Small intestine
The small gut extends from the pyloric end of the stomach to the ileocaecal junction.
Total length: 6.5 meters
Parts:
1. Proximal Fixed part (Duodenum )
2. Distal Mobile part (jejunum & ileum)
Jejunum & Ileum:
The mobile part of the small intestine extends from the duodenal-jejunal flexure to the ileocaecal junction suspended from the posterior abdominal wall by mesentery.
Proximal 2/5 of the small gut forms the jejunum & distal 3/5 is known as the ileum.
Length: 6 meters or 20 feet.
Out of which jejunum is about 8 feet and ileum 12 feet.
Special features :
I. Large surface area
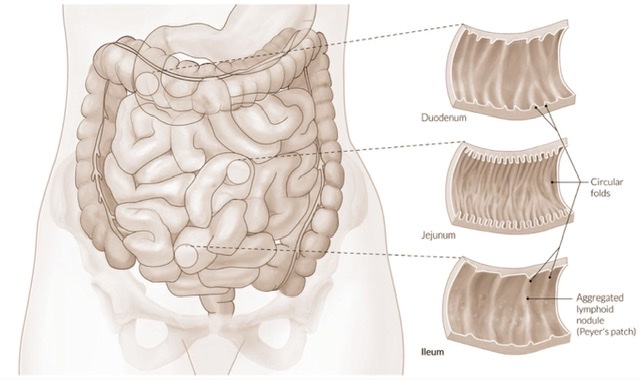
a) Circular folds/plicae circulares:
These are permanent mucous folds. They increase the surface area for absorption by about 3 folds.
Why circular folds permanent?
They are permanent because they are due to the projection of the sub-mucosa.
b) Villi:
The villi are finger-like projections of the mucous membrane, just visible to the naked eye.
Or can be said as the finger-like projection of the lamina propria covered by surface epithelium.
They increase the surface area by about 8-10 folds.
Shape of villi:
| In duodenum: Tongue like |
| In Jejunum: Leaf-like |
| In Ileum: Finger-like |
c) Microvilli:
Microvilli are the finger-like projections of the cytoplasm of surface epithelium, covered by the cell membrane, that can not be seen by the naked eye. The microvilli makeup brush borders & increase the surface area by about 20 folds.
Surface Area Increment:
| Circular Fold: by 3 folds |
| Villi: by 10 folds |
| Microvilli: by 20 folds |
| Total Increment: 3x10x20 =600 folds |
II. Intestinal glands:
1. Brunner's glands:
| They are characteristics of the duodenum & seen in the submucosa. |
| These glands produce an alkaline (pH=9) mucoid secretion rich in bicarbonate which neutralizes acid chyme from the stomach. |
| Secretes an enzyme that helps the activation of trypsinogen from pancreatic acinar cells. |
2. Crypts of Lieberkuhn:
These are straight tubular intestinal glands that open between the bases of the submucosa.
The cells at the bottom of each crypt are of two types-
a. Paneth cell &
b. Undifferentiated small columnar cell.
The paneth cells are characteristics of a small gut that secretes lysozyme. Paneth cell controls the bacterial flora of the intestine.
(Throughout the GIT tract, the submucosal gland is found only esophagus & duodenum. Rest of the viscera, there are presents mucosal gland - found in lamina propria of mucous.)
Solitary lymphatic follicles & Peyer's patches:
| Solitary follicles are the collection of localized lymphatic tissues (like lymphocytes, macrophage, plasma cells.) |
| Peyer's patches are produced by the aggregation of about 10-200 solitary follicles. They are more prominent in children & disappear in old age. Villi are absent over the patches. |
| They are situated in the antimesenteric border along the long axis of the small gut. |
| Solitary follicles are present in both the large gut & small gut. But Peyer's Patches are the characteristics feature of the ileum. |
Importance:
a) The epithelial cells covering Peyer's patches are known as M(microfold) cells. M cells endocytose the antigen and transport them to the underlying cells of lamina propria.
b) The patches may be affected in typhoid fever producing ulcers.
Difference between jejunum and ileum:
(Macroscopic)
| Jejunum | Ileum |
| Occupies upper and left parts of the intestinal area. | Occupies lower & right parts of the intestinal area. |
| Thick wall & more vascular. | Thin wall & less vascular. |
| Wider lumen | Narrow lumen |
| Mesentery: Windows present means more transparent as fat is less abundant, Arterial arcades-1 or 2, Vasa recta longer and fewer. |
Mesentery: Windows absent as Fat more abundant Arterial arcades -3 or 4, Vasa recta shorter & more numerous. |
| In the jejunum, fat is mostly confined along the root of the mesentery. Therefore, translucent windows present between the blood vessels. |
| In the ileum, fat is distributed throughout the breadth of the mesentery & windows are usually not observed. |
Microscopic differences:
| Jejunum | Ileum |
| Villi are larger, thicker, and more abundant. (Leaf-like) | Villi are shorter, thinner, and less abundant. (Finger-like) |
| Peyer’s patches are scanty | Peyer's patches are more numerous. |
| Circular folds are large, numerous & closely set. | Circular folds are smaller, few & sparsely set. |
Histological structures of the small intestine (Mobile part):
1) Serous coat:
Derived from the peritoneum and invests the entire tube except for the attachment of mesentery.
2)Muscular coat:
Consists of outer longitudinal and inner circular layers of smooth muscle separated by the myenteric plexus of nerves (Auerbach’s plexus). During peristalsis, the muscles are stimulated. The circular muscles form a zone of constriction and a zone of dilation produced by the longitudinal muscle.
3) Submucous coat:
It consists of loose areolar tissue and contains the plexus of blood vessels, lymphatics, and nerves (Meissner’s plexus).
4) Mucous membrane:
It consists from outside inwards of muscularis mucosa, lamina propria, and surface epithelium.
Artery supply of small gut:
Duodenum:
| The first part of the duodenum is supplied by a series of end arteries. |
| Above the major duodenal papilla: Supplied by the superior pancreaticoduodenal artery, a branch of the gastroduodenal artery which is a branch of the coeliac trunk. |
| Below the major duodenal papilla: Supplied by the inferior pancreaticoduodenal artery, a branch of the superior mesenteric artery. |
Jejunum & ileum:
Supplied by the Jejunal & ileal branches from the Superior mesenteric artery
Venous drainage:
Superior mesenteric vein → portal vein.
Nerve supply of small gut:
Sympathetic supply:
Preganglionic fibers come from the T6-T9 segment of the spinal cord.
Function:-
- Decreased motility
- Decreased secretions
- Motor to sphincters.
Parasympathetic supply:
Derived from both vagus nerves.The nerve cells in Auerbach’s plexus and Meissner's plexus act as postganglionic fibers.
Function:-
- Increased motility
- Increased secretions
- Inhibitions or relaxation of sphincter.
Development of small gut:
| The mucous membrane of the duodenum above and including the ampulla of Vater is developed from the endoderm of the foregut. |
| Rest of the mucous membrane below the ampulla is developed from the endoderm of the midgut. |
| The musculature and other structures are developed from the splanchnopleuric layer of the lateral plate mesoderm. |
THE Mesentery:
The mesentery is a broad fan-shaped fold of the peritoneum and suspends the jejunum & ileum from the posterior abdominal wall.
It presents two borders-
A) Vertebral border or root of the mesentery or attached border.
B) Intestinal or free border.
A. Root of the mesentery:
Length: 15cm (6 inches)
Extension: Obliquely downwards from the left side of the L2 vertebrae at the duodenojejunal flexure to the right sacroiliac joint at the ileocaecal junction.
B. Free or intestinal border:
It is about 20 feet long.
Extension: From the duodenojejunal flexure to the ileocaecal junction.
Structures crossed by the root of the mesentery:
- Third part of duodenum
- Abdominal aorta
- IVC
- Right gonadal vessels
- Right ureter & right psoas major
- Right genito-femoral nerve
- Right sacroiliac joint
Contents of the mesentery:
- Jejunum & ileum.
- Jejunal & ileal branches of superior mesenteric vessels.
- Intestinal lymphatics & mesenteric lymph nodes(100-200 in number )
- Loose areolar tissue and plexus of nerve around the blood vessels.
- Fat
| In the jejunum, fat is mostly confined along the root of the mesentery. Therefore, translucent windows present between the blood vessels. |
| In the ileum, fat is distributed throughout the breadth of the mesentery & windows are usually not observed. |
Physiological inguinal hernia:
As a result of the rapid growth of the liver, the abdominal cavity temporarily becomes too small to contain all the intestinal loops. They enter the extraembryonic cavity in the umbilical cord during the 6th week of development. This is known as physiological inguinal herniation.
Meckel’s diverticulum:
It is a blind pouch that arises from the antimesenteric border of the ileum about 2 feet proximal to the ileocaecal junction.
Length: 2 inches
Present in 2% subjects.
Formation:
The diverticulum is a remnant of the proximal part of the vitello-intestinal duct. In fetal life, it connects the midgut with the extraembryonic part of the yolk sac in the umbilical cord.
Clinical importance:
| It can become uncreated and cause intestinal perforation. |
| It may be inflamed and may spread to the peritoneal cavity. |
| It may cause intestinal obstruction. |
Also read: Anatomy Question Collection
Also read: Anatomy Questions & Answers
Also read: Anatomy notes

Comments (0)