|
Impotency It is the inability of a person to perform sexual intercourse. |
|
Sterility It is the inability of a male to beget children and in the female inability to conceive children. |
|
Frigidity It is an inability to initiate or maintain the sexual arousal pattern in females. |
| Sexual dysfunction is an impairment either in the desire for sexual gratification or in the ability to achieve it. |
|
Potency: Ability of a person to perform sexual intercourse and to achieve gratification. |
|
Vaginismus It is a psychosomatic disorder where contraction of muscles of the surrounding of the vagina, cause complete obstruction of vaginal canal occurs. |
|
Bridegroom frigidity It is the coldness of sexual instinct due to excitement, fear, or shyness on the 1st night of marriage. |
|
Quoad hoc Quoad Hoc is an individual who is impotent with one particular woman but not with others. |
3 patterns of impotency:
1. He has no urge for sexual intercourse
2. He has got urge but there is no erection of the penis
3. He has got an urge, erection of penis but premature ejaculation.
Difference between impotency and sterility:
| Traits | Impotency | Sterility |
| Affected person | Only male | Both male and female |
| Sexual intercourse | Cannot perform | Can |
Medico-legal importance of impotency and sterility:
| Civil Cases |
|
1. Nullity of marriage 2. Divorce 3. Adultery 4. Disputed paternity and legitimacy 5. Adoption 6. Claim for damage, where the loss of sexual function is claimed as the result of an assault or accident |
| Criminal Cases |
|
1. Adultery 2. Rape 3. Unnatural sexual offense 4. Blackmailing |
Causes of impotency and sterility in male:
| Causes | Description |
| Age | There is no age limit. Before puberty one may be sterile but not impotency (above 60 years 50% males become impotence) |
| Defects of development & acquired abnormality |
1. Absence and non-development of penis 2. Double penis 3. Penis adherent to the scrotum 4. Hypospadias and epispadias (abnormal position of the urethral orifice) 5. Cryptorchidism (Testes fail to descend from abdomen to scrotum) 6. Removal of testis 7. Amputation of the penis 8. Azoospermia |
| Local disease |
Large hernias, elephantiasis or large hydroceles, phimosis, and adherent prepuce may cause temporary impotence by mechanical obstruction to sexual intercourse. Diseases of the testicles, epididymis, or penis, such as cancer, sarcoma, tuberculosis, syphilis, trauma (Fracture pelvis with injury to parasympathetic, fracture spine at L-4 and 5 levels with injury to sacral segments of the spinal cord) Exposure to X-rays causes temporary azoospermia. When spermatic cords are blocked due to operation or disease, ligated or cut, sterility results. Lithotomy operation may damage ejaculatory ducts. |
| General disease |
Impotence is common during the course of any acute illness Neurogenic- hemiplegia, paraplegia, sclerosis, spina bifida, tumor/injury to cauda equina Syphilis, cancer, TB, Gonorrhea, atrophy of testis. |
| Psychological cause |
Emotion, fear, guilt, anxiety, timidity, aversion, overexcitement |
Malnutrition, vitamin C and zinc deficiency may cause erectile dysfunction.
Excessive masturbation
Alcoholism, anabolic steroids, heroin, and cannabis can cause erectile dysfunction.
Heavy smoking causes impotence due to thrombosis in the penile arteries.
|
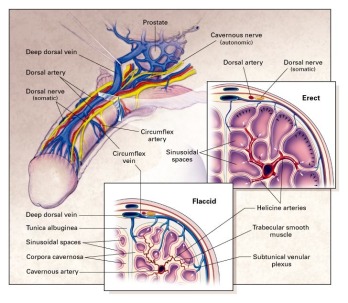
Vasculogenic impotence is one of the most frequent causes of erectile failure (about 40%). Vasculogenic impotence may be due to poor arterial inflow into the penis due to arteriosclerotic narrowing of the arteries supplying the penis. Diabetes, hypertension, pelvic and genital injuries can cause a reduction in blood flow (arteriogenic impotence), or excessive venous leakage of blood from the penis. Other causes are diabetes mellitus (20%), psychogenic (12%), neurogenic (7%), due to injuries to the spine, pelvic or perirenal injuries and pelvic surgeries causing injury to the nerves of the penis, endocrinologic, such as testosterone deficiency, luteinizing hormone and prolactin, hypothyroidism, Cushing's syndrome, trauma, etc. (20%). |
Causes of impotency & sterility in females:
| Causes | Description |
| Age | Before puberty and after menopause. In old age, they become sterile but not impotence |
| Defect of development & acquired abnormality |
Absence of vagina, adhesion of the labia, and the tough imperforate hymen, Absence of uterus, ovaries, or Fallopian tubes Acquired anomalies - Injury/operation of the vagina, hysterectomy, tubectomy & ovariectomy |
| Local Diseases: |
Gonorrhea involving the cervix, uterus, ovaries, and Fallopian tubes. Hyperesthesia of vagina, prolapse of the uterus or bladder, and vulval or Vaginal tumors, elephantiasis produce temporary impotence. Disorder of menstruation Diseases of ovaries |
| General diseases | Occupational exposure to lead or exposure to X-rays leads to sterility. Drug dependence may also lead to sterility. |
| Psychological cause |
Vaginismus is a spasmodic contraction of the vagina due to hyperesthesia. It is a classical example of a psychosomatic illness Fear of pain for sexual intercourse. |
Sterilization
It is a procedure to make male/female person sterile without interference with potency.
Types of Sterilization:
1. Compulsory:
It is done in the person
- Ordered by the state e.g., one is suffering from AIDS.
- Mental defective
- Punishment of sexual crime
2. Voluntary:
It is performed by one married person with consent from both husband and wife.
- Therapeutic:
To prevent danger to the health - Eugenic:
Sterilization to physically or mentally effective person - Contraceptive purpose
Purposes of voluntary sterilization
| Therapeutic use |
To prevent damage of the health or life of the mother. Example: 1. Repeated cesarean section 2. Repeated pregnancy 3. DM |
| Eugenic | It performs to prevent the conception of children who is likely to be physically and mentally defective. The object is to improve the race by preventing the transmission of disease and hereditable defects. |
| Contraception |
It is performed to limit the size of the family. Example: family planning |
Methods of sterilization
1. Surgical
2. Radiological
3. Chemical
4. Mechanical
Clinically sterilization is of 2 types.
A. Permanent/Surgical method
1. Vasectomy (male)
2. Tubectomy (female)
3. Exposure to deep X-rays in both sexes.
B. Temporary/voluntary method
1. Coitus interrupts
2. Loop copper – T
3. Foam tablets
4. Diaphragm
5. Oral hormonal pill
6. Spermicidal jelly
7. Condom (best)
Methods of contraception:
1. Mechanical methods: IUCD, Cu-T
2. Hormonal methods: OCP, POP
3. Post contraception method: MR, abortion
4. Sterilization: vasectomy, tubectomy
Guidelines to avoid legal complications:
1. Written consent of both husband and wife.
2. It is not unlawful in case of therapeutic and eugenic.
3. It is preferable to have a check-up after vasectomy, advised to abstain from sexual intercourse for 3 months or seminal examination show absence of spermatozoa on two successive examinations
4. The pills containing hormonal substances may be harmful so necessary precautions have to be taken.
Surrogate mother
A surrogate mother is a woman who by contact agrees to bear a child for someone else.
It is intended to help a couple, of whom the woman is infertile, but the male has no reproductive deficiency.
Artificial insemination with the semen of the barren woman's husband is carried out in a hired woman (womb leasing). After surrogate birth, the baby is returned to its biological father and his wife.
Another method is to remove a mature healthy ovum from the wife and fertilize it in 'vitro' with the husband's semen, and implant the embryo in the womb of a hired woman. In the birth registration, the hospital concerned should clearly indicate that the child has conceived through surrogate motherhood.
The legal problems of surrogate motherhood are those of Artificial Insemination Donor.
Methods of artificial fertilization:
1. Artificial insemination
2. Test tube
3. By clonic- glomadal tissue
Conception is possible without penetration of the vagina by the penis due to deposition of semen on the vulva which leads to ''fecundation ab extra", the insemination occurring due to passage of spermatozoa from the external genitalia to the uterus.
Artificial insemination
The artificial introduction of semen into the vagina, cervix, or uterus to produce pregnancy is called artificial insemination.
Types of Artificial Insemination:
1. A.I.H (Artificial Insemination Homologous/Husband) - If the semen of the woman's husband is used
2. A.I.D (Artificial Insemination Donor) - If the semen of some person other than the husband is used
3. A.I.H.D (Artificial Insemination Husband & Donor) - Pooled donor semen is composed of donor semen to which semen from the husband has been added.
Biological Aspects:
Semen is obtained by masturbation and one ml. is deposited by means of a syringe in or near the cervix.
The ovum can survive in a fertilized form only for about 24 hours, and probably only for 8 to 12 hours after it leaves the ovary.
The usual time taken by sperms to travel from the vagina to tubes is 6 to 24 hours. The power of sperms to fertilize is usually retained for about 48 hours.
The use of frozen semen for AI.D. is becoming increasingly common. This is done by the addition of glycerol, slow cooling, rapid freezing, and storage below minus 79°C.
Indication of A.I:
1. When husband is impotent and sterile.
2. When the husband is unable to deposit the semen in vagina due to hypospadiasis, epispadiasis, etc.
3. Rh incompatibility between husband and wife.
4. When Husband is suffering from hereditary disease.
Precaution of A.I:
1. Consent of husband and wife is essential.
2. Donor identity must be secreted
3. Donor should not know to whom the semen is donated and the result of insemination
4. Donors must be mentally and physically healthy and should not be suffering from any hereditary or familial disease.
5. The donor must not be a relative of either spouse, he should have had children of his own.
6. The race and characteristics of the donor should resemble those of the husband of the woman as closely as possible.
7. The donor should be of the same blood group as that of the husband.
8. There should not be any Rh incompatibility between the donor and recipient.
9. The physician should have permission to use his own best judgment in selecting the donor.
10. The couple should be psychologically fit and emotionally stable.
11. The woman to be inseminated and her husband must give consent in writing that an unknown donor should be used.
12. A witness must be present, when insemination is done.
13. It is usually wise to use "pooled" semen. When the husband's semen is mixed with that of a donor, there is the technical possibility that the husband may, in fact be the father of the child.
14. The physician who administers artificial insemination should avoid delivering the child. This will avoid the necessity of either falsifying the birth records or disclosing the true paternity in those records.
15. Usually, a single donor's semen is not used to produce more than ten children.
Complication of A.I:
The husband may feel the humiliation of his deficiency from the presence of the child of someone else and may develop psychiatric symptoms.
If the child is mentally retarded or physically deformed, the father may develop bitter feelings, for he may be held responsible for this deformity by other persons.
A neurosis may develop in the mother, based on the fact that the child belongs to her alone.
She may also develop an obsession to know the donor, and to have a second child from the same donor. The child may suffer mental trauma if he learns his past history.
TEST TUBE BABIES (in vitro fertilization; I.V.F):
The ovum is removed from the ovary through the abdominal wall and is fertilized by the sperm of her own husband in a small laboratory dish in an artificial medium. At the stage of the blastocyst, the embryo is returned to the uterus through the uterine cervix, which gets implanted in the endometrium.

Comments (0)