Growth disturbance and adaptive changes
Objectives:
- Cellular responses to injurious stimuli.
- Define cellular adaptation.
- List the different types of cellular adaptations.
- Describe the pathogenesis and morphological features of different types of cellular adaptations.
Cellular Responses to Stress and Noxious Stimuli
 FIGURE 1- Stages in the cellular response to stress and injurious stimuli.
FIGURE 1- Stages in the cellular response to stress and injurious stimuli.
Cellular Responses to Injury
|
Nature of Injurious Stimulus |
Cellular Response |
|
ALTERED PHYSIOLOGICAL STIMULI; SOME NONLETHAL INJURIOUS STIMULI |
CELLULAR ADAPTATIONS |
|
Increased demand, increased stimulation (e.g., by growth factors, hormones) |
Hyperplasia, hypertrophy
|
|
Decreased nutrients, decreased stimulation Chronic irritation (physical or chemical |
Atrophy Metaplasia |
|
REDUCED OXYGEN SUPPLY; CHEMICAL INJURY; MICROBIAL INFECTION |
CELL INJURY |
|
Acute and transient
Progressive and severe (including DNA damage) |
Acute reversible injury Irreversible injury ? cell death |
|
METABOLIC ALTERATIONS, GENETIC OR ACQUIRED; CHRONIC INJURY |
INTRACELLULAR ACCUMULATIONS; CALCIFICATION |
|
CUMULATIVE SUBLETHAL INJURY OVER LONG LIFE SPAN |
CELLULAR AGING |
Cellular Adaptation
Definition:
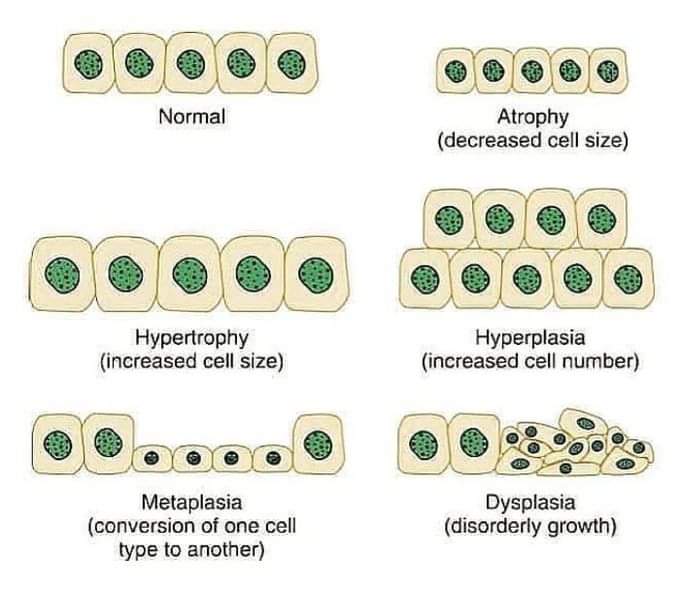
Adaptations are reversible changes in the size, number, phenotype, metabolic activity, or functions of cells in response to changes in their environment.
Source: Robbin’s Pathology10th edition
Type of Cellular Adaptation:
- Hyperplasia
- Hypertrophy
- Metaplasia
- Atrophy
Hyperplasia:
Hyperplasia is an increase in the number of cells in an organ or tissue in response to a stimulus.
- Note: Hyperplasia takes place in cells that undergo mitotic division; by contrast, hypertrophy involves cell enlargement without cell division.
Types of Hyperplasia
- Physiologic hyperplasia
- Hormonal
- Compensatory
- Pathologic hyperplasia
- A) Physiologic hyperplasia
- Hormonal:
- Breast: proliferation of the glandular epithelium of the female breast at puberty and during pregnancy in response to estrogen and progesterone.
- Uterus: pregnant uterus in response to estrogen.
- Compensatory hyperplasia
Example:
- Liver: Compensatory hyperplasia of the liver after partial hepatectomy.
- Kidney: Compensatory hyperplasia of the remaining kidney after unilateral nephrectomy.
- B) Pathologic Hyperplasia:
Example:
- Endometrial hyperplasia: due to excessive stimulation by estrogen.
- Benign prostatic hyperplasia: in response to Androgen.
Importance of pathological hyperplasia:
Constitute a fertile soil for malignant transformation.
Mechanisms
- Hyperplasia is the result of growth factor driven proliferation of mature cells (after partial hepatectomy) and
- in some cases, by increased output of new cells from tissue stem cells (hepatitis, where proliferative capacity is compromised).
- After partial hepatectomy, growth factors are produced in the liver that engage receptors on the surviving cells and activate signaling pathways that stimulate cell proliferation.
- If the proliferative capacity of the liver is compromised (as in hepatitis), hepatocytes can instead regenerate from intrahepatic stem cells.
Role of growth factors
- The roles of growth factors and stem cells in cellular replication and tissue regeneration

Fig: Liver regeneration by the proliferation of hepatocyte.
Role of growth factors
- Hyperplasia is generally caused by-
- increased local production of growth factors,
- increased levels of growth factor receptors on the responding cells, or
- activation of particular intracellular signaling pathways.
Mechanism of Hyperplasia from last edition
All these changes lead to production of transcription factors that turn on many cellular genes, including genes encoding growth factors, receptors for growth factors, and cell cycle regulators, and the net result is cellular proliferation.
Hypertrophy
Definition:
Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ.
Hypertrophied organ has -
- No new cells, just larger cells.
- The increased size of the cells is due to the synthesis of more structural components.
- Nuclei in hypertrophied cells may have a higher DNA content than in normal
Type of Cells that undergo Hypertrophy and hyperplasia:
- Cells capable of division may respond to stress by undergoing both hyperplasia (described below) and hypertrophy,
- whereas in nondividing cells (e.g., myocardial fibers) increased tissue mass is due to hypertrophy.
- In many organs hypertrophy and hyperplasia may coexist and contribute to increased size (Uterus, breast).
Hypertrophy:
- Types: Physiologic
Pathologic
General Cause: increased functional demand or by stimulation by hormones and growth factors.
1) Physiological:
- Muscle hypertrophy due to increased workload.
- Uterus (myometrium): during pregnancy in response to oestrogen.
2) Pathological:
- Left ventricular hypertrophy:
due to chronic haemodyanamic overlode caused by Hypertension or faulty heart valves.
Mechanisms of Hypertrophy
- Hypertrophy is the result of increased production of cellular proteins.
- Hypertrophy results from the action of growth factors and direct effects on cellular proteins
There are three basic steps in the molecular pathogenesis of cardiac hypertrophy--
- Hypertrophy can be induced by the integrated actions of mechanical sensors, growth factors and vasoactive agents. Mechanical sensors themselves induce production of growth factors and agonists
- mechanical sensors (triggered by increased work load),
- growth factors (including TGF-β, insulin-like growth factor-1 [IGF-1], fibroblast growth factor),
- vasoactive agents (such as α-adrenergic agonists, endothelin-1, and angiotensin II).
2) These signals originating in the cell membrane activate a complex web of signal transduction pathways.
(Two such pathways are phosphoionositide 3 kinase (PI3K)/ AKT pathway (Physiological) and signaling downstream of G protein-coupled receptors (pathological)
3) These signaling pathways activate a set of transcription factors such as GATA4, nuclear factor of activated T cells (NFAT), and monocyte enhance factor 2(MEF2). These stimuli work coordinately to increase the synthesis of muscle proteins that are responsible for the hypertrophy.
Atrophy:
- Definition: Atrophy is reduced size of an organ or tissue due to a decrease in cell size and number.
- Types of Atrophy:
- Physiological: Common in early childhood.
- Notochord and thyroglossal duct, undergo atrophy during fetal development.
- The uterus decreases in size after parturition
- Pathological:
Depends on the underlying cause and can be generalized or localized.
Atrophy (Causes):
Causes of atrophy are the following:
- Decreased workload (atrophy of disuse)
- Loss of innervation
- Diminished blood supply
- Inadequate nutrition
- Loss of endocrine stimulation
- Aging
- Pressure
- Decreased workload (atrophy of disuse):
When a broken limb is immobilized in a plaster cast or when a patient is restricted to complete bed rest, skeletal muscle undergo rapid atrophy.
- Loss of innervation (denervation atrophy):
Damage to the nerves leads to rapid atrophy of the muscle fibers supplied by those nerves.
- Diminished blood supply:
The brain may undergoes progressive atrophy, due to atherosclerosis narrows its blood supply (senile atrophy)
- Inadequate nutrition:
Protein-calorie malnutrition (marasmus) is associated with the marked skeletal muscle wasting.
- Loss of endocrine stimulation:
Physiologic atrophy of the endometrium, vaginal epithelium, and breast due to loss of estrogenic stimulation after menopause.
- Aging (senile atrophy):
The aging process is associated with cell loss, typically seen in tissues containing permanent cells, particularly the brain and heart.
- Pressure:
Tissue compression for any length of time can cause atrophy. An enlarging benign tumor can cause atrophy in the surrounding compressed tissues.
Mechanism of Atrophy
- Atrophy results from decreased protein synthesis and increased protein degradation in cells.
- The degradation of cellular proteins occurs mainly by the ubiquitin- proteasome pathway.
- Activated ubiquitin ligases, attach the small peptide ubiquitin to cellular protein and target these proteins for degradation in proteasome.
Autophagy and heterophagy
- Autophagy (self eating):
- the process in which the starved cell eats own components to reduce nutrition demand to match the supply.
- Autophagic vacuoles:
- These are membrane-bound vacuoles within the cell that contain fragments of cell components (e.g., mitochondria, endoplasmic reticulum) into which the lysosomes discharge their hydrolytic contents.
Brown Atrophy:
- When atrophy is accompanied by increased autophagy, marked by the appearance of increased number of autophagic vacuoles.
Some of the cell debris within the autophagic vacuole may resist digestion and persist as membrane bound residual bodies in the cytoplasm. An example of such residual Bodies is the lipofuscin granules. When present in sufficient amounts, they impart a brown discoloration to the tissue known as brown atrophy.

Metaplasia:
Definition:
Metaplasia is a reversible change in which one differentiated cell type (epithelial or mesenchymal) is replaced by another cell type.
Type:
- A) Epithelial metaplasia
- Columnar to squamous: (Squamous metaplasia)
- Squamous to columnar: (Columnar metaplasia)
- B) Mesenchymal metaplasia
Squamous metaplasia
- In the respiratory tract (Trachea and bronchus):
Normal ciliated columnar epithelium of trachea and bronchus is replaced by stratified squamous epithelium in habitual smoker in response to chronic irritation.
- Salivary glands, pancreas, or bile ducts:
Stone may cause replacement of the normal secretory columnar epithelium by stratified squamous epithelium.
- 3. A deficiency of vitamin A (retinoic acid) induces squamous metaplasia in the respiratory epithelium.
- Cervix: Columnar to squamous in endocervical glands.
- Renal pelvis: Transitional to squamous.

Columnar metaplasia:
Columnar metaplasia: Metaplasia from squamous to columnar type.
Example: occur in Barrett esophagus, in which the esophageal squamous epithelium is replaced by intestinal-like columnar cells under the influence of refluxed gastric acid.
Connective tissue metaplasia:
Formation of cartilage, bone, or adipose tissue (mesenchymal tissues) in tissues that normally do not contain these elements.
- Example,
- Myositis ossificans: bone formation in muscle, occasionally occurs after bone fracture.
- Osseous metaplasia: in costal and thyroid cartilage in aging process.
Metaplasia:
- Importance:
- Metaplastic cells are capable to survive in adverse situation.
- If the influences persistent, may induce malignant transformation in metaplastic epithelium.
Mechanism
- Metaplasia is the result of reprogramming of stem cells that are known to exist in normal tissue or of undifferentiated mesenchymal cells present in connective tissue.
Hyperplasia & Hypertrophy Difference
- Hyperplasia:
- Occur in dividing cell (That is cell permit mitotic division).
- Cell involves: Labile cell and Stable cell.
- Hypertrophy:
- Occur in Both dividing and non-dividing cells.
- Cell involves: Permanent cell, Labile and stable cell also.

Comments (0)