, increased vascular permeability, endothelial activation |
| Serotonin | Platelets | Vasodilation, increased vascular permeability |
| Prostaglandins | Mast cells, leukocytes | Vasodilation, pain, fever |
| Leukotrienes | Mast cells, leukocytes | Increased vascular permeability, chemotaxis, leukocyte adhesion and activation |
| Platelet-activating factor | Leukocytes, mast cells | Vasodilation, increased vascular permeability, leukocyte adhesion, chemotaxis, degranulation, oxidative burst |
| Reactive oxygen species | Leukocytes | Killing of microbes, tissue damage |
| Nitric oxide | Endothelium, macrophages | Vascular smooth muscle relaxation, killing of microbes |
| Cytokines (TNF, IL-1, IL-6) |
Macrophages, endothelial cells, mast cells | Local: Endothelial activation (expression of adhesion molecules). Systemic: Fever, metabolic abnormalities, hypotension(shock) |
| Chemokines | Leukocytes, activated macrophages | Chemotaxis, leukocyte activation |
PLASMA PROTEIN–DERIVED mediators of inflammation
| Mediator | Principal Sources | Actions |
| Complement products (C5a, C3a, C4a) | Plasma (produced in the liver) | Leukocyte chemotaxis and activation, vasodilation (mast cell stimulation) |
| Kinins | Plasma (produced in the liver) | Increased vascular permeability, smooth muscle contraction, vasodilation, pain |
| Proteases activated during coagulation | Plasma (produced in the liver) | Endothelial activation, leukocyte recruitment |
Vasoactive Amines: Histamine, serotonin
Vasoactive amines are so named because they have important actions on blood vessels. They are stored as preformed molecules in cells and are therefore among the first mediators to be released during inflammation.
Histamine:
Source of histamine: Mast cell, Basophils, Platelets
The function of histamine:
- Arteriolar dilation
- Increased permeability of venules (Principal mediator; producing inter-endothelial gaps)
- Constrict large arteries
Stimulation for degranulation of mast cell:
- Physical injury trauma, cold, heat
- Immune reactions/Immediate hypersensitivity (allergic) reaction (Binding of antigen to IgE antibody which is bounded to mast cells)
- Anaphylatoxin (C3a, C3b)
- Histamine releasing protein
- Neuropeptides Eg: Substance P
- Cytokines (IL-1, IL-8)
Serotonin (5-hydroxytryptamine)
- Serotonin (5-hydroxytryptamine) is a pre-formed vasoactive amine
- Actions similar to those of histamine.
- It is present in Platelets and enterochromaffin cells and (in mast cells in rodents but not in humans.)
Arachidonic acid metabolites (Eicosanoids):
Arachidonic acid is 20 carbons polyunsaturated fatty acid (5, 8, 11, 14-eicosatetraenoic acid) that is derived from a dietary sources or by conversion of essential fatty acid Linoleic acid.
Arachidonic acid metabolites
- Prostaglandins
- PGE2, PGD2, PGF2α, PGI2 (prostacyclin), and TxA2 (thromboxane)
- Leukotrienes
- LTB4
- LTC4, LTD4, LTE4
- Lipoxins
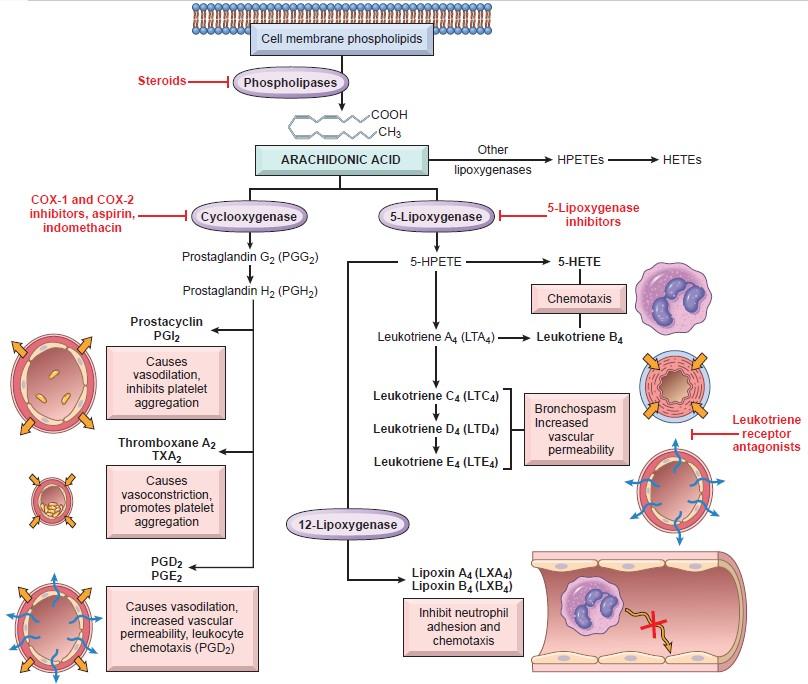
Figure: Production of arachidonic acid metabolites & their role in inflammation Robbin's 10th edition (Page 87)
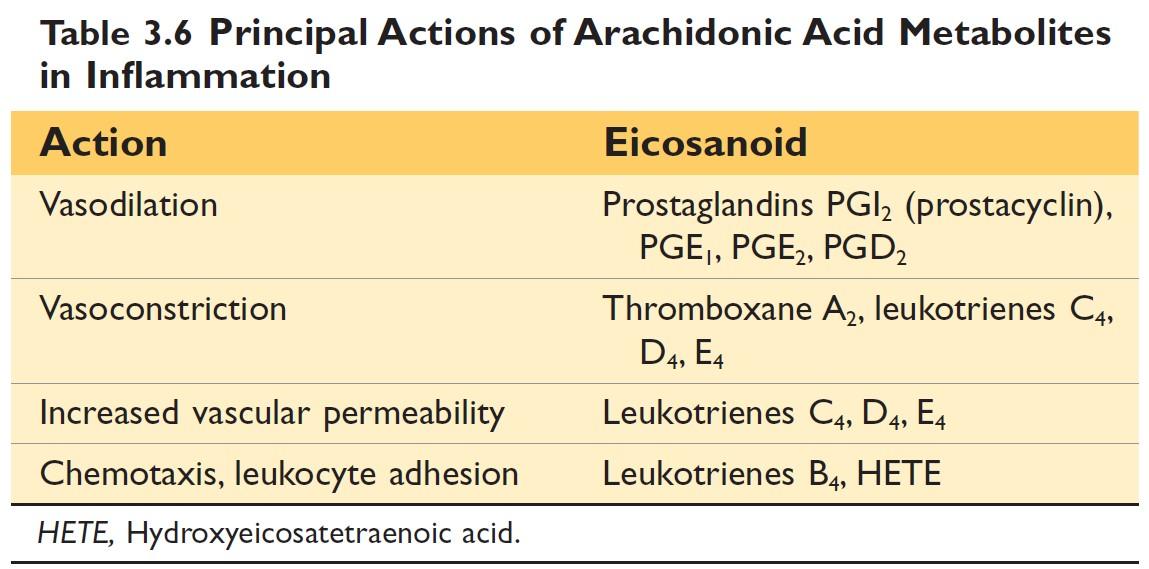
AA-derived mediators, also called eicosanoids (because they are derived from 20-carbon fatty acids; Greek eicosa = 20), are synthesized by two major classes of enzymes: cyclooxygenases (which generate prostaglandins) and lipoxygenases (which produce leukotrienes and lipoxins)
Prostaglandins Role in Inflammation:
- PGD2 & PGE2:
- Vasodilation and increases the permeability, potentiating edema formation. - PGD2: Also a chemoattractant for neutrophils.
- PGF2: Contraction of uterine and bronchial smooth muscle and small arterioles.
Prostaglandins are also involved in the pathogenesis of pain and fever in inflammation.
- PGI2 (Prostacyclin)
- Vasodilation, increase vascular permeability, potent inhibitor of platelet aggregation, and has chemotactic effects on other mediators. - TxA2 (Thromboxane)
- Platelet-aggregation and vasoconstriction.
Leukotrienes Role in Inflammation:
- LTB4:
- Chemotaxis
- Activator of neutrophils, causing aggregation and adhesion of the cells to venular endothelium, generation of ROS, and release of lysosomal enzymes. - LTC4, LTD4, LTE4:
- Vasoconstriction, bronchospasm (important in asthma), and increased vascular permeability.
Lipoxin Role in Inflammation: Inhibitors of inflammation
- Inhibit leukocyte recruitment and the cellular components of inflammation.
- They inhibit neutrophil chemotaxis and adhesion to endothelium.
- Play a role in the resolution of inflammation
(lipoxins may be endogenous negative regulators of leukotrienes).
Inflammatory actions of eicosanoids
Pharmacologic Inhibitors of Prostaglandins and Leukotrienes
- Cyclooxygenase inhibitors include aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- Lipoxygenase inhibitors
- Corticosteroids are broad-spectrum anti-inflammatory agents
- Leukotriene receptor antagonists
- Another approach to manipulating inflammatory responses by increasing the consumption of fish oil for the production of anti-inflammatory lipid products, including lipids called resolvins.
Cytokines:
Cytokines are proteins produced by many cell types that modulate the function of other cells type. Eg: IL-1, TNF.
Source of cytokines:
Lymphocytes, macrophages, dendritic cells, endothelium, epithelium & connective tissue cells.
Function of cytokines:
- Stimulate acute phase protein synthesis
- Stimulate endothelial cells
- Stimulate fibroblast
- Stimulate leukocytes
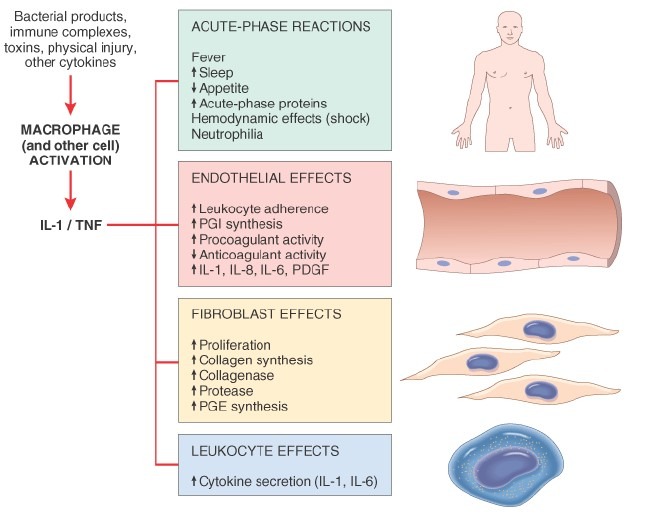
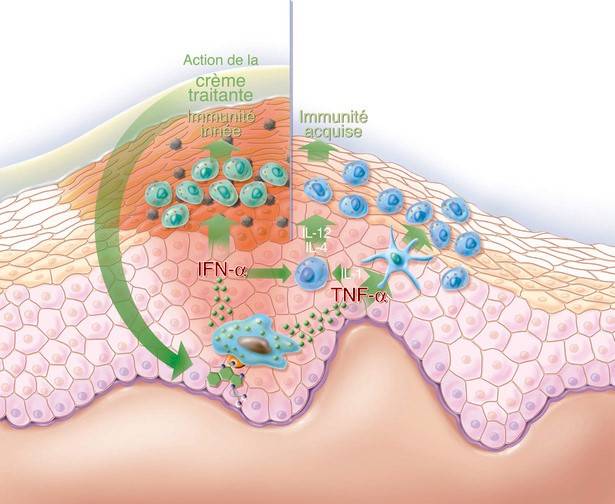
Figure: Major effects of interleukin-1 (IL-1) and tumor necrosis factor (TNF) in inflammation. (Source: Robbin’s 7th Edition)
Cytokines in Inflammation:
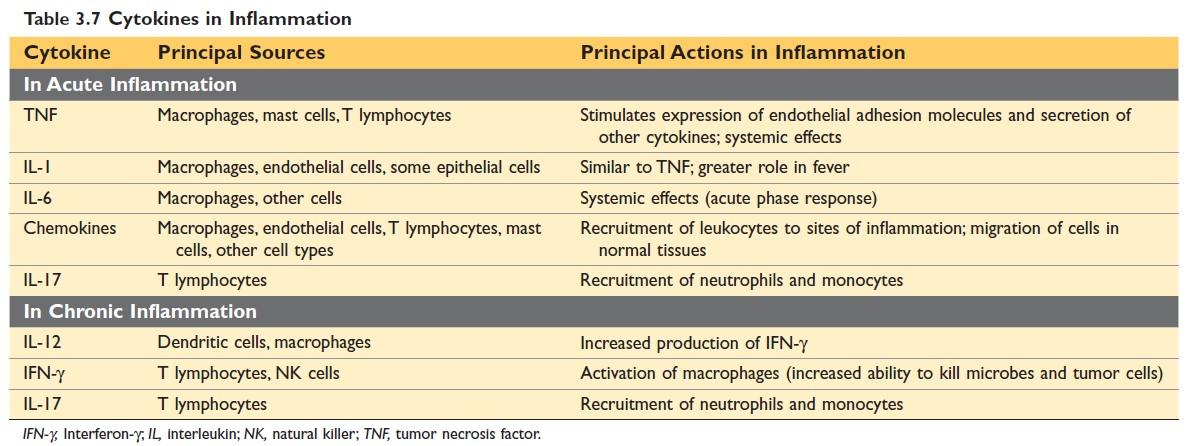
Figure: Cytokines in Inflammation Source: Robbin’s 10th Edition
Chemokines
Chemokines are a family of small (8 to 10 kD) proteins that act primarily as chemoattractants.
Chemokines have two main functions:
- Stimulate leukocyte recruitment in inflammation and
- control the normal migration of cells through various tissues.
Nitric oxide:
NO or endothelium-derived relaxing factor because it causes vasodilation by relaxing vascular smooth muscle.
- Synthesis of Nitric oxide: From L-arginine by the enzyme nitric oxide synthase (NOS)
- Source of Nitric oxide: Endothelial cells (eNOS), Macrophages, Neurons
- The function of Nitric oxide:
- Vasodilation
- Reduced platelets aggregation and adhesion
- NO, and its derivatives are microbicidal.
Platelet-activating factor:
PAF is a phospholipid-derived mediator. Its name was initially discovered as a factor derived from antigen-stimulated, IgE-sensitive basophils that cause platelet aggregation, so name the PAF.
Source: All leukocytes, Endothelial cells.
The function of Platelet-activating factor:
- Platelet aggregation
- Vasoconstriction
- Bronchospasm
- Vasodilation at extremely low concentration, &
- Increase venular permeability (potency 100 to 10,000 times greater than that of histamine)
- Leukocyte adhesion, chemotaxis, degranulation & the oxidative burst.
- Stimulate the synthesis of other mediators, eg- eicosanoids.
Lysosomal constituents of leukocytes:
Source: Neutrophils & monocytes (within lysosomal granules)
Granules of neutrophils: two types
| The smaller specific (or secondary) granules: | The large azurophil (or primary) granules: |
| Lysozyme, Lactoferrin, Collagenase, Gelatinase, Histaminase, Plasminogen activator, Alkaline phosphatase. | Lysozyme, Lactoferrin, Collagenase, Gelatinase, Histaminase, Plasminogen activator, Alkaline phosphatase. |
Monocyte & macrophage (Act in chronic inflammation):
- Acid hydrolases
- Collagenase, elastase, phospholipase &
- Plasminogen activators.
Plasma proteins
Complement systems:
Activation of complement:
1. The Classical pathway-
- triggered by fixation of C1 to antigen-antibody complex
2. The Alternate pathway-
- triggered by microbial surface products (endotoxin, or LPS), complex polysaccharides, and cobra venom.
3. The Lectin pathway-
- plasma mannose-binding lectin binds to carbohydrates on microbes and directly activates C1.
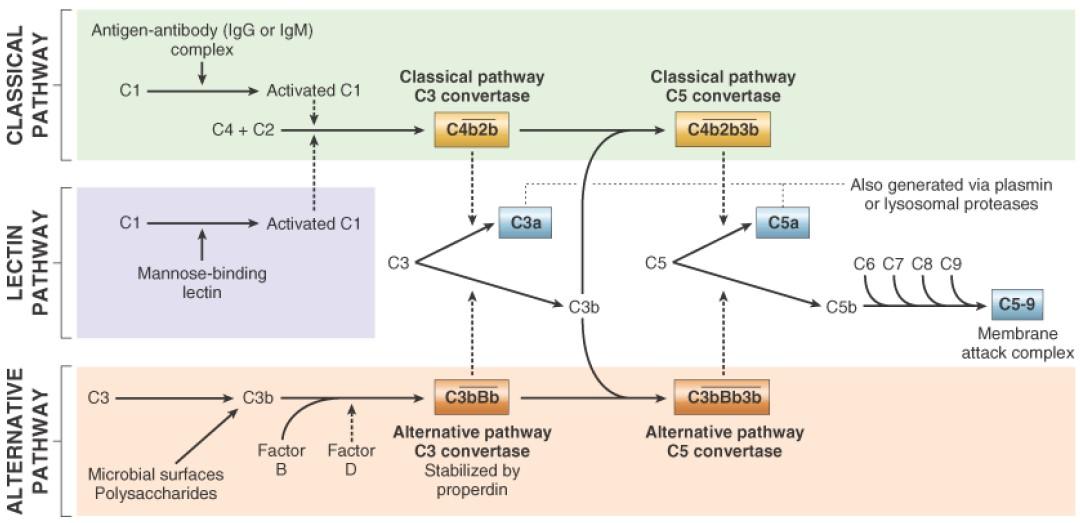
Figure: Activation and function of complement system Robbin’s 7th Edition
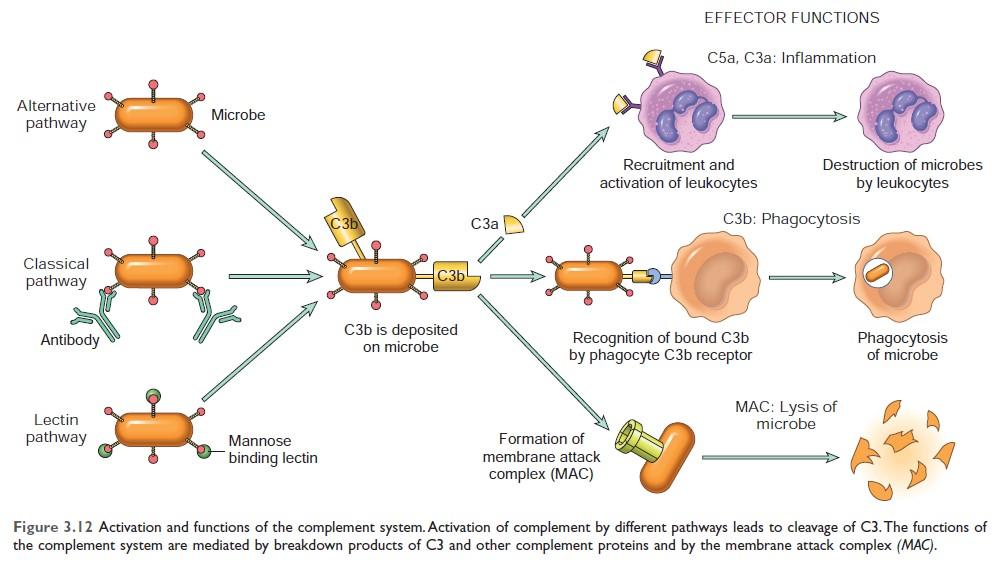
Figure: Activation and function of complement system Source: Robbin’s 10th Edition (Page 91)
Complement systems: The biological functions
A. Inflammation: C3a, C5a, and, to a lesser extent C4a,
- Increase vascular permeability and cause vasodilation. (called anaphylatoxins).
- C5a is a powerful chemotactic agent.
- C5a activates the lipoxygenase pathway of AA metabolism.
B. Opsonization & phagocytosis: C3b and iC3b (inactive C3b), act as an opsonin and promote phagocytosis.
C. Cell lysis: The deposition of the MAC on cells makes these cells permeable to water and ions and results in the death (lysis) of the cells.
Bradykinin Function:
- Increases vascular permeability
- Contraction of smooth muscle
- vasodilatation
- Causes pain.
Kallikrein Function:
- Potent activator of Hagemen factor.
- Has chemotactic activity
- Converts C5 to the C5a
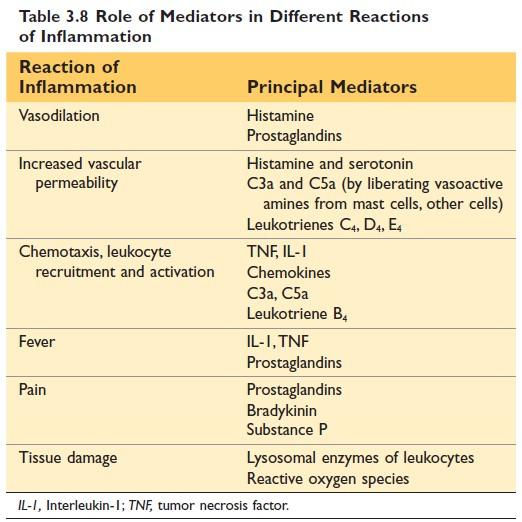
Figure: Role of mediator in inflammation

Comments (0)