Blood & Body Fluids Physiology (Viva)
Q.1 How much is the volume of total body water (TBW) in a normal young adult?
Males: 60 – 65% of body weight.
Females: 50 – 55%.
Normally, TBW is about 40 liters in a person weighing 70 kg.
Q.2 Name the compartments of body fluid.
- Intracellular fluid (ICF) present inside the cells forming about 55% of the TBW, i.e. 22 liters
- Extracellular fluid (ECF) present outside the cells forming about 45% of TBW, i.e. 18 liters.
Q.3 How is ECF distributed? ECF is distributed in five subunits:
- Interstitial fluid and lymph – 20%
- Plasma – 7.5%
- Fluid in bones – 7.5%
- Fluid in connective tissues – 7.5%
- Transcellular fluid – 2.5%.
Transcellular fluid includes cerebrospinal fluid, intraocular fluid, digestive juices, serous fluid (like intrapleural fluid, pericardial fluid, and peritoneal fluid), synovial fluid, and fluid in the urinary tract.
Q.4 What are the main differences between ECF and ICF?
Composition:
ECF contains more of sodium, chlorides, and bicarbonates whereas ICF contains more of potassium, magnesium, phosphates, sulfates, and proteins
Volume:
The quantity of ECF is less (18 liters) and that of ICF is more (22 liters)
pH:
The pH of ECF is 7.4 and that of ICF is 7.0.
Q.5 Name the method by which the volume of body fluids is measured.
Indicator (dye) dilution method.
Q.6 What are the qualities (characteristics) of the marker substance?
Marker substance:
- Must be nontoxic
- Must mix well with fluid compartment within a reasonable time
- Should not be excreted rapidly
- Should not change the color of body fluid
- Should not alter the volume of body fluid.
Q.7 Which type of marker substances is used to measure TBW? Give examples.
The marker substances which can move freely into all the compartments of the body fluid are used to measure TBW.
Examples: Deuterium oxide, tritium oxide, and antipyrine.
Q.8 Which type of marker substances is used to measure ECF volume? Give examples.
The substances which remain within the compartments of ECF and do not enter inside the cells are used to measure ECF volume.
Examples: Radioactive ions of sodium, chloride, bromide, sulfate and thiosulfate, and nonmetabolizable saccharides like inulin, mannitol, and sucrose.
Q.9 What are sodium space, chloride space, inulin space, and sucrose space?
Some of the marker substances like sodium, chloride, inulin, and sucrose, which are used to measure ECF volume move widely throughout all the sub-compartments of ECF. The measured volume of ECF by using these substances is called sodium space, chloride space, inulin space, or sucrose space.
Q.10 How is the ICF volume measured?
The volume of ICF cannot be measured directly because there is no substance, which can enter the cells without mixing with ECF. So, the ICF volume can be measured only by indirect method i.e., by measuring the volume of TBW and ECF. Thus, ICF volume = TBW – ECF volume.
Q.11 Which type of substance is used to measure plasma volume? Give examples.
Plasma volume can be measured by using marker substances, which bind strongly with plasma proteins and do not diffuse into interstitium.
Examples: Radioactive iodine (131I) and Evans blue (T-1824)
Q.12 How is interstitial fluid volume measured?
It cannot be measured directly. It is calculated from the values of ECF volume and plasma volume. Interstitial fluid volume = ECF volume – Plasma volume.
Q.13 What are the features of severe and very severe dehydration?
Severe dehydration: Decrease in blood volume, decrease in cardiac output, and hypovolemic shock.
Very severe dehydration: Damage of organs like brain, liver, and kidneys, mental depression, confusion, renal failure, and coma.
Q.14 What is overhydration (hyperhydration, water excess, or water intoxication)?
It is the condition in which the water content in the body increases enormously.
Q.15 List the causes of overhydration.
- Heart failure
- Renal disorders
- Hypersecretion of ADH
- Administration of large quantities of medications and fluids
- Underdeveloped kidney in the first month of infancy
- Swimming practice during infancy
- Consumption of excess water (> 8 liters/ day).
Q.16 What is the difference between plasma and serum?
Plasma is the fluid portion of the blood obtained without clotting while serum is the fluid obtained after clotting. Serum is thus plasma without fibrin.
Q.17 What is the normal concentration of plasma protein?
It is 6.4-8.3 gm/100 ml of blood.
Q.18 How hypoproteinemia produces edema?
Hypoproteinemia → decrease in capillary oncotic pressure→ decrease in filtration at the arterial end→ decrease in absorption of fluid at the venous end? abnormal collection of fluid in interstitial spaces → edema.
Q.19 What is A/G ratio?
It is the ratio of albumin to globulin.
Normally it is 1.7:1.
Q.20 What is the average daily production of plasma proteins?
It is about 15 gm/day.
Q.21 Can any of the plasma proteins pass through the capillary endothelium?
Capillary endothelium normally is impermeable to plasma proteins though in some diseases like glomerulonephritis, nephrotic syndrome, etc. albumin can pass through the capillary membranes.
Q.22 What are the features of severe conditions of overhydration?
Delirium, seizures, and coma.
Q.23 How much is the volume of the blood in a normal young healthy adult?
5 liters.
Q.24 What is the normal pH of the blood?
7.4.
Q.25 What is the normal viscosity of the blood?
Normally, the blood is five times more viscous than water.
Q.26 What is the cause for the viscosity of the blood?
Presence of red blood cells and plasma proteins.
Q.27 What is the composition of blood? Blood consists of many components these include :
55% Plasma.
45%, Blood cells of these 99% are erythrocytes (RBC), and 1% Leukocytes (WBC and platelets).
Q.28 Name the organic substances of plasma.
| Plasma proteins—albumin, globulin, and fibrinogen |
| Amino acids |
| Carbohydrates—glucose |
| Fats—triglycerides, cholesterol, and phospholipids |
| Internal secretions—hormones |
| Enzymes |
| Non-protein nitrogenous substances— ammonia, creatine, creatinine, xanthine, hypoxanthine, urea, and uric acid |
| Antibodies. |
Q.29 Name the inorganic substances and gases of plasma.
The inorganic substances are sodium, calcium, potassium, magnesium, bicarbonate, chloride, phosphate, iodide, iron, and copper. The gases present in blood are oxygen and carbon dioxide.
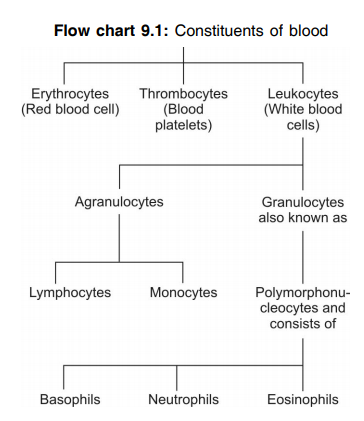
Q.30 What are the formed elements of the blood?
The formed elements of the blood are the blood cells:
- Erythrocyte or red blood cell (RBC)
- Leukocyte or white blood cell (WBC)
- Platelet (thrombocyte).
Q.31 What is hematocrit? What is the other name for it? What is its normal value?
The volume of RBCs in the blood expressed in percentage is called hematocrit. It is otherwise called packed cell volume (PCV). Normal value: 45%.
Q.32 How is hematocrit determined?
Hematocrit is determined by using Wintrobe’s tube or hematocrit tube. Blood is mixed with anticoagulant (EDTA), filled in this tube, and centrifuged for 30 minutes at a speed of 3000 revolutions per minute (RPM). Then the tube is taken out and reading is taken.
Q.33 What are the different layers noticed in the hematocrit tube after centrifuging?
- The upper clear supernatant fluid is plasma and it is normally 55%
- The lower red-colored column is packed red blood cells, which is about 45%
- In between the plasma and red blood cells, there is a thin white buffy coat, which is formed by the collection of WBCs and platelets.
Q.34 Name the plasma proteins.
Serum albumin, serum globulin, and fibrinogen.
Q.35 What is serum?
When blood is collected in a container, it clots. After 45 minutes, a straw-colored fluid oozes out of the blood clot. This fluid is called serum.
Q.36 What is the composition of serum?
It contains all the substances, which are present in the plasma except fibrinogen. The fibrinogen is converted into fibrin during the process of clotting. That is why serum is usually expressed as plasma minus fibrinogen.
Q.37 Give the normal values of plasma proteins.
Total plasma proteins: 7.3 gm%
Albumin: 4.7 gm%
Globulin: 2.3 gm%
Fibrinogen: 0.3 gm%
Q.38 Name the methods by which the plasma proteins are separated.
- Precipitation method
- Salting out method
- Electrophoretic method
- Cohn’s fractional precipitation method
- Ultracentrifugation method
- Immunoelectrophoretic method.
Q.39 What are the functions of plasma proteins?
The plasma proteins:
- Help in coagulation of blood (fibrinogen)
- Play important role in defense mechanism against invading organism (gamma globulin)
- Help in the transport of hormones (albumin and globulin)
- Maintain the osmotic pressure of the blood (albumin plays an important role)
- Regulate the acid-base balance in blood (buffering action)
- Provide viscosity to the blood
- Help in the erythrocyte sedimentation rate
- Help in maintaining the suspension stability of the red blood cells
- Along with leukocytes, the plasma proteins produce trephone bodies in tissue culture
- Act as reserve proteins during conditions like starvation.
Q.40 Name the conditions when hypoproteinemia occurs.
- Diarrhea
- Hemorrhage
- Burns
- Pregnancy
- Malnutrition
- Prolonged starvation
- Cirrhosis of liver
- Chronic infections like chronic hepatitis or chronic nephritis.
Q.41 Name the conditions when hyperproteinemia occurs.
- Dehydration
- Hemolysis
- Acute infections like acute hepatitis or acute nephritis
- Respiratory distress syndrome
- Excess of glucocorticoids
- Leukemia
- Rheumatoid arthritis
- Alcoholism.
Q.42 What is plasmapheresis?
Plasmapheresis is the experimental procedure done in animals to demonstrate the importance of plasma proteins.
Q.43 What is therapeutic plasma exchange?
Therapeutic plasma exchange is the process of plasmapheresis. It is used as a blood purification procedure for an effective temporary treatment of many autoimmune diseases like myasthenia gravis, thrombocytopenic purpura, etc
Q.44 Which is the most common site for bone marrow biopsy?
Body of sternum between 2nd and 3rd ribs.
Q.45 What is the normal average ratio of WBC to RBC in human blood?
It is 1:700 (WBC: RBC).
Q.46 Why erythrocytes are red in color?
Because of the presence of hemoglobin.
Q.47 What is normal RBC count?
Adult males: 5 million/cu mm of blood
Adult females: 4.5 million/cu mm of blood.
Q.48 What is the normal size of RBC?
Diameter: 7.2 microns (μ)
Thickness: 2.2 μ in periphery and 1 μ in the center
Surface area: 120 square μ
Volume: 90 cubic μ
Q.49 What is the normal shape of RBC?
When seen from front: Spherical
When seen from side: Biconcave or dumbbell-shaped
The reason for the dumbbell shape of RBC is the thicker periphery (2.2 μ) and thinner center (1 μ).
Q.50 What are the advantages of the biconcave shape of RBC?
- It helps in equal and rapid diffusion of oxygen and other substances into the interior of the cell
- It provides a large surface area for absorption or removal of different substances
- It offers minimal tension on the membrane when the volume of cell alters
- While passing through minute capillaries, these cells can squeeze through the capillaries very easily without being damaged.
Q.51 What is the fate of hemoglobin?
Old and inactive red cells are ingested by the RES and are broken into globin and iron. Globin and iron are reused whereas the porphyrin moiety of iron is converted into biliverdin and thence bilirubin which is excreted into bile and ultimately excreted mostly through the feces and partly through the urine.
Q.52 What is rouleaux formation?
When the blood is taken out of the blood vessel and allowed to stand without movement, the RBCs pile up one above the other like the pile of coins. This is known as rouleaux formation.
Q.53 What is polycythemia?
An increase in RBC count is called polycythemia.
Q.54 What is physiological polycythemia? Name some conditions when it occurs.
An increase in the number of RBC in physiological conditions is known as physiological polycythemia.
It occurs in:
- Age – infancy
- Sex – in males
- High altitude
- Muscular exercise
- Emotional conditions
- Increased environmental temperature
- After meals.
Q.55 Describe pathological polycythemia in brief.
The abnormal increase in RBC count is called pathological polycythemia.
It is two types:
• Primary polycythemia or polycythemia vera
– persistent increase in RBC count occurs because of malignancy of bone marrow
• Secondary polycythemia
– increase in the number of RBC because of diseases other than the bone marrow diseases, i.e. it is secondary to some pathological conditions.
Q.56 Name the diseases when secondary polycythemia occurs.
- Respiratory diseases
- Congenital heart disease
- Ayerza’s disease
- Chronic carbon monoxide poisoning
- Poisoning by chemicals like phosphorus and arsenic
- Repeated mild hemorrhages.
Q.57 What are the physiological conditions when RBC count decreases?
- After sleep
- During pregnancy
- At high barometric pressure.
Q.58 What are the possible variations in the size of RBC?
- Microcytes—decrease in the size of RBC as in the case of iron deficiency anemia
- Macrocytes—increase in the size of RBC as in the case of megaloblastic anemia
- Anisocytosis—unequal sizes of RBC as in the case of pernicious anemia.
Q.59. What are the abnormal shapes of RBC?
- Crenation—shrunken cell
- Spherocytosis—globular form
- Elliptocytosis—elliptical shape
- Sickle shape—crescent shape
- Poikilocytosis—unusual shapes.
Q.60 What is the normal life span of RBC?
120 days
Q.61 How is the life span of RBC determined?
By radioisotope method.
Q.62 What is the fate of RBC after its life span?
After the life span of 120 days, the RBC is destroyed and heme and globin are released. From heme, iron and bilirubin are released. The iron is stored as ferritin. The globin part is stored as protein. Q.63 Name the main conditions in which blood viscosity rise. It is during acidosis, hypercalcemia, and hyperglycemia.
Q.64 Name the buffer systems in the body which help to maintain the body pH.
It is bicarbonate, phosphate, protein, and hemoglobin buffer systems.
Q.65. How is the biconcavity of RBCs maintained?
It is maintained by the presence of a contractile layer of a lipoprotein molecule “spectrin” in a fibrillar manner below its cell membrane.
Q.66 What are the advantages of the biconcave shape of RBC?
These are:
- It can withstand considerable changes of osmotic pressure by altering its cell volume and thereby prevent hemolysis.
- Allows easy passage of RBC through narrow capillaries by folding itself.
- Facilitates quick and optimal exchange of gases in and out of hemoglobin.
Q.67 What are the advantages of having no nucleus, no mitochondria, and no ribosome in RBC?
It is to accommodate more amount of hemoglobin and also to decrease the use of O2 by its own structure and thereby increases the availability of O2 to the other cells.
Q.68 What are the disadvantages of nonnucleated RBC?
- It cannot multiply.
- It cannot synthesize necessary enzymes so has less lifespan.
Q.69 How does RBC survive for 120 days though it has no nucleus, mitochondria, and ribosomes?
For energy supply RBCs depend on glucose metabolism only, which comes through facilitated diffusion. These glucoses are oxidized by cytoplasmic enzymes already present inside the cells to get the energy for their activity. When these cytoplasmic enzymes are exhausted, i.e. after 120 days, it dies.
Q.70 Which is the principal cation in RBC?
It is potassium ion.
Q.71 Why RBC is stained pink by Leishman’s stain though it has no ribosomes in their cytoplasm?
It is because of the presence of hemoglobin.
Q.72 Mention the site of RBC formation.
- In the fetus—bone marrow, spleen, liver, and thymus gland.
- After birth—red bone marrow of long bones like the sternum, vertebrae, etc.
Q.73 What is the site of production of heme of Hb?
It is in mitochondria.
Q.74 Name the common methods of Hb estimation.
These are: Sahli’s hemoglobinometer method, Haldane hemoglobinometer method, Oxy-Hb colorimetric, and also Cyano methemoglobin colorimetric method.
Q.75 Why is Sahli’s method so accurate?
- In this method reduced Hb in the blood is not converted into acid hematin, thereby the value obtained is less than the total Hb content in the blood.
- This method depends on a person’s color vision. As the color vision varies from person to person results may also vary.
Q.76 In which form iron is stored in reticuloendothelial cells?
Ferritin and hemosiderin form.
Q.77 Mention the varieties of hemoglobin with special reference to the difference of each.
These are as follows:
- Adult Hb (HbA) - Contains 2 ? and 2 ? globin chain.
- Adult Hb (HbA2) - Contains 2 ? and 2 ? chain.
- Fetal Hb (HbF) - Contains 2 ? and 2 ? chain
- HbS - Contains 2 ? and 2 ? chain but in b chain glutamate of 6th position is replaced by a valine residue.
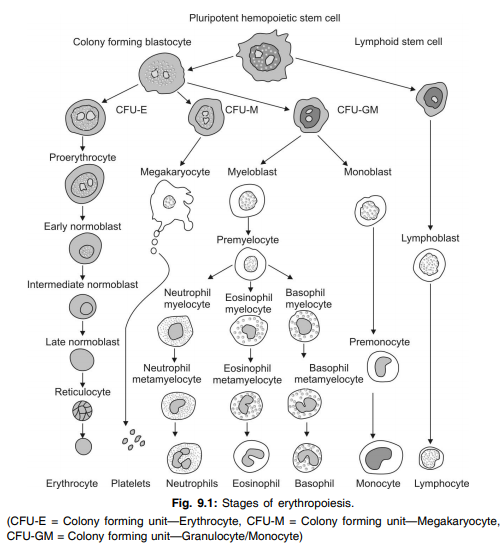
Q.78 Define erythropoiesis.
Erythropoiesis is the process that involves the origin, development, and maturation of red blood cells.
Q.79 What are the sites of erythropoiesis?
- Fetal life:
– Mesoblastic stage
– from mesenchyme of yolk sac during the first 2 months
– Hepatic stage
– from liver, spleen, and lymphoid organs from 3rd month
– Myeloid stage
– from bone marrow and liver during the last trimester
- Children:
– From the red bone marrow in all the bones.
- Adults:
– From the membranous bones and the head of long bones.
Q.80 What are the changes taking place in the cell during the process of erythropoiesis?
- Reduction in size of the cell (from the diameter of 25 ? to 7.2 ?).
- Disappearance of nucleoli and nucleus
- Appearance of hemoglobin
- Change in the staining properties of the cytoplasm.
Q.81 What are stem cells? What are the different types of stem cells?
The primitive cells in the bone marrow which give rise to blood cells are called stem cells.
The different stem cells:
Uncommitted pluripotent hemopoietic stem cells develop into committed pluripotent hemopoietic stem cells which give rise to lymphoid stem cells and colony-forming blastocysts.
Lymphoid stem cells develop into lymphocytes.
The colony-forming blastocytes are of three types:
- Colony-forming unit—Erythrocytes (GFU-E) which develop into the red blood cells
- Colony-forming unit—Granulocytes/ Monocytes (GFU–GM) from which the granulocytes and monocytes develop
- Colony-forming unit—Megakaryocytes (CFU–M), which give rise to the platelets.
Q.82 Name the stages of erythropoiesis.
- Proerythroblast
- Early normoblast
- Intermediate normoblast
- Late normoblast
- Reticulocyte
- Matured red blood cell.
Q.83 In which stage, nucleoli disappear?
Early normoblast stage.
Q.84 In which stage, hemoglobin appears?
Intermediate normoblast stage.
Q.85 In which stage, the nucleus disappears? How does the nucleus disappear?
Nucleus disappears in the late normoblast stage and it disappears by the process called pyknosis.
Q.86 What is the normal reticulocyte count?
In newborn baby: 2 to 6% of red blood cells
In adults: 1% or less than 1% of red blood cells.
Q.87 Why the reticulocyte is called the immature red blood cell?
The reticulocyte has a large quantity of hemoglobin and the nucleus is absent. It is larger than the red blood cell, round in shape with remnants of disintegrated organelles. So, it is called the immature red blood cell.
Q.88 How long does it take for the complete development of red blood cells?
It takes 7 days for the formation and maturation of red blood cells. It takes 5 days up to the stage of reticulocyte and 2 more days for the development of matured red blood cells.
Q.89 What are the factors necessary for erythropoiesis?
- General factors—erythropoietin, thyroxine, growth inducers (interleukin-3), and vitamins B, C, and D
- Maturation factors—vitamin B12, intrinsic factor of Castle, and folic acid
- Factors necessary for hemoglobin formation—proteins, iron, copper, cobalt, nickel, and vitamins.
Q.90 At what serum bilirubin level jaundice occurs in adults and infants?
- In adult: If serum bilirubin increases beyond 2 mg% it results in jaundice
- In infants: If serum bilirubin increases beyond 5 mg% it results in jaundice
Q.91 Why jaundice is first detected in the eyes?
It is because of the whiteness of sclera. Sclera has a protein known as elastin which has a high affinity to bind bilirubin. So even in low grade of jaundice bilirubin can get bind with sclera.
Q.92 Why does stool darken on standing in air?
It is due to the conversion of residual urobilinogen (colorless) to colored urobilin.
Q.93 What is prehepatic jaundice? Why it does result in unconjugated hyperbilirubinemia?
When jaundice occurs due to increased formation of bilirubin it is called as prehepatic or hemolytic jaundice. In this case, the liver is unable to conjugate the large amounts of bilirubin produced resulting in unconjugated hyperbilirubinemia.
Q.94 What is posthepatic jaundice? Why it does result in conjugated hyperbilirubinemia?
If the jaundice occurs due to biliary obstruction it is known as posthepatic jaundice. In this case, the conjugated bilirubin produced in the liver regurgitates back into blood instead of flowing out into the duodenum. This is why it results in conjugated hyperbilirubinemia.
Q.95 What is hepatic jaundice? Why it does usually result in conjugated hyperbilirubinemia?
The jaundice due to the impairment of all steps of bilirubin metabolism in the liver is known as hepatic jaundice. The commonest cause is infective hepatitis. In this case, the excretion of bilirubin is worstly affected that results in conjugated hyperbilirubinemia.
Q.96 Define hemoglobin.
Hemoglobin is the coloring matter or the chromoprotein of the red blood cells.
Q.97 What is normal hemoglobin content in the blood?
Males: 15 g% Females: 14.5 g%.
Q.98 What are the functions of hemoglobin?
- Transport of respiratory gases
- Buffer action.
Q.99 What are the components of hemoglobin?
Hemoglobin consists of a protein (globin) and iron-containing pigment (heme). The pigment part of heme is porphyrin.
Q.100 What are the types of hemoglobin?
- Adult hemoglobin (HbA) ? H2?2
- Fetal hemoglobin (HbF) ? H2?2
Q.101 What are the differences between adult hemoglobin and fetal hemoglobin?
Structural difference: Adult hemoglobin has got two alpha chains and two beta chains whereas the fetal hemoglobin has two alpha chains and two gamma chains Functional difference: Fetal hemoglobin has got more affinity for oxygen than the adult hemoglobin.
Q.102 Name the abnormal hemoglobin.
- Hemoglobinopathies – hemoglobin S, C, E, and M
- Hemoglobin in thalassemia and related disorders – hemoglobin G, H, I, Bart’s, Lepore, and constant spiring.
Q.103 Name the abnormal hemoglobin derivatives.
- Carboxyhemoglobin
- Methemoglobin or ferrihemoglobin
- Sulfhemoglobin.
Q.104 What is the quantity of iron in the body?
About 4 g
Q.105 How is iron transported in the blood?
Iron is transported in blood as transferrin (iron combines with beta globulin called apo transferrin and forms transferrin).
Q.106 How is iron stored in the body?
A large quantity of iron is stored in reticuloendothelial cells and liver hepatocytes and a small quantity is stored in other cells. In the cell cytoplasm, iron combines with a protein to form apoferritin. This is converted into ferritin and stored in the cytoplasm. A small quantity of iron is also stored in the form of hemosiderin.
Q.107 What is the morphological classification of anemia?
The classification of anemia according to the size and color (hemoglobin content) of RBC is known as morphological classification.
By this, the anemia is classified into four types:
- Normocytic normochromic anemia – the size and the hemoglobin content of the cells are normal but the number is reduced
- Macrocytic normochromic anemia – the cells are larger with normal hemoglobin content but the number is reduced
- Macrocytic hypochromic anemia – the cells are larger in size with less hemoglobin content
- Microcytic hypochromic anemia – cells are smaller with less hemoglobin content.
Q.108 What is the etiological classification of anemia?
The classification of anemia depending upon the cause is known as etiological classification.
By this, anemia is classified into five types:
- Hemorrhagic anemia – due to blood loss
- Hemolytic anemia – due to the destruction of a large number of red blood cells
- Nutrition deficiency anemia – due to lack of nutritive substances like iron, protein, and vitamins C and B12
- Aplastic anemia – due to destruction of bone marrow
- Anemia of chronic diseases – due to sustained diseases.
Q.109 What is the commonest form of anemia in the world?
It is iron deficiency anemia.
Q.110 What is the etiology of pernicious anemia?
It is due to a deficiency of the hematinic principle, i.e. lack of castle’s intrinsic factor, resulting in failure of absorption of vitamin B12 from the diet through the ileum.
Q.111 Name the physiological and pathological condition of anemia?
Physiological—Pregnancy.
Pathological—Thalassemia, spherocytosis, malaria, iron deficiency, etc.
Q.112 What will happen if folic acid is given to a pernicious anemic patients?
The administration of folic acid to pernicious anemic patient will improve the blood picture but it can not protect against neuropathy which is due to deficiency of Vit-B12.
Q.113 What is the role of iron in the body?
These are: synthesis of hemoglobin, myoglobin, and cytochromes.
Q.114 What is the blood and bone marrow picture in iron deficiency anemia?
The RBCs are microcytic, hypochromic and MCH, MCHC, and total RBC count is reduced, whereas the bone marrow shows the proliferation of the precursor cells with a larger proportion of the mature forms. Some of the precursor cells may show scanty, polychromatic cytoplasm with a pyknotic nucleus, i.e. the cytoplasmic maturity is less than nuclear maturity.
Q.115 What is the blood and bone marrow picture in megaloblastic anemia?
The blood picture is characterized by macrocytosis, anisocytosis, poikilocytosis, neutropenia with over matured neutrophils and also thrombocytopenia. Whereas in bone marrow all the RBC precursors show megaloblastic changes that includes:
- Larger cell with larger nucleus
- More reticular chromatin
- Normal hemoglobinization of cytoplasm.
Q.116 What are the effects of folate deficiency?
This results in defective erythropoiesis resulting in megaloblastic anemia
Q.117 Compare and contrast the folic acid, Vit-B12, and iron deficiency anemia.
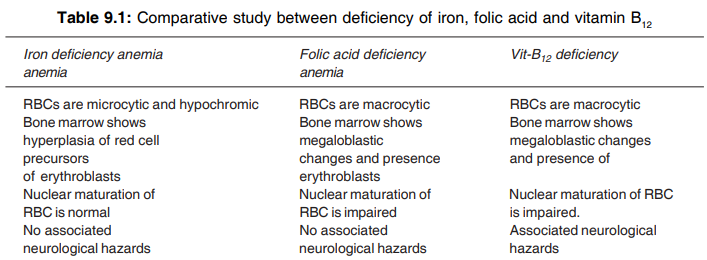
Q.118 Give characteristics features of
(i) iron-deficiency anemia
(ii) pernicious anemia.
- Characteristics feature of iron deficiency anemia is as follows:
– Microcytic hypochromic RBC
– MCV, MCH, MCHC, and CI decreases
– RBC count decreases or remains normal
– Normoblastic hyperplasia of bone marrow
– Normal WBC and platelet count
– Soft, brittle, and spoon-shaped nail
– Angry red tongue and dysphagia
– Irritability, loss of concentration, headache, impotence
– Early breathlessness, palpitation
- Characteristics feature of pernicious anemia is as follows:
– Microcytic normochromic RBC
– Marked decrease in RBC count and Hb concentration
– Lemon yellow-colored skin due to anemic paleness and mild jaundice
– MCV, MCH increases and MCHC remains normal
– Increase in reticulocyte count
– Low-grade hemolytic jaundice
– Increase in serum iron concentration
– Paresthesia, i.e. numbness, tingling, burning sensation ataxia, etc.
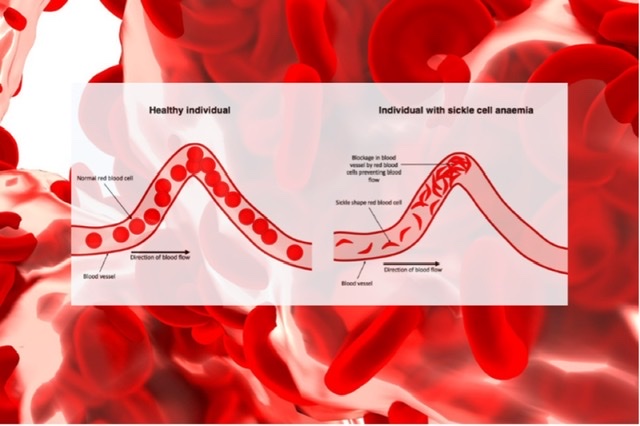
Q.119 What is sickle cell anemia?
Anemia due to the presence of sickle-shaped RBCs that contain abnormal hemoglobin (hemoglobin S) is called sickle cell anemia.
Q.120 What is thalassemia? What are its other names?
Thalassemia is the anemia due to inherited anomalies of hemoglobin. It is also called Cooley’s anemia or Mediterranean anemia.
Q.121 What is the role of the intrinsic factor of Castle?
The intrinsic factor of Castle is essential for the absorption of vitamin B12 (extrinsic factor) from the intestine. Vitamin B12 and the intrinsic factor of Castle together form the hematinic principle, which is necessary for the maturation of red blood cells.
Q.122 What is pernicious or Addison’s anemia?
Anemia due to deficiency of vitamin B12 or intrinsic factor of Castle is known as pernicious or Addison’s anemia.
Q.123 What is the morphology of RBC in pernicious anemia? Why?
In pernicious anemia, the RBCs are macrocytic and normochromic. This is because of a lack of vitamin B12 and/or intrinsic factor which are necessary for the maturation of red blood cells. So, the cells are not matured and remain larger in size.
Q.124 What is megaloblastic anemia?
Anemia due to deficiency of folic acid is known as megaloblastic anemia.
Q.125 What is the morphology of RBC in megaloblastic anemia? Why?
Megaloblastic anemia is due to the lack of folic acid, which is essential for the synthesis of DNA in red blood cells. Because of the deficiency of folic acid, DNA synthesis becomes defective. So, the cells are not matured and are macrocytic and hypochromic in nature.
Q.126 What is ESR? What is its normal value?
ESR or erythrocyte sedimentation rate is the rate at which the RBCs settle down when the blood is allowed to stand.
Normal value:
Males : 3 to 7 mm in one hour
Females: 5 to 9 mm in one hour
Infants : 0 to 2 mm in one hour.
Q.127 How is ESR determined?
By Westergren’s method or Wintrob’s method.
Q.128 What is the clinical importance of determining ESR?
Determination of ESR helps for diagnosis and prognosis. It has got more of prognostic value than the diagnostic importance.
Q.129 Name the physiological conditions when ESR increases.
ESR increases in infants, children, and females. In females, it further increases during menstruation and pregnancy.
Q.130 Name the pathological conditions when ESR increases.
Tuberculosis, some types of anemia, rheumatoid arthritis, rheumatic fever, and liver diseases.
Q.131 Name the pathological conditions when ESR decreases.
Allergic conditions, sickle cell anemia, peptone shock, and polycythemia.
Q.132 What is packed cell volume (PCV)?
Packed cell volume is the volume of RBCs packed at the bottom of a hematocrit tube when the blood is centrifuged.
The normal value is 40 to 45% in males and 38 to 42% in females.
Q.133 Name the condition when PCV increases.
Polycythemia.
Q.134Name the conditions when PCV decreases.
Anemia and pregnancy.
Q.135 What are blood indices?
Blood indices are the values, which indicate the size, volume, and the hemoglobin content of RBCs.
Q.136 Define and give the normal values of blood indices.
| Mean corpuscular volume (MCV): The average volume of a single red blood cell – 78 to 90 cu. μ |
| Mean corpuscular hemoglobin (MCH): The quantity or amount of hemoglobin present in one red blood cell – 27 to 32 pg |
| Mean corpuscular hemoglobin concentration (MCHC): The concentration of hemoglobin in one red blood cell – 30 to 38% |
| Color index (CI): The ratio between the percentage of hemoglobin and the percentage of RBCs in the blood – 0.8 to 1.2. |
Q.137 What is the advantage of blood indices?
Blood indices help to determine the type of anemia.
Q.138 What is hemolysis?
The breakdown of blood cells especially the RBCs is known as hemolysis.
Q.139 What is fragility? Which RBCs are more fragile?
The susceptibility of the RBCs to breakdown (hemolysis) is known as fragility. Older RBCs are more fragile and are easily broken down.
Q.140 Enumerate the variations of osmotic fragility of RBC.
Osmotic fragility is decreased during acholuric jaundice and some anemias. Whereas it is increased during hereditary spherocytosis, deficiency of glucose-6- phosphate dehydrogenase, cobra bite, etc.
Q.141 What happens if the RBC is kept in hypotonic and hypertonic saline?
In a hypotonic solution, water moves inside the RBC cell due to the concentration gradient → swelling up of RBC → increase of RBC volume → rupture (hemolysis) of RBC takes place.
In a hypertonic solution, water moves out of the cell → shrinkage of the cell (crenated).
Q.142 What are hemolysins? Name the hemolysins.
Hemolysins or hemolytic agents are the substances, which cause the breakdown of red blood cells.
Hemolysins are:
- Chemical substances – alcohol, benzene, chloroform, ether, acid, alkalis like ammonia, bile salts, saponin, and poisons like arsenical preparations, carbolic acid nitrobenzene, and resin
- Toxins from bacteria
- Venom of poisonous snakes like cobra
- Hemolysins from normal tissues.
Q.143 What are the differences between the RBC and WBC?
Structural differences: RBC is nonnucleated, biconcave in shape (round in front view), and red in color whereas WBC is nucleated, irregular in shape, and colorless
Functional differences: RBC transports respiratory gases and plays an important role in buffer function whereas WBC plays important role in defense of the body.
Q.144 Classify WBCs.
WBCs are classified into granulocytes and agranulocytes depending upon the presence or absence of granules in the cytoplasm.
Q.145 What are trephones?
These are the substances prepared by leukocytes from plasma proteins that help in tissue nutrition.
Q.146 What is the average period for the normal development of neutrophils?
12 days.
Q.147 Why the neutrophils are called polymorphs?
Because they have a multilobed nucleus.
Q.148 Why neutrophils are so named?
This is a misnomer because they are not stained by the neutral stain rather by the mixed (both acidic and basic) stain like Leishman stain.
Q.149 Which stain is generally used to stain the peripheral blood smear?
It is Leishman stain.
Q.150 Which is the largest cell in the peripheral blood?
It is monocyte (diameter 15-20 μm).
Q.151 What is respiratory burst?
Within seconds of stimulation neutrophils sharply increase their oxygen uptake which is known as respiratory burst.
Q.152 What is Cook-Arneth count? What is its significance?
Counting of neutrophils on the basis of the number of lobes of their nuclei is called Cook- Arneth count. Clinical significance: It represents the maturity of neutrophils. If a shift to the left occurs that indicates the hyperactive bone marrow whereas hypoactive bone marrow is indicated by a shift to the right
Q.153 How do you differentiate between neutrophils, eosinophils, and basophils?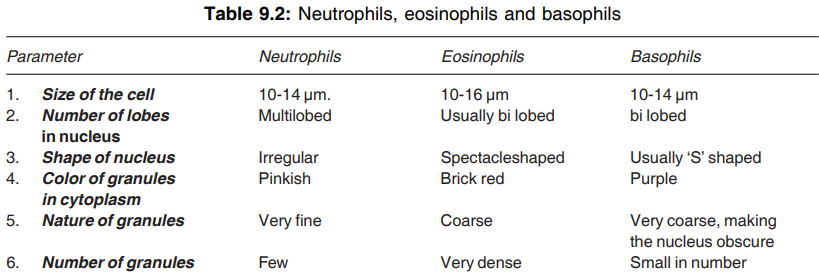
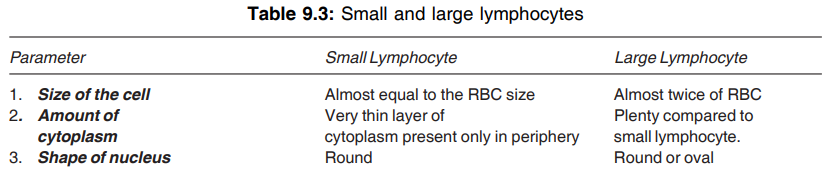
Q.154 How do you differentiate small and large lymphocyte? Which one is more mature?
Small lymphocyte is more mature.
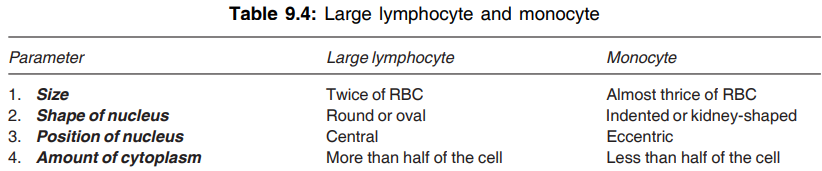
Q.155 How do you differentiate large lymphocyte with monocyte?
Q.156 What is Schilling index?
Arranging and counting of all leukocytes according to their age is known as the Schilling index.
Q.157 What are the body’s Ist line of defense and where they are located?
It is a monocyte-macrophage system or RES. They are located in almost all the tissues but in different form, e.g.
- In skin and sub- – Histocytes cutaneous tissues
- Lungs – Alveolar macrophages
- Intestine – Lymphoid tissue
- Liver and – Kupffer cells. spleen pulp
Q.158 Which lobed neutrophils are most active?
It is a three-lobed neutrophil (N3).
Q.159 What do you mean by shift to the left and what is its significance?
In Arneth count, if N1 + N2 + N3 becomes greater than 80 percent then it is known as shift to left or regenerative shift. It indicates the hyperactive bone marrow.
Q.160 What is the shift to the right? What is its significance?
In Arneth count, if N4 + N5 + N6 is greater than 20 percent it is called a shift to right or degenerative shift which indicates the hypoactive bone marrow.
Q.161 Is trilobed eosinophil possible?
Yes, 15 percent of eosinophils is trilobed.
Q.162 What are the stages of phagocytosis of WBC?
These are as follows:
Diapedesis → chemotaxis → opsonization and then phagocytosis → which causes degranulation → then inflammatory response → finally stops or limits inflammation.
Q.163 Classify the lymphocytes.
Histologically—two types:
Small and large lymphocytes.
Functionally—two types:
T-lymphocytes (responsible for cellular immunity) and
B lymphocytes (responsible for humoral immunity).
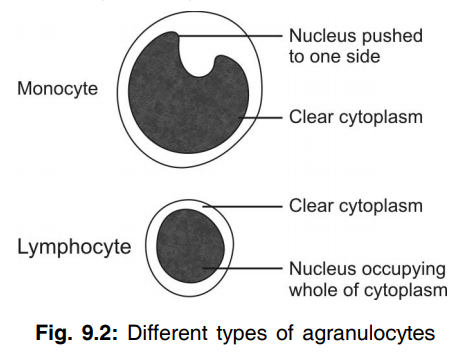
Q.164 Name the agranulocytes and describe them briefly.
The types of agranulocytes are as follows
Monocytes, which are the largest of all the WBCs with clear cytoplasm. The nucleus is kidney-shaped and it is either in the center of the cell or pushed to one side and a large amount of cytoplasm is seen
Lymphocytes, which also have clear cytoplasm. The nucleus is oval or kidney-shaped and occupies the whole of the cytoplasm. Depending upon the size, the lymphocytes are classified into small and large lymphocytes.
Q.165 Give the total count and differential count of WBCs.
Total WBC count ranges between 4,000 and 11,000/cu mm of blood.
Differential WBC count:
| Neutrophils: 50to70 % (3000 to 6000/ cu mm) |
| Eosinophils: 2 to 4% (150to 450/cu mm) |
| Basophils: 0 to 1% (0to 100/cu mm) |
| Monocytes: 2 to 6% (200to 600/cu mm) |
| Lymphocytes: 20 to 30% (1500to 2700 /cu mm) |
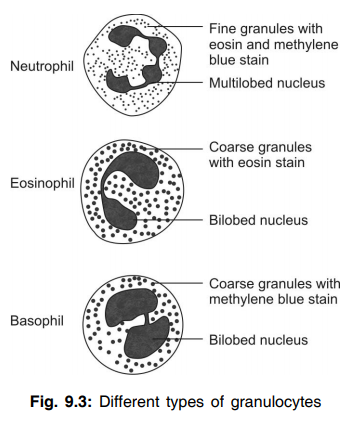
Q.166 Name the granulocytes and describe them briefly.
The types of granulocytes are as follows :
- Neutrophil with fine granules, which take both acidic and basic stain (violet).
It has a multilobed nucleus - Eosinophil with coarse granules, which stain bright red or orange with eosin.
It has a bilobed nucleus - Basophil with coarse granules, which stain purple with methylene blue.
It also has a bilobed nucleus.
Q.167 What is leukocytosis? Name some physiological conditions when leukocytosis occurs.
An increase in WBC count is known as leukocytosis. Physiologically, it is found in infants, children, and males. It also occurs in high altitudes, during muscular exercise, during emotional conditions, and in pregnancy.
Q.168 Name some pathological conditions when leukocytosis occurs.
- Infections
- Allergic conditions
- Common cold
- Tuberculosis
- Glandular fever.
Q.169 What is leukopenia? Name some pathological conditions when leukopenia occurs.
A decrease in WBC count is called leukopenia.
It occurs in:
- Anaphylactic shock
- Cirrhosis of liver
- Disorders of spleen
- Pernicious anemia
- Typhoid and paratyphoid
- Viral infections.
Q.170 What is neutrophilia? Name some pathological conditions when it occurs.
An increase in neutrophil count is called neutrophilia or neutrophilic leukocytosis.
It occurs in:
- Acute infections
- Metabolic disorders
- Injections of foreign proteins
- Injections of vaccines
- Poisoning by chemicals and drugs like lead, mercury, camphor, benzene derivatives, etc.
- Poisoning by insect venom
- After acute hemorrhage.
Q.171 Define neutropenia and mention its causes.
Neutropenia can be defined as a clinical condition characterized by the reduction of both differential and absolute neutrophil count.
Causes
Viral infections like typhoid.
Paratyphoid, AIDS, kala-azar, bone marrow depression, etc.
Q.172 What is eosinophilia? Name some pathological conditions when it occurs.
An increase in eosinophil count is called eosinophilia.
It occurs in:
• Allergic conditions
• Asthma
• Blood parasitism
• Intestinal parasitism
• Scarlet fever.
Q.173 What is eosinopenia and when does it occur?
Eosinopenia can be defined as the reduction in absolute eosinophil count below 50/ cu.mm of blood.
It can be caused by ACTH or glucocorticoid therapy, acute stressful illness, and acute pyogenic infection.
Q.174 What is basophilia? Name some pathological conditions when it occurs.
An increase in basophil count is called basophilia.
It occurs in:
• Smallpox
• Chickenpox
• Polycythemia vera.
Q.175 What is monocytosis? Name some pathological conditions when it occurs.
An increase in monocyte count is called monocytosis.
It occurs in:
- Tuberculosis
- Syphilis
- Malaria
- Kala-azar
- Glandular fever.
Q.176 Mention the causes of monocytopenia
Bone marrow depression is the major cause of monocytopenia
Q.177 Name some pathological condition in which lymphocytopenia occurs.
Low blood lymphocyte count, also known as lymphocytopenia usually occurs in patients with steroid therapy.
Q.178 What is lymphocytosis? Name some pathological conditions when it occurs.
An increase in lymphocyte count is called lymphocytosis.
It occurs in:
- Diphtheria
- Infections
- Hepatitis
- Mumps
- Rickets
- Syphilis
- Thyrotoxicosis
- Tuberculosis.
Q.179 What is leukemia?
Leukemia is the condition in which there is an uncontrolled increase in WBC count due to malignancy of bone marrow. In this, the total WBC count increases up to 1,000,000 per cu. mm of blood.
Q.180 What are the properties of WBC?
- Diapedesis—process of squeezing through the narrow blood vessels
- Amoeboid movement – movement by protruding the cytoplasm
- Chemotaxis – movement due to the attraction by chemical substances called chemoattractants released from the affected tissues
- Phagocytosis – process by which the foreign bodies are engulfed
Q.181 What are the functions of neutrophils?
Neutrophils provide first-line defense along with monocytes. The neutrophils move to the site of infection by diapedesis and engulf the foreign bodies by phagocytosis.
The enzymes like proteases, myeloperoxidases, elastase, and metalloproteinases present in the neutrophils destroy the foreign invaders. Neutrophils secrete platelet-activating factor.
Q.182 What are the chemical substances present in the granules and cell membrane of neutrophils?
Granules:
Enzymes like proteases, myeloper-oxidases, elastases and metalloproteinases and the antibody-like substances called defensins.
Cell membrane:
Dihydronicotinamide adenine dinucleotide phosphate oxidase (NADPH oxidase). All these substances help the neutrophils to destroy the foreign bodies.
Q.183 What are the functions of eosinophils?
The eosinophils play an important role in defense mechanisms by detoxification, disintegration, and removal of foreign proteins. Eosinophils also act against the parasites.
Q.184 Name the chemical substances present in the granules of eosinophils.
Eosinophil peroxidase, major basic protein, eosinophil cationic protein, eosinophil-derived neurotoxin, and cytokines.
Q.185 What are the functions of basophils?
Basophils prevent intravascular clotting by secreting heparin and play an important role in healing processes after inflammation and allergy.
Q.186 Name the chemical substances present in the granules of basophils.
Histamine, heparin, hyaluronic acid, proteases, myeloperoxidase, and cytokine.
Q.187 What are mast cells? What is their function?
Mast cells are large tissue cells resembling the basophils. These cells are present in the bone marrow and around the cutaneous blood vessels but do not enter the circulation. Mast cells play an important role during allergy and anaphylaxis by secreting substances like heparin, histamine, serotonin, and hydrolytic enzymes.
Q.188 What are the functions of monocytes?
Monocytes provide first-line defense along with neutrophils. These cells wander freely through all the tissues. The matured monocytes move into the tissues and become tissue macrophages. The macrophages engulf the foreign particles by phagocytosis and destroy them.
Q.189 What are the functions of lymphocytes?
Lymphocytes protect the body by providing immunity.
Q.190 What is pus? What are the pus cells?
Many WBCs are destroyed while attacking the invading organisms. These dead WBCs along with plasma, liquefied tissue cells, and RBCs combine to form a liquid product called pus. The dead WBCs are called the pus cells.
Q.191 What is leukopoiesis?
Leukopoiesis is the origin, development, and maturation of WBCs.
Q.192 What is a leukemoid reaction?
An extreme increase of TLC (>50,000/cumm of blood) characterized by elevated levels of leukocyte alkaline phosphatase due to severe infection is known as leukemoid reaction. Its difference with leukemia is that in the case of leukemia alkaline phosphatase level is reduced whereas here it is increased significantly.
Q.193 What is leukemia? What is its difference with leukocytosis?
Leukemia is a group of malignant neoplasms resulting from the uncontrolled proliferation of hemopoietic leukocytic stem cells of bone marrow and lymphoid tissue. In this case, TLC becomes much higher than leukocytosis, i.e. 1-3 lac/cu.mm, and the number of immature cells are dominant.
Q.194 What are the types of immunity?
Innate immunity or inborn immunity – present from the birth itself like the resistance given by the stomach against the pathogens entering through the food.
Acquired immunity – developed in the body when exposed to a new invading organism.
Q.195 What are the types of acquired immunity?
Cellular immunity and humoral immunity.
Q.196 Which are the cells responsible for acquired immunity?
Lymphocytes are responsible for acquired immunity. T lymphocytes provide cellular immunity and B lymphocytes provide humoral immunity.
Q.197 What are T lymphocytes?
Lymphocytes that are processed in the thymus and taking part in cellular immunity are called T lymphocytes.
Q.198 What are B lymphocytes? Why these cells are called so?
Lymphocytes that are processed in bone marrow and liver and taking part in humoral immunity are called B lymphocytes. These cells were first discovered in the Bursa of Fabricius in birds and hence the name B lymphocytes.
Q.199 Where are the T cells and B cells stored?
After being processed, the T cells and B cells migrate and get stored in the lymphoid tissues present in the lymph nodes, spleen, bone marrow, and gastrointestinal tract.
Q.200 What are the different types of T cells?
- Helper T cells
- Cytotoxic or killer T cells
- Suppressor T cells
- Memory T cells.
Q.201 What are the different types of B cells?
Plasma cells and memory B cells.
Q.202 What are antigens? What are the types of antigens?
The antigens are the protein substances, which induce specific immune reactions in the body.
Types of antigens:
- Self antigens or autoantigens
- Nonself antigens.
Q.203 What are the self antigens?
The antigens present in cells of our own body are known as self-antigens.
Q.204 What are the nonself antigens?
Nonself antigens are the antigens, which enter the body from outside through some bacteria, viruses, fungus, transplanted organs transfused incompatible blood cells, allergens, etc.
Q.205 What are the antigen-presenting cells?
The cells, which expose or present the antigen of invading organisms to the lymphocytes are called antigen-presenting cells. The macrophages and dendritic cells are the antigen-presenting cells.
Q.206 Name the two types of helper T cells. Mention their functions.
Helper–1 cells are concerned with cellular immunity and secrete
- Interleukin – 2 which activates other T cells
- Gamma interferon that stimulates the cytotoxic cells, macrophages, and natural killer cells.
Helper–2 cells are concerned with humoral immunity and secrete interleukins 4 and 5 which are concerned with
- Activation of B cells
- Proliferation of plasma cells
- Antibody production by plasma cells.
Q.207 What are the functions of cytotoxic T cells?
The cytotoxic T cells:
- Attack the invading organisms and destroy them by releasing cytotoxic substances like lysosomal enzymes
- Destroy cancer cells, transplanted cells, and other foreign bodies
- Destroy even the body’s own tissues which are affected by foreign bodies.
Q.208 What are the disadvantages of the actions of cytotoxic T cells?
The cytotoxic T cells are otherwise called killer T cells because these cells destroy the invading organisms. But, at the same time, the cytotoxic T cells may attack the cells in transplanted heart or kidney leading to rejection of the transplanted tissues. These cells may destroy even the tissues affected by the invading organisms.
Q.209 What is the role of suppressor T cells?
Suppressor T cells or regulatory cells suppress the action of killer cells so that, the destruction of the body’s own tissues is prevented. The suppressor T cells also suppress the activities of helper T cells.
Q.210 What is the importance of memory T cells?
Some of the T cells activated by the antigens of invading organisms move to the lymphoid tissues and remain there. These cells are called memory T cells. When the body is attacked by the same organism for the second time, these memory cells recognize the organism and immediately activate the other T cells so that, the invading organism is destroyed quickly and effectively.
Q.211 What is humoral immunity? Which are the cells responsible for it?
The immunity provided by the antibodies is known as humoral immunity. B lymphocytes are responsible for it.
Q.212 What is the role of plasma cells in humoral immunity?
Plasma cells produce antibodies against the antigens of invading organisms. The antibodies which are also called immunoglobulins destroy the invading organisms.
Q.213 Name the immunoglobulins secreted by the plasma cells.
Immunoglobulins secreted by the plasma cells are IgA, IgD, IgE, IgG, and IgM.
Q.214 What are the mechanisms of action of immunoglobulins?
Immunoglobulins destroy the invading organisms by two mechanisms:
- Direct action
- Through the complement system.
Q.215 What are the direct actions of immunoglobulins?
The direct actions by which the immunoglobulins destroy the foreign bodies are agglutination, precipitation, neutralization, and lysis.
Q.216 What is the complement system?
The system of enzymes that enhances or accelerates various activities during the fight against the invading organisms is called the complement system. Apart from the direct actions, the immunoglobulins can destroy the invading organism through this system also.
Q.217 What is a natural killer cell (NK cell)? What are its functions?
NK cell is a large granular cell with a nucleus. It is considered as the third type of lymphocyte.
NK cell:
- Destroys virus
- Destroys viral infected or damaged cells, which might form tumors
- Destroy the malignant cells
- Secretes cytokines – interleukin-2, interferons, colony-stimulating factor, and tumor necrosis factor-α
Q.218 What is autoimmune disease? Name some autoimmune diseases.
When the immune system fails in the body, antibodies are produced against the body’s own tissues and destroy them. This is known as an autoimmune disease. Some of the autoimmune diseases are insulin-dependent diabetes mellitus (IDDM), myasthenia gravis, Hashimoto’s thyroiditis, Graves’ disease, and rheumatoid arthritis.
Q.219 Define and classify immunization.
Immunization is the method of preparing the body to fight against a specific disease.
It is of two types:
- Passive immunization—produced by administration of serum or gamma globulins from a person who is already immunized to a non-immune person
- Active immunization—acquired by activating the immune system of the body.
Q.220 Define and classify cytokines.
Cytokines are the hormone-like small proteins acting as intercellular messengers by binding to specific receptors of target cells.
Cytokines are of six types:
- Interleukins
- Interferons
- Tumor necrosis factors
- Chemokines
- Defensins
- Cathelicidins.
Q.221 What are platelets? What is the normal platelet count?
Platelets or thrombocytes are small, colorless, and nonnucleated formed elements of the blood. The normal platelet count is 2.5 lakhs (250,000)/cu mm of blood.
Q.222 Name the organic substances present in the platelets.
- Contractile proteins—actin, myosin, thrombosthenin.
- von Willebrand factor
- Fibrin stabilizing factor
- Platelet-derived growth factor
- Platelet-activating factor
- Vitronectin
- Thrombospondin.
Q.223 What are the events involved in hemostasis?
These are:
- Vasoconstriction
- Formation of a temporary hemostatic plug.
- Conversion of temporary hemostatic plug into secondary or definitive hemostatic plug by fibrin.
Q.224 How the primary hemostatic plug is formed?
It is represented by the following sequences:
Platelet adhesion → platelets activation → platelets aggregation → activation of phospholipase A2 → release of arachidonic acid from membrane phospholipids → release of thromboxane A2 and prostacyclin → this ultimately causes adhesion of more and more platelets and then platelets are aggregated with each other to seal the rupture of blood vessels temporarily.
Q.225 What are the principal causes of hemorrhagic state in the body?
These are:
- Defect in the blood vessels due to infection, allergy, etc.
- Defect in platelets (purpura)
- Defect in clotting mechanism.
Q.226 What is thrombocytosis? Name some conditions when thrombocytosis occurs.
Increase in platelet count is known as thrombocytosis.
It occurs in:
- Allergic conditions
- Asphyxia
- Hemorrhage
- Bone fractures
- Surgical operations
- Splenectomy
- Rheumatic fever
- Trauma.
Q.227 What is thrombocytopenia? Name some conditions when thrombocytopenia occurs.
Decrease in platelet count is known as thrombocytopenia.
It occurs in:
- Acute infections
- Acute leukemia
- Aplastic anemia and pernicious anemia
- Chickenpox
- Smallpox
- Splenomegaly
- Scarlet fever
- Typhoid
- Tuberculosis.
Q.228 What is thrombocythemia? Name some conditions when thrombocythemia occurs.
The condition with persistent and abnormal increase in platelet count is called thrombocythemia.
It occurs in:
- Carcinoma
- Chronic leukemia
- Hodgkin’s disease.
Q.229 Name the properties of platelets.
Adhesiveness, aggregation and agglutination.
Q.230 What are the functions of platelets?
Platelets:
- Are responsible for blood clotting
- Are responsible for clot retraction
- Prevent blood loss during hemorrhage, by causing vasoconstriction and sealing the wound by plug formation
- Help in the repair of the endothelium of damaged blood vessels
- Play a role in defense mechanism by agglutination and phagocytosis.
Q.231 What is hemostasis?
The arrest of bleeding is called hemostasis.
Q.232 Name the stages of hemostasis.
Stage i: Vasoconstriction caused by serotonin secreted by platelets.
Stage ii: Formation of platelet plug caused by ADP and thromboxane A2 secreted from platelets.
Stage iii: Coagulation of blood.
Q.233 Define coagulation of blood.
When blood is shed out or collected in a container, it loses its fluidity and becomes a jelly-like mass after few minutes. This is known as coagulation or clotting of blood.
Q.234 Name the clotting factors.
- Fibrinogen
- Prothrombin
- Thromboplastin
- Calcium
- Labile factor (proaccelerin or accelerator globulin)
- Presence has not been proved
- Stable factor
- Antihemophilic factor (antihemophilic globulin)
- Christmas factor
- Stuart-Prower factor
- Plasma thromboplastin antecedent
- Hegman factor (contact factor)
- Fibrin stabilizing factor (fibrinase).
Q.235 Which is the inorganic ion necessary for blood clotting?
Calcium ion (factor IV). Q.236 Mention the role of Ca++ in the clotting mechanism. Except for the first 2 steps in the intrinsic pathway, calcium ions are required for the promotion of all reactions involved in both intrinsic and extrinsic pathways.
Q.237 Why Christmas factor is called so?
Christmas factor was named after the patient in whom it was discovered.
Q.238 Why blood does not clot during circulation?
Blood does not clot during circulation because:
- Clotting factors are in inactive form
- Smooth endothelial lining of the blood vessels does not allow the blood clotting
- Continuous flow does not allow the blood clotting
- The natural anticoagulant called heparin in the blood prevents clotting during circulation.
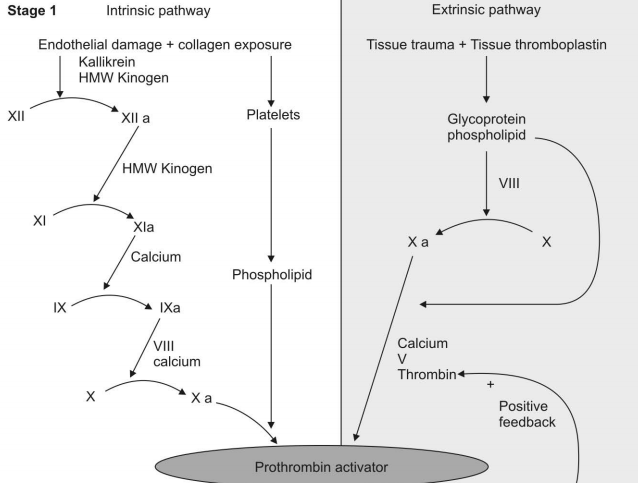
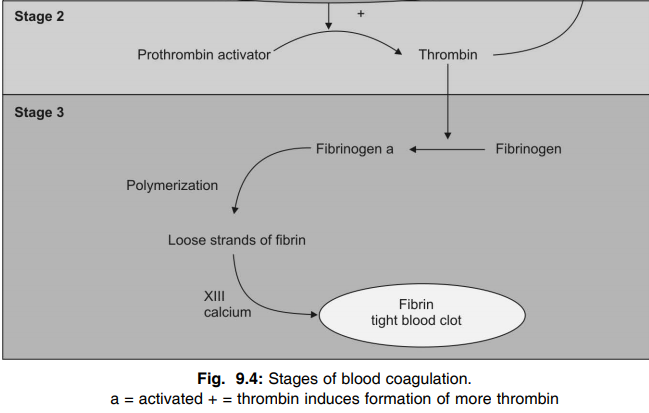
Q.239 What are the three stages of blood clotting?
Stage i: Formation of prothrombin activator
Stage ii: Conversion of prothrombin into thrombin
Stage iii: Conversion of fibrinogen into fibrin.
Q.240 What are the components of blood clot?
The blood clot consists of the RBCs, WBCs, and the platelets entrapped in the fibrin meshwork.
Q.241 What is clot retraction?
30 to 45 minutes after formation, the blood clot contracts and a straw-colored fluid called serum oozes out of it. This process is called clot retraction.
Q.242 What are the substances necessary for clot retraction?
The contractile proteins actin, myosin, and thrombosthenin present in the cytoplasm of platelets are necessary for clot retraction.
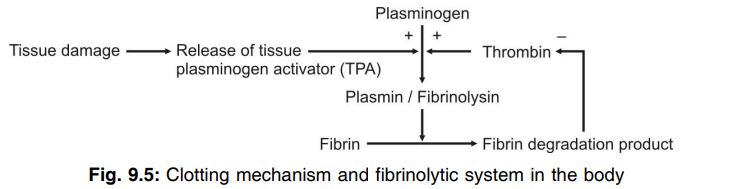
Q.243 What is lysis of clot? How is it brought?
The destruction or dissolution of a blood clot is known as lysis of clot. It is brought out by a substance called plasmin.
Q.244 What is anticoagulant?
A substance that prevents or prolongs blood clotting is called anticoagulant.
Q.245 Name some anticoagulants, which can be used in vivo (inside the body).
Heparin, dicoumarol, warfarin, and EDTA.
Q.246 What is the mechanism of action of heparin?
Heparin prevents blood clotting by:
- Suppressing activity of thrombin (antithrombin activity)
- Activating antihrombin
- Removing thrombin from circulation
- Inactivating other clotting factors.
Q.247 Name the anticoagulants, which are used in vitro.
Heparin, EDTA, oxalates, and citrates.
Q.248 Define bleeding time.
The time interval from oozing of blood after injury till the arrest of bleeding is called bleeding time.
Q.249 What is the normal bleeding time? In which disease it is prolonged?
The normal bleeding time is 1 to 3 minutes. It is prolonged in purpura.
Q.250 Define clotting time.
The time interval between oozing out of blood after injury and clot formation is called clotting time.
Q.251 What is the normal clotting time? In which disease it is prolonged?
The normal clotting time is 3 to 8 minutes. It is prolonged in hemophilia.
Q.252 What are indications of BT and CT?
These are:
- Frequent and persistent bleeding from minor injuries.
- Before the minor/ major surgeries.
- In case of a family history of bleeding.
Q.253 Which aspects of hemostasis are tested by BT and CT?
BT is to test for platelet function whereas CT is to test the abnormalities (if any) in clot formation. That is why in hemophilia BT is normal but CT is prolonged as in hemophilia, the temporary hemostatic plug is formed because of the normal functioning of platelets but they are washed off by the flowing blood as the definitive hemostatic plug, i.e. clot is not formed.
Q.254 Mention the conditions when BT and CT are prolonged.
BT is increased during thrombocytopenic purpura, allergic and also senile purpura, infection like typhus, bacterial endocarditis, deficiency of vitamin C, etc. CT is prolonged in hemophilia, afibrinogenemia, vitamin-K deficiency, liver disease, etc.
Q.255 What are the physiological and pathological variations of platelet count?
Physiological
Increase of count—in severe exercise and high altitude
Decrease of count—in newborn babies and after menstruation
Pathological
Increase of count—Severe hemorrhage and removal of spleen.
Decrease of count—Bone marrow depression, acute septic fever, aplastic anemia, toxemia, autoimmune-destruction of platelets, AIDS, etc.
Q.256 What is the basic difference between intrinsic and extrinsic system of blood clotting?
In the intrinsic system, injury to blood cells like platelets, releases phospholipid that activate different clotting factors to induce clotting. Whereas in the extrinsic system injury to blood vessels or nearby tissues releases tissue thromboplastin which induces clotting mechanism by activating different clotting factors by cascade mechanism.
Q.257 What is prothrombin time? What is its significance?
Prothrombin time is the test for prothrombin activity and thereby it is a test for testing the extrinsic system of blood coagulation.
The normal value of prothrombin time is 11-16 sec and it is increased in liver failure and deficiency of vitamin-K. It is generally used to monitor patients with anticoagulant therapy to adjust their dose.
Q.258 Name the bleeding disorders.
Hemophilia, purpura, and von Willebrand disease.
Q.259 What is hemophilia?
Hemophilia is a sex-linked inherited bleeding disorder with prolonged clotting time and normal bleeding time.
Q.260 What are the types of hemophilia? And what is the cause for each?
Hemophilia is of two types:
- Hemophilia A or classical hemophilia. It is due to the deficiency of clotting factor VIII (antihemophilic factor).
- Hemophilia B or Christmas disease. It is due to the deficiency of clotting factor IX (Christmas factor).
Q.261 How a balance is maintained between the clotting mechanism and fibrinolytic system in the body?
Factors that initiate the clotting mechanism also stimulate the dissolution of clot (fibrinolysis) by the following mechanism.
Q.262 What is purpura? What are its causes?
The purpura is a purple-colored petechial hemorrhagic condition with bruises in the skin due to the degradation of Hb over a period of time. The causes are thrombocytopenia, allergy, old age, functional platelet defects, etc.
Q.263 What is the difference between thrombocytopenia and thrombasthenia?
Reduction of platelet count below 1.5 lakh/ cu.mm of blood is known as thrombocytopenia whereas impairment of platelet functions due to the presence of abnormal platelets are known as thromboasthenia.
Q.264 Name two well known vascular causes of bleeding?
Scurvy and Cushing syndrome.
Q.265 Why does Vit-K deficiency cause bleeding tendency?
This is due to the fact that Vitamin K deficiency results in low plasma levels of both procoagulants as well as some anticoagulants. These proteins are called vitamin K dependent proteins.
Q.266 Why does blood become incoagulable following violent death?
In the case of violent death, the blood remains in fluidic and incoagulable in nature due to fibrinolysis resulted due to adrenaline-induced rapid release of plasminogen activators from endothelial cells.
Q.267 What is the difference between rouleaux formation and agglutination?
Rouleaux formation is simply stacking of RBCs without any hemolysis whereas in agglutination there is an antigen-antibody reaction on the red cells resulting in hemolysis of RBC.
Q.268 Name the cold antibodies present in our body.
ABO antibodies are the cold antibodies because they act best at low temperatures, i.e. between 5°C-20oC.
Q.269 Name the warm antibodies present in our body?
Rh-antibody is the warm antibody because they act best at normal body temperature, i.e. 37°C.
Q.270 How is hemophilia differentiated from purpura by simple laboratory test?
In hemophilia, the clotting time is prolonged whereas in purpura the bleeding time is prolonged.
Q.271 What is von Willebrand disease? What is its cause?
von Willebrand disease is the condition associated with excessive bleeding even with a mild injury. It is due to the deficiency of the von Willebrand factor. This factor is a protein necessary for the adherence of platelets to the endothelium of blood vessels during hemostasis. If there is a deficiency of this factor, the platelets do not adhere and this leads to excessive bleeding even with mild injury.
Q.272 What is thrombosis?
Intravascular clotting is known as thrombosis.
Q.273 What is thrombus?
The solid mass of intravascular clot is called a thrombus.
Q.274 What is embolism?
Embolism is the process in which the thrombus or a part of it gets detached, travels in the bloodstream, and obstructs the blood flow to any part of the body.
Q.275 Name the causes for thrombosis.
- Injury to blood vessel
- Rough endothelial lining
- Sluggish flow of blood
- Agglutination of red blood cells
- Presence of toxic substances like mercury and snake venom
- Congenital absence of protein C.
Q.276 What is Landsteiner’s law?
Landsteiner’s law states that “if an agglutinogen is present in red blood cell of a person, the corresponding agglutinin must be absent in the plasma” and “if an agglutinogen is absent in the red blood cell, the corresponding agglutinin will be present in the plasma”. According to Landsteiner’s law, blood group is classified as ‘A’, ‘B’, ‘AB’ and ‘O’ depending upon the presence or absence of agglutinogen (antigen) in the red blood cell. This grouping is also known as ABO system.
Q.277 Name the agglutinogen (antigen) and agglutinin (antibody) present in ABO system.
The agglutinogen and agglutinin present in ABO system are as follows:
In ‘A’ group: Agglutinogen is ‘A’ and agglutinin is beta (anti ‘B’)
In ‘B’ group: Agglutinogen is ‘B’ and agglutinin is alpha (anti ‘A’)
In ‘AB’ group: Both ‘A’ and ‘B’ agglutinogens are present but no agglutinin
In ‘O’ group: No agglutinogen is present but both alpha and beta agglutinins are present.
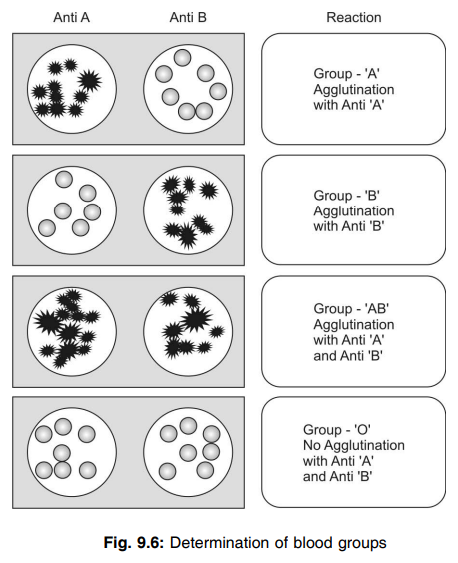
Q.278 Who is a universal donor? Why?
A person with ‘O’ group blood is called a universal donor because his blood does not contain any agglutinogens in his blood. Usually, during transfusion of blood, the RBCs of the donor (which contains agglutinogen) agglutinate with the agglutinin present in the recipient’s plasma. Since ‘O’ group blood does not contain any agglutinogen it can be given to any blood group person without the risk of agglutination. So he is known as a universal donor.
Q.279 Who is a universal recipient? Why?
A person with ‘AB’ blood group is called a universal recipient, because, his blood does not contain any agglutinin in his plasma. Usually, during blood transfusion, the donor’s agglutinogen will agglutinate with the recipient’s agglutinin. But, ‘AB’ group blood does not contain any agglutinin in plasma and, so the person with the ‘AB’ group can receive blood from persons with any other blood group. So, this person is called a universal recipient.
Q.280 What is cross-matching? What is its importance?
Matching (or blood typing or determination of blood group) is done by mixing the recipient’s RBCs with test sera. In cross-matching, the serum of the recipient and the RBCs of the donor are mixed. Cross-matching is always done before blood transfusion. If agglutination of the RBCs from a donor occurs during cross-matching, the blood from that person is not used for transfusion.
Q.281 What is the Rh factor? Why is it called so?
Rh factor is an antigen present in the red blood cell. It was first found in rhesus monkey and hence it is called Rh factor.
Q.282 How is Rh blood type classified?
Rh blood type is classified depending upon the presence or absence of Rh factor (antigen) in the RBCs. If the Rh factor is present, the person is called Rh-positive and if the Rh factor is absent, the person is called Rh-negative.
Q.283 In what way Rh type is different from ABO system?
In ABO system of blood grouping, there is a natural corresponding antibody (agglutinin) whereas, in Rh typing, there is no natural corresponding antibody.
Q.284 What are the complications (transfusion reactions) of mismatched blood transfusion?
- Agglutination
- Hemolysis
- Jaundice
- Cardiac shock
- Renal shut down.
Q.285 Why the transfusion reactions do not occur when an Rh-negative person is given Rh+positive blood for the first time? And what happens if the same person is given Rh-positive blood for the second time?
There is no antigen in Rh-negative blood and there is no antibody in the Rh-positive person. So, when Rh-positive blood is given to Rh-negative person for the first time, there is no reaction. But, the Rh antibody develops and remains in his blood. So, when the same person receives Rh-positive blood for the second time, the transfusion reactions occur
Q.286 Name the hemolytic diseases of the newborn.
- Erythroblastosis fetalis
- Hydrops fetalis
- Kernicterus.
Q.287 Explain erythroblastosis fetalis briefly.
It is the complication developed in the fetus of Rh-negative mother. When the mother is Rh-negative and the father is Rh-positive, the fetus may be Rh-positive. The placental barrier does not allow Rh antigen (D antigen) to move from fetal blood into the mother’s blood. So, there is no complication and the child escapes. But, during the delivery of the child, due to the severance of the umbilical cord, the Rh antigen from the fetal blood enters the mother’s blood. This causes the development of antibodies in the mother’s blood. During the second pregnancy, the Rh antibody from the mother’s blood enters the fetus since the placental barrier permits the Rh antibody. If this fetus also is Rh-positive, agglutination occurs in fetal blood leading to complications like severe hemolysis, jaundice, and anemia. This condition is called erythroblastosis fetalis.
Q.288 What are the complications of hemolysis in Rh-positive fetus apart from the presence of erythroblastic cells?
The other complications are hydrops fetalis and kernicterus.
Q.289 Name the blood groups other than ABO group.
Lewis blood group, MNS blood group, Auberger group, Diego group, Bombay group, Duffy group, Lutheran group, P group, Kell group, I group, Kidd group, and Sulter Xg group.
Q.290 What is the importance of determining blood groups?
Determination of blood groups helps in
- Safe blood transfusion
- Medicolegal cases
- Paternity test
- Prevention of complications like erythroblastosis fetalis.
Q.291 Name the conditions when blood transfusion is essential.
Hemorrhage, trauma, burns, and anemia.
Q.292 Why the stored blood is not suitable for transfusing WBCs and platelets to a recipient?
It is because the blood stored for more than 24 hours does not contain active WBCs and platelets.
Q.293 The term universal donor and universal recipient are no longer valid. Justify
In both the cases, complications can also be produced due to mismatching of Rh factors and other blood groups.
Q.294 What changes RBCs undergo during cold storage?
Cold storage results following changes:
- Appearance of spherocytic RBC due to a net increase in the volume of the cell.
- Increase in tendency of hemolysis.
Q.295 What are the precautions to be taken before the transfusion of blood?
- Donor must be healthy without any infectious diseases like syphilis, hepatitis and AIDS
- Only compatible blood must be transfused
- Both matching and cross-matching must be done.
Q.296 What are the precautions to be taken while transfusing blood?
- Apparatus must be sterile
- The temperature of the blood must be the same as body temperature
- Transfusion must be done slowly to avoid the load on the heart.
Q.297 What is a blood substitute? Name some commonly used blood substitutes.
The substance infused in the body instead of whole blood is known as blood substitute. The commonly used blood substitutes are human plasma, 0.9% sodium chloride solution, 5% glucose solution, and some colloids like gum acacia, isinglass, albumin, and animal gelatin.
Q.298 What is exchange transfusion or replacement transfusion? What is its significance?
Exchange transfusion is the procedure that involves the removal of a patient’s blood and replacing it with fresh donor blood or plasma. It is an important life-saving procedure usually done to decrease or remove the effects of severe jaundice or changes in the blood like sickle cell anemia.
Q.299 What is the normal blood volume?
5 liters in a young healthy adult weighing about 70 kg.
Q.300 Name some pathological conditions when blood volume decreases.
- Hemorrhage
- Fluid loss
- Hemolysis
- Anemia
- Obesity
- Hypothyroidism.
Q.301 Name some pathological conditions when blood volume increases.
- Hyperthyroidism
- Hyperaldosteronism
- Cirrhosis of liver
- Congestive heart failure.
Q.302 How is blood volume regulated?
Blood volume is regulated by renal mechanism and hormonal mechanism which are controlled by the hypothalamus.
Q.303 What is the reticuloendothelial system?
The reticuloendothelial system is a system of primitive cells, which play an important role in the formation of blood cells, the destruction of blood cells, and the defense mechanism of the body.
Q.304 What is macrophage?
A macrophage is a large cell that has the property of phagocytosis.
Q.305 What are the two types of cells (macrophages) found in the reticuloendothelial system?
- Fixed cells – tissue macrophages (fixed histiocytes) present in pleura, omentum, mesentery, endothelium of blood sinusoids, reticulum of spleen and liver, meningocytes, microglia in brain, lungs, and subcutaneous tissue
- Wandering cells – free histiocytes present in blood (neutrophils and monocytes) and solid tissues like connective tissue.
Q.306 What are the tissue macrophages?
The fixed reticuloendothelial cells present in the tissues are called tissue macrophages or fixed histiocytes.
Q.307 What are the functions of the reticuloendothelial system?
Most of the functions of the reticuloendothelial system are carried out by tissue macrophages.
The functions are:
- Phagocytosis
- Secretion of bactericidal agents
- Secretion of interleukins
- Secretion of tumor necrosis factors
- Secretion of transforming growth factor
- Secretion of colony stimulation factor
- Secretion of platelet-derived growth factor
- Removal of carbon particles and silicon
- Destruction of senile RBC
- Destruction of hemoglobin
- Hemopoietic function.
Q.308 What are the functions of the spleen?
- Formation of blood cells
- Destruction of blood cells
- Blood reservoir function
- Role in defense mechanism of the body.
Q.309 What is splenomegaly and hypersplenism?
Enlargement of the spleen is called splenomegaly and increased activities of the spleen is called hypersplenism.
Q.310 Name some causes of splenomegaly.
- Infectious diseases
- Inflammatory diseases
- Pernicious anemia
- Liver diseases
- Hematological disorders
- Cysts in spleen
- Hodgkin’s disease
- Glandular fever.
Q.311 What is asplenia?
The absence of normal functions of the spleen is called asplenia.
Q.312 What is the lymphatic system? And what is lymph?
The lymphatic system is a closed system of lymph channels or lymph vessels. And lymph is a tissue fluid.
Q.313 What is the composition of lymph?
Lymph contains 96% of water and 4% of solids. Solids are organic and inorganic substances.
Organic substances:
- Proteins – albumin, globulin, fibrinogen, prothrombin, clotting factors, antibodies, and enzymes
- Lipids – chylomicrons and lipoproteins
- Carbohydrate – glucose
- Amino acids
- Nonprotein nitrogenous substances – urea and creatinine.
Inorganic substances: Sodium, calcium, potassium, chlorides, and bicarbonates.
Q.314 What do you mean by secretors and nonsecretors?
The A and B antigens are also present in other tissues like the liver, pancreas, kidney, etc. and also in body fluids like saliva, semen, etc. The individuals who have a high concentration of these antigens in their body fluids are called secretors and those having low concentration of these antigens in their body fluid are known as nonsecretors.
Q.315 What are human leukocyte antigens (HLA) and what is their importance?
HLA are the antigens present on the surface of WBCs. HLA typing is done before tissue or bone marrow transplant since they are responsible for the early rejection of the transplant.
Q.316 Name the factors promoting erythropoiesis.
These are hypoxia, iron, porphyrin, traces of copper, cobalt, protein, vitamin-C, thyroxin, hematinic principle, maturation factor, etc.
Q.317 Why we do not make an immunological response of our own body proteins?
The body has got the capacity to identify it’s own ‘self’ protein against of which no immunological response is evoked.
Q.318 What are the functions of lymph?
- Return of proteins from tissue spaces to blood
- Redistribution of fluid in the body
- Removal of substances like toxins and bacteria
- Maintenance of structural and functional integrity of tissues
- Serves as the route for absorption of fat
- Transport of lymphocytes.
Q.319 What are the functions of lymph nodes?
- Filtration of lymph
- Destruction of bacteria and toxic substances by acting like defense barriers.
Q.320 Name the main extracellular fluid cation.
It is sodium.
Q.321 Name the main anions in extracellular fluid.
These are chloride and bicarbonate.
Q.322 Which is the main intracellular fluid cation?
It is potassium.
Q.323 What is the average pH of extracellular fluid?
It is 7.4.
Q.324 What is the normal average capillary pressure at the arterial end?
It is 32 mm Hg.
Q.325 What is the normal average capillary pressure at the venous end?
It is 12 mm Hg.
Q.326 Name the various of RES in the body.
These are Kupffer cells in the liver: endothelium and reticulum cells in the spleen; reticulum cells in the bone marrow and lymph glands; histiocytes in the serous membrane, and cells in capsules of suprarenal glands and anterior pituitary body.
Q.327 Of the lymph and the tissue fluid which has more protein content?
It is the lymph. The protein content of tissue fluid is almost negligible.
Q.328 What is the rate of lymph flow?
It is 1-1.5 ml/min.
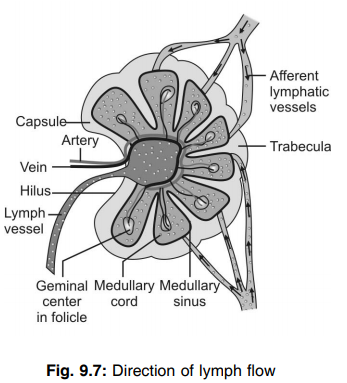
Q.329 What is the most important function of lymphatic circulation?
It is the removal of proteins from interstitial spaces, without which it is very difficult for the person to survive.
Q.330 What is tissue fluid?
Tissue fluid is the interstitial fluid that forms about 20% of the total body water.
Q.331 What are the functions of tissue fluid?
- It acts as a medium for the exchange of various substances between the cells and the blood in capillaries.
- It functions as a medium for the exchange of respiratory gases.
Q.332 How is tissue fluid formed?
Tissue fluid is formed by means of a process called filtration.
Q.333 How is the volume of tissue fluid regulated?
The volume of tissue fluid is regulated by the process of reabsorption.
Q.334 What is edema?
The swelling due to excessive accumulation of fluids in the tissues is called edema.
Q.335. Name the types of edema.
- Intracellular edema – collection of fluid inside the cell
- Extracellular edema – collection of fluid outside the cell. Q.336 What are the causes for intracellular edema?
- Malnutrition
- Poor metabolism
- Inflammation of tissue.
Q.337 What are the causes of extracellular edema?
- Increased capillary pressure
- Decreased amount of plasma proteins
- Obstruction of lymph flow.
Q.338 Name some common clinical conditions when extracellular edema occurs.
- Heart failure
- Renal disease
- Hypoproteinemia.
Q.339 What is pitting edema?
When the area of edema is pressed by a finger, displacement of fluid occurs producing a depression or pit. The pit remains for few seconds to one minute till the fluid flows back into that area. This type of edema is called pitting edema.
Q.340 What is nonpitting edema? What is its cause?
When the area of edema is pressed by a finger, there is no displacement of fluid or development of a depression or pit and the area remains hard. This type of edema is called nonpitting edema. This occurs because the accumulated fluid is bound in a proteoglycan meshwork, which is hard. So, the fluid is not displaced when the area is pressed. The nonpitting edema also occurs due to swelling of the cells or clotting of interstitial fluid in the presence of fibrinogen.
Also read: Physiology Questions & Answers

Comments (0)