Cardiovascular Physiology (Viva)
Q.1 What structural characteristics of cardiac muscle enable its continuous rhythmic contractions?
These are: Presence of pacemaker cell that initiates autorhythmicity, presence of special conductive tissue, and presence of free branchings between the muscle fibers (syncytium) ensure the quick passage of impulse from pacemaker cell to all parts of the heart to initiate continuous rhythmic contractions.
Q.2 Name the special conducting tissues of the heart.
SA node, AV node, bundle of His and Purkinje fibers 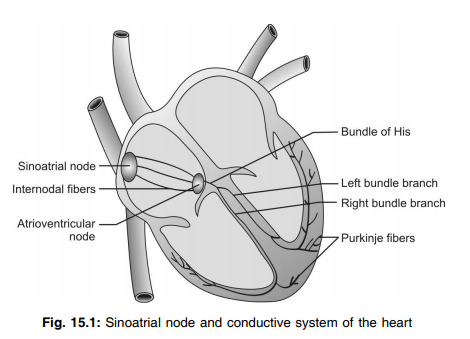
Q.3 What is a cardiac pacemaker?
SA node is called as the cardiac pacemaker because it is made up of ‘P’cells which can generate the impulse more rapidly than any of the pacemaker tissue of the heart and thereby determine the rate at which the heartbeats.
Q.4 What is the law of heart muscle?
It states that the size of muscle fibers, glycogen content, and rate of conduction increases from nodal to Purkinje’s fiber whereas the length of systole, duration of the refractory period, and rhythmicity increases in the reverse direction.
Q.5 What is intercalated disc and what is its importance?
At the point of contact of two cardiac muscle fibers, extensive folding of the cell membrane occurs which is known as intercalated discs. They provide a strong union between fibers so that the pull of one contractile unit can be transmitted to the next, thereby helps in increasing the force of contraction.
Q.6 What is the role of gap junction in cardiac muscle?
Gap junction is present in the intercalated disc of cardiac muscle fibers and helps in the rapid transferring of electrical currents, ions, etc. from one cell to another without coming in contact with ECF. Thus they provide low resistance bridge for the rapid spread out of electrical impulse, thereby helps the cardiac muscle to act as syncytium (functional).
Q.7 Name the valves and their location.
There are 4 valves—two in between the atria and ventricles known as atrioventricular valves (A-V valves) and two are at the opening of the blood vessels arising from the ventricles (semilunar valves).
A-V valves:
These are present in between the atria and ventricles. The valve present in between the right atria and right ventricle is known as the Tricuspid valve and the valve present in between the left atria and left ventricle is known as the Bicuspid valve.
Semilunar valves:
There are two semilunar valves namely the Pulmonary valve and the Aortic valve. The pulmonary valve is present at the pulmonary orifice which leads from RV to pulmonary artery and the aortic valve is present at the aortic orifice which leads from LV to the aorta.
Q.8 Name the special junctional tissues and their conduction rate.
The special junctional tissues and their rate of impulse generating capacity are:
| Special junctional tissues | Impulse generating capacity |
| S A Node | 75 ± 5 times/min |
| A V Node | 60 times/min |
| Bundle of His | 40 times/min |
| Purkinje’s fiber | 20 times/min |
Q.9 What do you mean by pacemaker potential or diastolic depolarization?
The pacemaker tissue is characterized by unstable RMP due to slow depolarization resulting from leakage of Na+ from outside to inside through Na+ leak channels. This show leakage of Na+ inside the cell causes an increase in electropositively inside the cell which ultimately enables to induce another action potential easily. This slow polarization in between action potential is known as prepotential or pacemaker potential or diastolic depolarization.
Q.10 Why SA node is called as cardiac pacemaker?
SA node acts as a pacemaker of the heart because the rate of impulse generation in a normal heart is determined by this node because of its highest rate of impulse generating capacity (75 ± 5 times/min) than other junctional tissues. This is why it is known as a cardiac pacemaker.
Q.11. What is an ectopic pacemaker?
When the pacemaker is other than SA Node (e.g. AV node, etc.) it is called as ectopic pacemaker.
Q.12 What is the duration of refractory period in cardiac muscle?
Refractory period is very long in cardiac muscles. It is about 0.53 seconds. In this, the absolute refractory period is 0.27 seconds and the relative refractory period is 0.26 seconds.
Q.13 What is the significance of the long refractory period in cardiac muscles?
Due to the long refractory period, the complete summation of contractions, fatigue, and tetanus do not occur in cardiac muscle.
Q.14 What do you mean by nodal and idioventricular rhythm?
The AV node takes the charge of generating impulse rhythmically when the SA node does not work. In this condition atria and ventricles beat almost simultaneously at the rate of 60 times per min. This rhythm of the heart is known as Nodal rhythm. Whereas 2nd Stannius ligature applied over the A-V groove makes the atria to continue beating with its own rhythm whereas the ventricle stops beating due to blockage of impulse from atria to ventricles. After sometime ventricle generates it’s own impulse and starts beating at a much slower rate. This rhythm of heartbeat in which atria and ventricular beating do not follow any specific pattern is known as idioventricular rhythm.
Q.15 What is AV delay? What is its significance?
When the impulse reaches to AV node, there is a delay of about 0.1 sec to pass the impulse to the bundle of His. This time gap is known as AV delay. It allows the atria to contract just ahead of ventricular contraction thereby atria is emptied before ventricular ejection.
Q.16 What is Frank-Starling's law?
Within the physiological limit the larger the initial length of muscle fiber (end-diastolic fiber length), the greater will be the force of contraction of the heart which is known as Frank-Starling's law of the heart.
Q.17 What is the ionic basis of the plateau phase of the cardiac action potential?
Immediately after depolarization voltage-gated Na+ channels used to close the resulting stoppage of entry of Na+ ions and voltage-gated K+ channel start opening resulting exit of K+. These results in a rapid fall of electropositivity initially known as rapid repolarization. Afterward, the rate of repolarization becomes slower due to the prolonged opening of voltage-gated Ca+2 channel through which Ca+2 enters inside. Thus the exit of K+ is almost counterbalanced by the entry of Ca+2 resulting sustained depolarization known as the plateau phase.
Q.18 Enumerate the properties of cardiac muscle.
- Excitability
- Rhythmicity
- Conductivity
- Contractility
Contractility includes:
– All or none law
– Staircase phenomenon
– Summation of subliminal stimuli
– Refractory period.
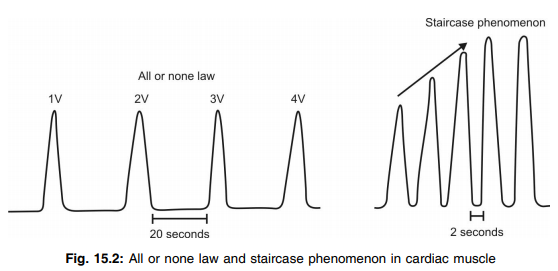
Q.19 Is all or none law applicable in the heart?
All or none law which states that if a stimulus is applied, whatever may be the strength of stimulus, the cardiac muscle responds maximally or it does not give any response at all. Of course, it is applicable only in whole atrial muscle (i.e. atrial syncytium) or in whole ventricular muscle (i.e. ventricular syncytium) not to a single cardiac muscle fiber.
Q.20 Define staircase phenomenon. Why does it occur?
If stimuli are applied repeatedly, with an interval of 2 seconds to the cardiac muscles, the force of contraction increases gradually for the first few contractions. Later the force remains the same. The gradual increase in the force of contraction is known as the staircase phenomenon or treppe response. It occurs because of the short interval of 2 seconds in between the stimuli. During this period, the beneficial effect is produced and this facilitates the force of successive contraction
Q.21 Why left ventricular subendocardial region is more prone to myocardial infarction?
The blood supply to the cardiac muscle in different areas of the heart is not the same. On the surface of the cardiac muscle, there are large epicardial arteries supplying more blood to those areas whereas in the subendocardial region blood supply is less because it is supplied by smaller intramuscular arteries and plexus of the subendocardial artery the diameter of which are less. This blood supply to the subendocardial plexus is further reduced during systole. Therefore the subendocardial region is more prone to myocardial infarction. Again as the left ventricular thickness is much more than that of the right ventricle the occlusion is more severe in the left ventricle. For this region LV subendocardial region is more prone to MI.
Q.22 What are the importance of anastomotic channels in heart muscle?
In the normal heart, there are some collaterals among the smaller arteries which become active under abnormal conditions like myocardial ischemia. They open up within a few seconds after the sudden occlusion of the larger artery and become double in number by the end of 2nd or 3rd day and reach to normal by one month. When atherosclerosis causes constriction of coronary arteries slowly over a period of many years, collateral vessels develop restoring normal blood and thus the patient never experiences acute episodes of cardiac dysfunction.
Q.23 What is the importance of autoregulation in blood supply in heart muscle?
Like some other organs, the heart has the capacity to regulate its own blood flow up to a certain limit in order to maintain an almost constant blood flow to the cardiac musculature in spite of any alteration of systemic blood flow. This is known as autoregulation of coronary blood supply.
Q.24 What is angina pectoris?
Due to myocardial ischemia, there is the stimulation of nociceptors present in the heart muscle resulting in pain sensation which is normally referred to as upper sternum, left forearm, left shoulder, neck, and side of the face. This clinical condition is known as angina pectoris.
Q.25 Why cardiac muscle cannot be tetanized?
It is because of it's long absolute refractory period and thus summation of contractile response is not possible which is essential for the tetanization of heart muscle.
Q.26. What is a cardiogram?
The record of the mechanical activity of the heart is known as cardiogram.
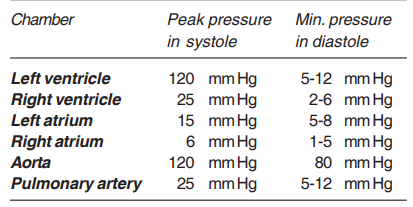
Q.27 Mention the maximum and minimum pressure in the heart during systole and diastole?
Q.28 Define and give normal values of end-diastolic volume, stroke volume, and end-systolic volume.
During ventricular diastole, the intraventricular volume is increased which results filling of the ventricles. At the end of the diastole, the amount of blood-filled by the ventricle is known as end-diastole volume (EDV).
It is about 120-130 ml.
During ventricular systole intraventricular volume decreases which results increase in pressure thus ejection of blood out of ventricles. During each systole, the amount of blood pumped out by each ventricle is known as stroke volume (SV).
Normal value:70 ml/beat.
At the end of the systole however, some amount of blood remains in each ventricle which is known as end-systolic volume (ESV).
The normal volume: 50-60 ml/ beat.
Q.29 What do you mean by vagal escape? What is its cause?
If strong vagal stimulation to the heart is continued then after a pause the ventricles resume to beat at a slow rhythm which is called a vagal escape. During prolonged vagal stimulation right auricle stops beating and distends due to blood overflow which leads to the fall of BP → afferent impulse from the carotid sinus to cardiac centers → stimulate ventricles to start its beat.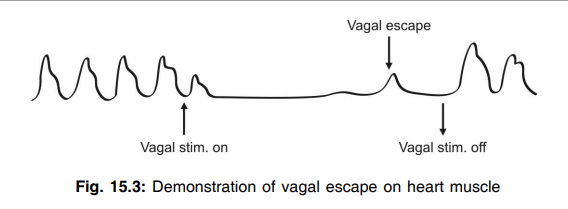
Q.30 What is the action of sympathetic nerves on the heart?
Sympathetic nerves increase the rate and force of contraction of the heart by secreting noradrenaline.
Q.31 What is sympathetic tone?
A continuous stream of accelerator impulses that arises from the cardio accelerator center and reaches the heart via sympathetic nerves is known as sympathetic tone or cardio accelerator tone. However, under resting conditions, the vagal tone is more dominant over the sympathetic tone.
Q.32 Define apex beat.
Apex beat is the impulse or throb which is felt and seen on the chest wall normally in the left 5th intercostal space just medial to left nipple.
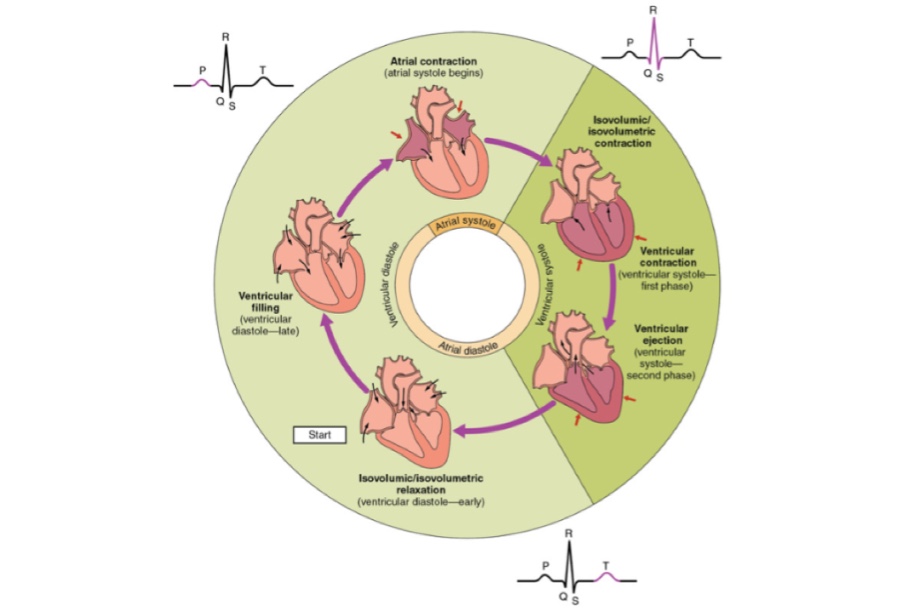
Q.33 Name different phases of the cardiac cycle. Mention the duration of each phase.
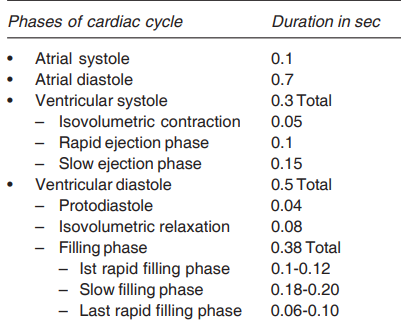
Q.34 What is protodiastole? Is it part of systole or diastole?
Protodiastole is the very brief phase before diastole in which ventricular systole has ceased but relaxation yet to start.
It can not be well defined whether the protodiastole is a part of systole or diastole as some workers include it in diastole as muscle contraction is stopped at this phase whereas some others believe that it is a part of systole as muscle relaxation has not yet started.
Q.35 Define cardiac cycle.
The sequence of events (mechanical, electrical, etc.) associated with consecutive heartbeat is repeated cyclically which is known as the cardiac cycle. The normal duration is 0.8 sec if the heart rate is 75 beats/ min.
Q.36 What are the causes of 1st heart sound?
These are:
- Closure and vibrations of AV valves at the beginning of ventricular systole.
- Vibrations of blood surrounding the AV valves.
- Vibrations of major blood vessels around the heart.
- Vibrations of walls of heart.
Q.37 What are the characteristics of 1st heart sound?
It is:
- Soft, prolonged with low pitch.
- Duration is 0.12 sec and occurs in peak or downstroke of R wave in ECG and just before the onset of ‘c’ wave in jugular pulse tracing.
- Best heard at the apex beat area and is associated with the onset of ventricular systole.
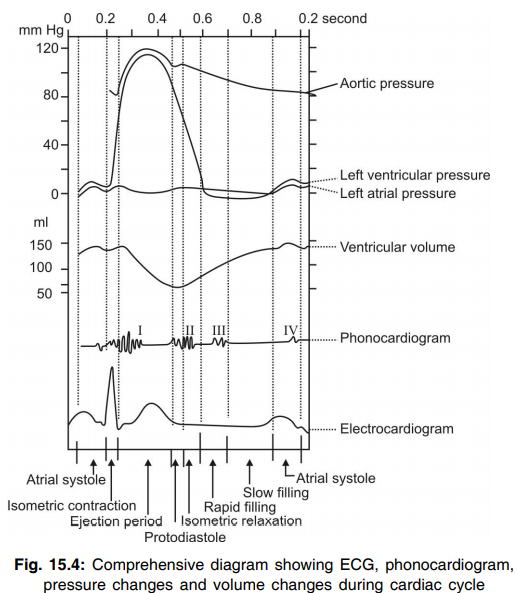
Q.38 What is the significance of 1st heart sound?
It indicates the force of contraction, condition of myocardium, and competence of AV valves.
Q.39 What are the causes of 2nd heart sound?
These are: Closure and vibration of semilunar valves at the end of ventricular systole. Vibrations of blood surrounding these valves.
Vibrations of walls of aorta and pulmonary artery. Vibrations of the wall of ventricles to a little extent. Q.40 What are the characteristics of 2nd heart sound?
It is:
- Sharp, short and high pitched.
- Duration is 0.08 sec and follows T wave in ECG and coincides with ‘v’ wave in jugular venous pulse tracing.
- Best heard at 2nd right costal cartilage for aortic component and 2nd intercostal space at the left sternal border for the pulmonary component.
- Associated with the onset of ventricular diastole.
Q.41 What is the significance of 2nd heart sound?
It indicates the competence of semilunar valves.
Q.42. When and how 3rd heart sound is produced?
3rd heart sound is produced during the first 1/3 of ventricular diastole. It occurs due to the vibrations set up by the rushing of the blood during the rapid filling phase of the ventricular diastole.
Q.43 Differentiate 1st and 2nd heart sound.
| 1st heart sound | 2nd heart sound |
| It is prolonged, low pitched and soft. | It is sharper, abrupt, clear, and high pitched |
| Coincides with carotid pulse | Does not coincide |
| Coincides with R wave of ECG | May precede, coincide or follow the T wave of ECG. |
| Best heard over mitral area | Best heard over the aortic and pulmonary areas. |
| The time interval between 1st and 2nd is shorter | The time interval between 2nd and next 1st is comparatively longer |
Q.44 What is murmur?
It is the sound produced by turbulence produced in the blood by a forward flow through a stenosed (narrowed) valve or backflow (regurgitation) through a deformed or incompetent valve.
Q.45. How do you classify murmur?
It will be classified on the basis of their relationship with main heart sounds like presystolic, systolic, diastolic, and also to and fro murmurs.
Q.46 What are the maximum and minimum pressure in the heart?
The maximum pressure in the left ventricle is above 120 mm Hg.
Max pressure in the right ventricle is above 25 mm Hg
The minimum pressure in the left ventricle is 80 mm Hg.
The minimum pressure in the right ventricle is a few mm Hg.
Q.47 What is the normal heart rate? What are the factors affecting heart rate (HR)?
The normal value of HR is 72 beats/min with the normal range 60-90 beat/min. The factors are: age, sex, body temperature, hypoxia, emotion, exercise, etc. and drugs like epinephrine and norepinephrine.
Q.48 Why HR is slightly higher in females than males?
It is because of two reasons:
- Lower systemic BP
- More resting sympathetic tone.
Q.49 What is the Cushing reflex?
It is represented by the following sequential events:
Increased intracranial pressure → decreases blood supply to medullary hypoxia and hypercapnia → stimulation of medullary vasomotor center → increase of systemic BP → stimulation of baroreceptors → stimulation of vagus nerve → decrease of HR and respiration. This reflex mechanism by which increased intracranial pressure results bradycardia is known as the Cushing reflex.
Q.50 What do you mean by sinus arrhythmia?
Heart rate increases with inspiration and decreases during expiration. This phenomenon is known as sinus arrhythmia.
Q.51 State Marey’s law.
If the other conditions remain constant then the HR is inversely related to systemic BP

Q.52 Define cardiac output, stroke volume, and cardiac index.
Cardiac output:
The amount of blood pumped out by each ventricle per min is called as cardiac output.
The normal value is 5 lit/min/ventricle.
Stroke volume:
The amount of blood pumped out by each ventricle in each beat is known as stroke volume.
Normal value is 70 ml/beat/ventricle.
Cardiac index:
It is the cardiac output per square meter of body surface area.
The normal value is 3.2 L/m2 /min.
Q.53 What do you mean by extrinsic and intrinsic autoregulation of cardiac output?
If cardiac output is controlled by controlling only heart rate (as CO = HR × SV) it is known as extrinsic autoregulation of cardiac output whereas if it is regulated by regulating only stroke volume, it is known as intrinsic autoregulation.
Q.54 What is the difference between heterometric and homometric regulation of cardiac output?
To control cardiac output when ventricular contraction is regulated by controlling the initial length of the muscle fiber, i.e. EDFL, then it is called as heterometric regulation which is independent of cardiac nerves. Whereas when cardiac nerves regulate the myocardial contractility to control the cardiac output, it is known as homometric regulation of cardiac output.
Q.55 What is Frank-Starling’s law of heart? What is its relation with venous return?
It states that within the physiological limit, the force of ventricular contraction is directly proportional to the initial length of muscle fibers (EDFL). If venous return is increased the EDFL of the ventricular muscle is also increased resulting in more force of ventricular contraction thereby more cardiac output.
Q.56 What do you mean by Vis A Tergo and Vis A Fronte in relation to cardiac pump?
Vis A Tergo is the force that drives the blood forward from behind, e.g. the contraction of the heart drives the blood in the forward direction, whereas Vis A Fronte is the force acting from the front that attracts blood in the veins towards the heart, e.g. ventricular systolic and diastolic suction pressure.
Q.57 Enumerate the factors affecting venous return.
The factors are: Thoracic or respiratory pump, cardiac pump, muscle pump, total blood volume, and increased sympathetic activities on veins.
Q.58 Name two methods by which cardiac output is measured.
These are:
- Direct Fick method and
- Indirect dye dilution method.
Q.59 Enumerate Fick’s principle.
It states that the amount of a substance taken up by an organ or by whole body per unit time is equal to the arterial level of that substances minus the venous level (i.e. A-V difference) times the blood flow,
i.e. amount of substance taken/min = A-V difference of the substance × blood flow/ min.
Q.60 What are the disadvantages of Fick’s method?
These are:
- As it is an invasive method the subject is exposed to all risk of hemorrhage, infection, etc.
- As the subject is conscious of the whole technique cardiac output may be higher than normal.
Q.61 Which dye is generally used in the Dye dilution method and why?
It is generally Evans blue or radioactive isotopes.
Criteria for selection are as follows:
- These stay in the circulation during the test.
- These are not harmful and not toxic.
- Do not alter the hemodynamics of blood flow.
- Concentration of these substances can be easily measured.
- Excreted totally and neither reabsorbed nor secreted by the body.
Q.62 What is Ballistocardiogram?
It is a record of the to and fro movements of the body in the headward to forward direction when the subject lies on a suitably suspended table. This is another method of measuring cardiac output though it is now absolute.
Q.63. What is Bundle of KENT?
In the individuals with WPW syndrome, there is one additional nodal connecting tissue in between the atria and ventricles besides the AV node which conducts the impulse more rapidly than the AV node. This additional conducting pathway is known as Bundle of KENT.
Q.64. Define blood pressure (BP).
It is the lateral pressure exerted by the moving column of blood on the wall of blood vessels during its flow.
Q.65 Define systolic, diastolic, mean, and pulse pressure with each of their normal average values.
Systolic pressure (SP):
It is the maximum pressure exerted during the systole of the heart.
Normal value = 120 mm Hg (Normal range:110-140 mm Hg).
Diastolic pressure (DP):
It is the minimum pressure during diastole of the heart.
Normal value = 80 mm Hg (Normal range: 60-90 mm Hg).
Pulse pressure (PP):
Pulse pressure is the difference between systolic and diastolic pressure.
Normal value = 40 mm Hg.
Mean pressure:
It is average pressure during each cardiac cycle.
Normal value = 93.3 mm Hg.
Q.66 Enumerate the significance of SP, DP, PP, and MP.
Systolic pressure indicates the extent of work done by the heart and also the force with which the heart is working. It also indicates the degree of pressure the arterial wall has to withstand.
Diastolic pressure is the measure of the total peripheral resistance and it indicates the constant load against which the heart has to work.
Pulse pressure determines the pulse volume. Whereas mean pressure indicates the perfusion pressure head which causes the flow of blood through the arteries, arterioles, capillaries, veins, and venules.
Q.67 Why does systolic pressure increase after meal?
After meal pressure over the heart increases due to distended abdomen which in turn increases heart rate and also there is a release of epinephrine which also increases systolic blood pressure.
Q.68 What do you mean by baroreceptors? Where are they located?
Baroreceptors are the pressure receptors stimulated in response to the change of pressure around them. These are located in the wall of blood vessels (e.g. arterial baroreceptor–present in the carotid sinus, aortic arch, root of right subclavian artery, junction of thyroid artery with common carotid artery, also pulmonary trunk) and also in the walls of the heart (e.g. atriocaval receptors, atrial receptors).
Q.69 What do you mean by buffer nerves? Why they are so-called?
The carotid sinus nerve originated from the carotid sinus and the aortic nerve arose from the arch of the aorta are collectively known as buffer nerves as they prevent any change in systemic BP and thus help the BP to keep normal.
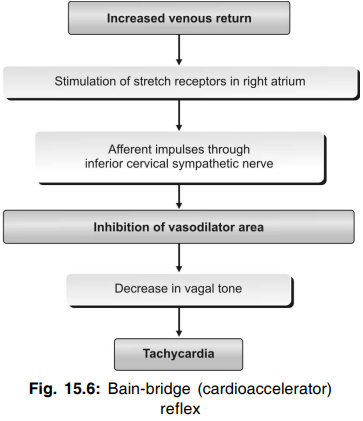
Q.70 What is Bain-bridge reflex?
Rapid injection of blood or saline in anesthetized animals produces a rise in heart rate if the initial heart rate is low. This is called as Bain-bridge reflex. This is due to the stimulation of stretch receptors in the wall of the right atrium.
Q.71 Name different chemoreceptors responsible for BP regulation. What are their stimulants?
These are carotid bodies and aortic bodies. They get stimulated by hypoxia, hypercapnia, asphyxia, and also acidemia.
Q.72 What is the effect of chemoreceptors on heart rate?
In conditions like hypoxia, hypercapnia, and increased hydrogen ion concentration, the chemoreceptors send inhibitory impulses to the vasodilator area (cardioinhibitory center). Now, the vagal tone is reduced and the heart rate is increased.
Q.73 Sudden standing increases diastolic BP—explain how?
On standing there is peripheral pooling of blood in lower parts of the body → lowering of venous return to the heart → decrease cardiac output → thereby decrease systolic BP → leads to decrease baroreceptor discharge → thereby increases sympathetic activity → results increase of the total peripheral resistance due to vasoconstriction → ultimately leads to an increase of diastolic pressure.
Q.74 If mean BP is decreased to 60 mm Hg then what compensatory mechanism will operate to bring it to normal?
Both the baroreceptor mechanism (which operates in between 60-200 mm Hg mean blood pressure) and chemoreceptor mechanism which operates between 40-100 mm Hg of mean BP.
Q.75 If BP is decreased to 40 mm Hg then which compensatory mechanism will start into action?
Both chemoreceptor mechanism and CNS ischemic response.
Q.76 If mean BP is increased to 140 mm Hg then what compensatory mechanism will be operated?
Only baroreceptor mechanism.
Q.77 What do you mean by stress relaxation and reverse stress relaxation mechanisms in relation to BP regulation?
Rise in arterial BP due to intravenous transfusion of blood increases perfusion pressure in blood storage organs that causes relaxation of blood vessels, thereby decreases venous return and thereby decreases cardiac output. This leads to a decrease in BP to a normal level. This mechanism is known as stress relaxation. The opposite phenomenon is known as the reverse stress relaxation mechanism which is as follows: Prolonged bleeding causes a decrease of BP → thereby decreases perfusion pressure → leads to vasoconstriction of blood storage organs → results in an increase of venous return and thus increases cardiac output → which in turn increases BP to a normal level.
Q.78 What is hypertension? What do you mean by systolic hypertension and white coat hypertension?
Chronic elevation of blood pressure beyond 140/90 is generally labeled as hypertension.
In advanced age, due to loss of elasticity of blood vessels, stretching of the wall of blood vessels decreases which results in increment of pressure during systole with normal diastolic pressure. This condition is known as systolic hypertension which is characterized by high pulse pressure. Some hypertensive patients because of nervousness, have higher BP in the clinician’s chamber than during their normal day time activity. This condition is known as white coat hypertension.
Q.79. What do you mean by malignant hypertension?
In some patients the blood pressure especially the diastolic pressure is increased to a very high level (>120 mm Hg) within a short period. This condition is known as malignant hypertension.
Q.80 Which pressure is considered better to judge the hypertension–SP or DP? Justify your answer.
Clinically diastolic pressure is more useful to characterize the state of hypertension because diastolic pressure is comparatively constant and does not fluctuate like SP in response to day-to-day activity.
Q.81 What do you mean by labile hypertension?
In the early stages of essential hypertension, systolic BP fluctuates. This is why it is referred to as labile hypertension.
Q.82. What is hypotension?
Chronic low BP especially the diastolic pressure below 60 mm Hg is called hypotension.
Q.83. What do you mean by postural hypotension?
In some hypotensive patients, sudden standing causes a further fall of systemic BP that may result in dizziness, dimness of vision, and even fainting. This is known as postural hypotension.
Q.84 What is the difference between pulse pressure and pressure pulse?
Pulse pressure is the difference of systolic and diastolic pressure whereas the pressure pulse or pulse is the wave transmitted to the arteries like radial arteries due to stretching and relaxation of a wall of the aorta in response to the ventricular ejection of blood and ventricular filling respectively during the cardiac cycle.
Q.85. What is the purpose of doing an exercise tolerance test?
It is for determining the efficiency of the heart as a pumping organ.
Q.86 What is isometric (isovolumetric) contraction of the heart?
The period during which the ventricles of the heart contract as closed cavities (because all the valves are closed) without any change in the volume of ventricular chambers or in the length of muscle fibers is known as isometric (isovolumetric) contraction. During this period, the pressure increases very much.
Q.87 What is the significance of isometric contraction of the heart?
During isometric contraction, the pressure in the ventricles is greatly increased. When the ventricular pressure increases more than the pressure in the aorta and pulmonary artery the semilunar valves open. Thus, the high pressure developed during isometric contraction is responsible for the opening of semilunar valves leading to the ejection of blood from the ventricles.
Q.88 What is isometric or isovolumetric relaxation of the heart?
The period during which the ventricles of the heart relax as closed cavities (because all the valves are closed) without any change in the volume of ventricular chambers or in the length of muscle fibers is known as isometric or isovolumetric relaxation. The pressure decreases very much during this period.
Q.89 What is cardiac reserve?
It is the difference between the basal cardiac output of an individual and the maximum cardiac output that can be achieved in that person. It is also expressed as cardiac reserve percent.
Q.90 By observing HR can you predict the intensity of exercise or work done by a person?
Yes,- If HR is 150; it will be severe exercise.
Q.91 Where do you find physiological bradycardia?
It is seen in athletes, during sleep and meditation.
Q.92. What is apex-pulse deficit?
Normally the pulse rate and heart rate are identical but in some cases like extrasystoles and atrial fibrillations, some of the heartbeats are too weak to be felt at the radial artery resulting in missing of that particular pulse. This causes a higher heart rate than the pulse rate. This condition is known as apex pulse deficit or pulse deficit.
Q.93 Name the waves of normal arterial pulse tracing. What are their physiological basis?
In the normal arterial pulse recording, there is one steep upstroke called anacrotic limb and one rather slow downstroke called catacrotic limb. The end of the anacrotic limb and beginning of the catacrotic limb is designated as percussion wave (p). In the catacrotic limb, there is also a negative wave called dicrotic notch (n) followed by a positive wave called dicrotic wave. Besides this, sometimes after the peak of the tracing, there is another small wave called tidal wave (t).
The waves are represented by
- Percussion wave: It is due to the expansion of the artery for ventricular ejection during ventricular systole.
- Catacrotic limb: It is due to the normalization of the artery due to the slow passing of blood towards the periphery.
- Dicrotic notch: It is due to the backflow of the blood from the aorta towards the heart due to pressure difference during ventricular diastole.
- Dicrotic wave: It is due to increase pressure again in the aorta due to the prevention of backflow of blood towards the heart by closure of the aortic valve.
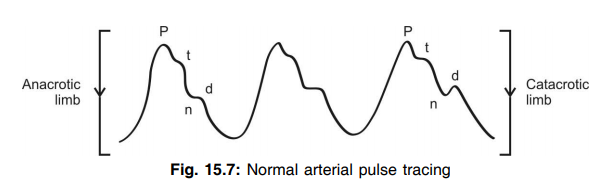
Q.94 Can you indicate the systolic and diastolic phases of the ventricle on the arterial pulse tracing?
Yes, the maximum ejection phase lasts from the start of the upstroke to the peak of ‘p’ wave while the reduced ejection phase lasts from the peak of ‘p’ wave to the peak of the dicrotic notch. The rest time period represents diastole.
Q.95. What is a dicrotic pulse?
There are two palpable waves—one in systole and another in diastole in congestive cardiomyopathy patients where stroke volume is low. This type of pulse is known as dicrotic pulse.
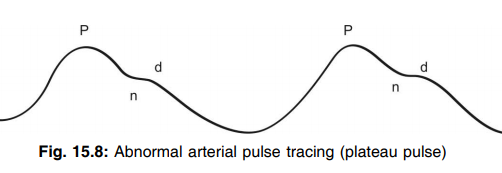
Q.96 What is plateau pulse?
During some pathological conditions like aortic stenosis, the pulse wave rises slowly, followed by a delayed and sustained peak and then the pulse faded slowly. Such type of pulse is known as plateau pulse.
Q.97 What is the anacrotic pulse?
Slow rising and slow fall of pulse wave due to prolonged ventricular ejection as occurs in aortic stenosis is known as anacrotic pulse.
Q.98 What do you mean by pulsus alterans and paradoxus?
Pulsus alterans is alternative weak and strong beating of pulse whereas the phenomenon when pulse disappears or becomes feeble during inspiration and becomes maximum during expiration is known as pulsus paradoxus.
Q.99 What is a water hammer pulse?
In some conditions like aortic regurgitation, there is a sharp and steep rise followed by sleep fall of pulse which is known as a water hammer pulse.
Q.100 How does jugular venous pulse record give the idea about right atrial pressure?
The jugular vein is connected directly with the right atrium and as there is no valve at the junction of the superior vena cava and right atrium, any change of right atrial pressure is directly transmitted to the jugular vein. That is why jugular venous pressure record gives the idea about right atrial pressure.
Q.101 Name the waves of jugular venous pulse and the causes of their onset.
The waves and their causes are as follows:
- ‘a’ wave – It is due to an increase in pressure within the atrium due to atrial systole.
- ‘c’ wave – It is due to increased pressure within the atrium due to the bulging of the tricuspid valve into the right atrium during the isovolumic ventricular contractile phase.
- ‘v’ wave – It is due to the rise in atrial pressure due to atrial filling before the tricuspid valve opens during diastole.
- X descends-It is due to the fall of intra-atrial pressure due to the descend of the tricuspid valves.
- Y descends-It is due to the fall of intraarterial pressure due to the opening of tricuspid valves to result in ventricular filling.
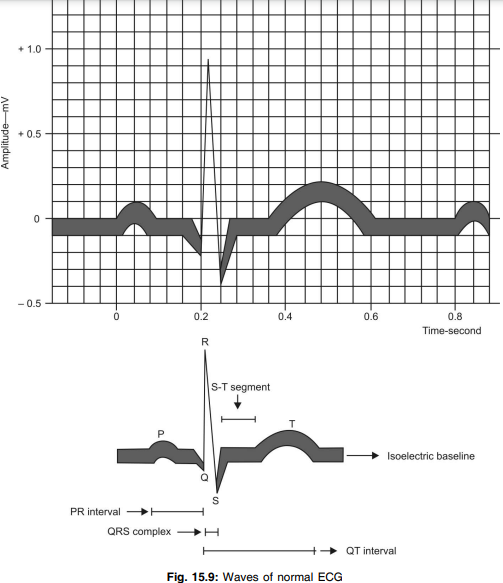
Q.102 Define ECG.
It is the record of electrical activities of the heart by electrocardiograph during different periods of the cardiac cycle.
Q.103 Enumerate the clinical significance of ECG.
Any abnormalities of the heart like ischemic heart disease, myocardial infarction, extrasystole, heart block, ventricular fibrillation and flutter, sinus arrhythmias, etc. are detected by the ECG record of the person.
Q.104 What does ‘P’ wave represent? What does it signify?
‘P’ wave represents the atrial depolarization. Any abnormalities of the ‘P’ wave means abnormality in the atria like a larger ‘P’ wave denotes the atrial hypertrophy.
Q.105 What do QRST and QRS represent? What is the duration of the ventricular complex?
QRST represents ventricular complex, i.e. ventricular depolarization and ventricular repolarization. The normal duration is 0.48 sec. QRS complex represents ventricular depolarization only.
Q.106 What do Q and RS waves indicate?
‘Q’ wave indicates the ventricular septal activity whereas the ‘RS’ wave indicates the excitation of ventricle proper with a duration of 0.08-0.1 sec.
Q.107 What is the significance of the T wave?
It is due to the repolarization of ventricles and its normal duration is 0.27 sec. It indicates the functional activity of the base of the heart. Clinically it signifies the myocardial damage in case of any abnormality in T wave.
Q.108 What does PR interval represent? What is its significance?
It represents atrial depolarization and conduction through the bundle of His. The normal duration is 0.13-0.16 sec. It is the interval from the beginning of the P wave to the beginning of the Q or R wave. Prolonged PR interval signifies the conduction block.
Q.109 What is TP interval and what is its significance?
It is the period from the end of the T wave to the beginning of the P wave of the next cardiac cycle. It represents the diastole or polarized state of the whole heart. The normal duration is 0.2 sec at a HR of 75/min.
Q.110 What is QT interval and what does it represent?
It is the interval from the beginning of the Q wave to the end of the T wave (Normal duration 0.40-0.43 sec). It represents ventricular events.
Q.111 What is ST interval? What does it represent?
The end of the S wave to the end of the T wave is known as the ST interval. The normal duration of which is 0.32 sec. It represents ventricular repolarization only.
Q.112 What is the ST segment? What is its significance?
Following the QRS there is a long isoelectric period which extends from the end of S wave to the beginning of the T wave called ST-segment. Any change of the position of ST-segment from the isoelectric line indicates the functional abnormalities of the heart. Deviation of ST-segment more than 2 mm up from the isoelectric line is called elevated ST-segment which is the clinical feature of MI. Similarly, deviation of the same more than 2 mm downward from the isoelectric line is called a depressed ST segment as seen in angina pectoris.
Q.113 Define lead.
The electrocardiographic connections, i.e. wires along with the electrodes to record ECG is known as lead.
Q.114 Classify leads.
Leads are classified as unipolar and bipolar leads which are again divided as follows:
- Unipolar lead
- Unipolar augmented limb lead
– aVR
– aVL
– aVF - Chest lead (V1-V6)
- Bipolar lead
– Standard limb lead—I
– Standard limb lead—II
– Standard limb lead—III
Q.115 Why unipolar lead is so called?
In this type of leads, one electrode becomes inactive (indifferent electrode) whereas the other one is active (exploring electrode). That is why it is known as a unipolar lead.
Q.116 What do you mean by rule of thumb?
It is the general observation in the ECG record obtained from chest leads as follows:
- As we pass across the chest leads (V1- V6) ‘R’ wave increases gradually in size and the ‘S’ wave becomes smaller gradually. In lead V3 both are equal.
- R wave in V6 and S wave in V1 represent left ventricular activity whereas R wave in V1 and S wave in V6 represent right ventricular activity.
Q.117 What is augmented limb lead? Why is it so-called?
Augmented limb leads are unipolar type limb leads with slight modification in the recording technique where one electrode (active) is connected to the positive terminal of the ECG machine and the other two are connected through electrical resistance to the negative terminal of the ECG machine.
It is so-called because the magnitude of different waves becomes larger by 50 percent than the same obtained from standard limb leads without any change of its normal pattern. These are classified as aVR, aVL, and aVF.
Q.118 What do unipolar chest leads represent?
V1 and V2 are associated with right atrial and ventricular activity respectively whereas V4, V5, and V6 represent left ventricular activity. V3 is regarded as a transitional zone.
Q.119 What do you mean by dextrocardiogram?
In case of damage to the left branch of the bundle of His, the impulse travels through the right branch to the right ventricle resulting in the predominant activity of the right ventricle. Such a record is called as dextrocardiogram.
Q.120 What is levocardiogram?
When the right branch of the bundle of His is damaged there is predominance of left ventricular activity. This type of record is called as levocardiogram.
Q.121 What do you mean by Einthoven’s triangle?
The equilateral triangle obtained by connecting the right arm, left arm, and right leg, by means of electrical wires with current source as the heart at its center is known as Einthoven’s triangle.
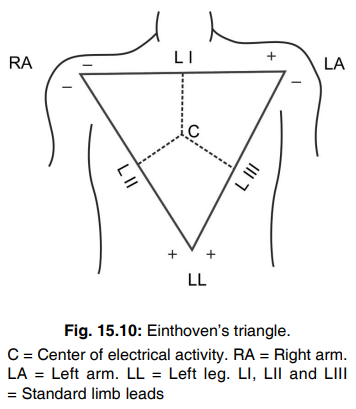
Q.122 What is Einthoven’s law?
It states that if the electrical potentials of any two of the three bipolar leads are known at any given instant, the 3rd one can be determined mathematically from the 1st two by simply summing the 1st two by considering the positive and negative signs of the different leads.
Q.123 What is J point? What is its significance?
J point is the endpoint of the S wave and beginning of ST-segment where no electrical activity of the heart exists. Normally the J point locates on the isoelectric line. Upward or downward deviation of this point indicates the heart diseases like MI and cardiac ischemia.
Q.124 What is a vector?
It is an arrow that points the direction of the electrical potential generated by the current flow with the arrowhead in a positive direction.
Q.125 Mention the characteristics of vector.
These are:
- Direction of current flow is represented by the arrowhead and
- Length of the arrow is drawn proportionate to the voltage of the potential.
Q.126 What do you mean by vector cardiogram?
The vector of current flow through the heart changes rapidly as the impulse spreads through the heart muscle.
These changes are:
- The vector increases and decreases in length because of the increasing and decreasing voltage of the vector.
- It also changes direction accordingly with the changes in the average direction of the electrical potential of the heart. The record that shows these changes in the vectors at different times during the cardiac cycle is called as vector cardiogram.
Q.127 What do you mean by the electrical axis of the heart or cardiac vector?
Since the standard limb leads I, II, III are records of the potential difference between two points, therefore, deflection in each lead at any point indicates the magnitude and direction in the axis of the electromotive force generated in the heart. This is called as electrical axis of the heart.
Q.128 What is the effect of change in the blood sodium concentration on the heart?
Increased sodium concentration in blood decreases the rate and force of contraction. Very high sodium concentration can stop the heart in diastole. A very low level of sodium produces low voltage waves in ECG.
Q.129 What is the effect of hyperkalemia on the heart?
Normal potassium concentration in serum is about 3.5 to 5 mEq/L. When it increases above 6 mEq/L (hyperkalemia) the resting membrane potential in cardiac muscle is decreased leading to hyperpolarization. It reduces the excitability of the muscle. ECG shows a tall T wave. The increased potassium concentration above 8 mEq/L affects the conductive system also. And in ECG, the P-R interval and the duration of the QRS complex are prolonged. During severe hyperkalemia (above 9 mEq/L), atrial muscle becomes unexcitable. So, in ECG, P wave is absent and the QRS complex merges with T wave. In experimental animals, increased potassium concentration stops the heart in diastole immediately.
Q.130 What is the effect of hypokalemia on the heart?
Hypokalemia (decrease in potassium concentration) reduces the sensitivity of the heart muscle. In ECG, the S-T segment is depressed. The amplitude of the T wave is reduced. In severe hypokalemia, the T wave is inverted. U wave appears. P-R interval is prolonged.
Q.131 What is the effect of hypercalcemia on the human heart?
Normal serum calcium level is 9 – 11 mg%.
In hypercalcemia, there is a reduction in the duration of the S – T segment and Q – T interval, with a slight increase in excitability and contractility.
Q.132 What is calcium rigor?
The stoppage of the heart in systole when a large quantity of calcium ion is infused in experimental animals is known as calcium rigor. It is a reversible phenomenon. When the calcium ions are washed, the heart starts functioning normally.
Q.133 What is the effect of hypocalcemia on the heart?
Hypocalcemia (reduction in serum calcium level) reduces the excitability of the cardiac muscle. In ECG, the duration of the S – T segment and Q – T interval is prolonged.
Q.134 What do you know about U wave in ECG?
It is rarely seen as a small positive round wave after the T wave. It is due to the slow repolarization of papillary muscles. It is more commonly seen in children.
Q.135 What do you mean by left and right axis deviation?
From the ECG record how can you assess whether any person is having left or right axis deviation? If the normal direction of the mean QRS vector falls in between –30° to +30°, it is called a left axis deviation which represents the horizontal position of the heart. Similarly, if it falls in between +75° to +110°, it is known as the right axis deviation which also represents the vertical position of the heart. Clinically axis deviations are made by finding the amplitude of the R wave in the bipolar leads as follows:
- If R wave is the tallest in lead II, it is the normal electrical axis of the heart (+59°).
- If R wave is the tallest in lead I, it is left axis deviation.
- If R wave is the tallest in lead III it is called as right axis deviation.
Q.136 What are the physiological left or right axis deviation? What is the clinical significance of the electrical axis of the heart?
Physiological left axis deviation is seen:
- During expiration
- When a person lies down
- If the person is stocky and fatty.
Physiological right axis deviation is seen:
- During inspiration
- When a person stands up
- Normally in tall and lanky people.
Clinical significance:
Hypertrophy of any ventricles and bundle branch block is indicated from the electrical axis of the heart. In patients with hypertrophy of left ventricle and left bundle branch block, left axis deviation is seen whereas, in hypertrophy of right ventricles and right bundle branch block patients, right axis deviation takes place.
Q.137 What is the extrasystole or premature contraction?
Sometimes, any part of the heart other than the SA node can produce an impulse. This is called an ectopic focus. The ectopic focus produces an extra beat of the heart, which is called extrasystole or premature contraction.
Q.138 What is a compensatory pause? What is its cause?
Extrasystole is always followed by a long pause where the heart stops. This temporary stoppage of heart, immediately after extrasystole is known as a compensatory pause. It occurs because the heart has to wait for the arrival of the next natural impulse from the pacemaker.
Q.139 What is the difference between 1st degree and 2nd-degree heart block?
When all atrial impulses reach the ventricles therefore atrial rate: ventricular rate becomes 1:1 but PR interval becomes longer than 0.2 sec, it is called as 1st-degree incomplete heart block.
Whereas when all atrial impulses are not conducted to the ventricles producing atrial and ventricular contraction at a rate of either 2:1 or 3:1 ratio with gradual lengthening of PR interval till one ventricular beat is missed, this type of heart block is known as 2nd-degree incomplete heart block.
Q.140 What do you mean by Wenckebach phenomenon?
In the case of 2nd-degree heart block, there is a gradual increase of PR interval until one ventricular beat is missed. This is known as Wenckebach phenomenon.
Q.141 What is 3rd-degree heart block? What do you mean by idioventricular rhythm?
Complete blockade of conduction of impulse from atria to ventricle is known as third-degree or complete heart block. In the case of complete heart block, the ventricle starts beating at its own rate, i.e. 45 beats/min which is independent to SAN. This rhythmic ventricular contraction is known as idioventricular rhythm.
Q.142 What is the difference between flutter and fibrillation?
| Flutter | Fibrillation |
| This is due to the spreading of regular circus movement of impulse through the heart. | This is due to the spreading of irregular circus movement in many areas of the heart. |
| In this case, there is a coordinated contraction of heart. | There is an uncoordinated contraction of the heart. |
| Heart rates are within 200 to 300 beats/min. | Heart rates are more than 300 beats/min. |
Q.143 What are the clinical findings of ECG during MI?
- Elevation of ST segments in the leads overlying the area of infarct and
- Depression of ST-segment in the reciprocal leads.
Q.144 What do you mean by Stokes-Adams syndrome?
In the case of a complete heart block, there is some delay before ventricles start beating at their own rate. During this period the systemic blood pressure falls to a very low level and blood supply to the brain becomes inadequate. If ventricles do not beat for more than a few seconds it causes dizziness and fainting called Stokes-Adams syndrome.
Q.145 What are the ECG changes during the bundle branch block? What changes take place in heart sound production during its bundle branch block?
The ECG changes are as follows:
- Prolonged QRS complex (>0.12 sec)
- Abnormal ST segment and T wave.
- The second heart sound is splited.
Q.146 What types of ECG changes take place in atrial flutter and atrial fibrillation?
In case of atrial flutter following changes are seen:
- Shortening of all time intervals, e.g. PR, TP intervals
- Merger of T wave with P wave of the next cardiac cycle
- 2nd-degree type (2:1) of heart block.
In the case of atrial fibrillation following changes are seen:
- Absence of P wave.
- Appearance of fibrillation (f) waves
- Absence of T wave
- Irregular QRS complex.
Q.147 How does the ECG record change with time after MI?
- Within few hours after MI: Elevation of ST-segment.
- After some days of MI: Elevation of ST-segment along with inversion of T wave.
- After several weeks of MI: ST segments return to normal but an inversion of T wave is still present along with the appearance of Q wave.
- After months and years of MI: T wave becomes normal and the Q wave becomes deep.
Q.148 What do you mean by mean circulatory filling pressure and mean systemic filling pressure?
If the heartbeat is stopped, the flow of blood everywhere in the circulation ceases after a few seconds resulting in equal pressure within the whole circulation which is known as mean circulatory filling pressure. Whereas the mean systemic filling pressure is the pressure measured everywhere in the systemic circulation after blood flow is stopped by the clamping of the large blood vessels at the heart. Normally the amount of both are almost equal.
Q.149 Name different types of blood vessels in the vascular system with examples of each.
These are as follows:
- Distensible (Windkessel) vessels
—aorta, pulmonary artery, and their large branches. - Resistance vessels
—arterioles, meta-arterioles - Exchange vessels
—capillaries - Capacitance vessels
—venules and venous compartments - Shunt vessels
—AV anastomoses.
Q.150 What is windkessel effect?
The blood flow through the aorta is pulsatile in nature, i.e. it increases during systole and decreases during diastole of the heart. However, the blood flow through other blood vessels becomes uniform and continuous. This is because, during systole, the aorta (and to some extent the other larger blood vessels) dilates and later it recoils. This elastic recoiling of the aorta causes the continuous blood flow through other blood vessels. Thus, the pulsatile blood flow is converted into continuous flow. This recoiling effect is known as windkessel effect and the blood vessels exerting this effect are called the windkessel vessels.
Q.151 What are the components of the vasomotor system?
- Vasomotor center
- Vasoconstrictor fibers
- Vasodilator fibers.
Q.152 Where is the vasomotor center situated?
The vasomotor center is situated in the reticular formation of the medulla oblongata.
Q.153 What are the components of the vasomotor center?
- Vasoconstrictor or pressor area
- Vasodilator or depressor area.
- Sensory area.
Q.154 Name the vasoconstrictor and vasodilator nerve fibers.
Vasoconstrictor fibers are the sympathetic vasoconstrictor fibers.
Vasodilator fibers are:
- Parasympathetic fibers
- Sympathetic cholinergic fibers
- Antidromic nerve fibers.
Q.155 What is the mode of action of sympathetic adrenergic fibers on blood vessels?
Sympathetic adrenergic fibers cause constriction of blood vessels (vasoconstriction) by secreting noradrenaline.
Q.156 What is vasomotor tone?
Vasomotor tone is the continuous discharge of impulses from the vasoconstrictor center to arterioles through vasoconstrictor nerve fibers. Vasomotor tone maintains arterial blood pressure by producing constant partial constriction of blood vessels (peripheral resistance). The arterial blood pressure is directly proportional to the vasomotor tone.
Q.157 Blood flow to the different body organs can be so effectively regulated by only small changes in the caliber of the arteries. How is it possible?
As resistance to blood flow is inversely proportional to the 4th power of the radius (r) of arterioles, the small changes of the radius can cause greater changes of resistance to blood flow and thereby flow to the different body organs.
Q.158 What do you mean by critical closing pressure?
Extravascular tissues exert a small but definite pressure on vessels and when the intraluminal pressure falls below this extravascular pressure the vessel collapses. The pressure at which the flow ceases is called critical closing pressure.
Q.159 State the law of Laplace. What is its functional significance?
It states that the distending pressure (P) in a distensible hollow object is equal at equilibrium to the tension in the wall (T) divided by two principal radii of curvature of object (R1 and R2), i.e. P = T (1/R1+1/R2).
Significance:
(i) smaller the radius of the blood vessels lesser the tension in the wall necessary to balance the distending pressure.
This is why
(i) thin and delicate capillaries are less prone to rupture,
(ii) a dilated heart has to do more work than a normal heart.
Q.160 What is axon reflex?
In response to a firm stroke in the skin, the afferent impulses are relayed to the endings near cutaneous arterioles down the branches of the sensory nerve to result in cutaneous arteriolar dilatation. This neural pathway which does not involve CNS is known as axon reflex.
Q.161 What do you mean by cold blue skin and warm red skin?
Cold blue skin is the skin in which the arterioles are constricted and the capillaries are dilated whereas in warm red skin both arterioles and capillaries are dilated.
Q.162 What is the triple response?
A firm and strong stroke on the skin by a blunt object evokes a series of responses which are
- Red reaction
- Flare and
- Wheal.
These responses to the injury are collectively known as triple response.
Q.163 What is the physiological basis of red reaction, flare and wheal?
Red reaction: It is due to the dilatation of the precapillary sphincter due to the release of histamine and/or bradykinin like vasodilator substances.
Flare: It is due to dilatation of arterioles, terminal arterioles, and precapillary sphincter which causes an increase in blood flow and thereby irregular erythematous area surrounding the red line.
Wheal: It is due to increased capillary permeability and rise of capillary pressure which ultimately causes local diffuse swelling at and near the site.
Q.164 What is a white reaction?
When a pointed object is drawn lightly over the skin the stroke line becomes pale due to draining out of blood from the capillaries and small vein due to contraction of precapillary sphincters.
Q.165 What is the average total peripheral resistance of rest?
It is 1 PRU.
Q.166 On what factors the peripheral resistance does depend.
It depends on the elasticity of the vessel wall, diameter of arterioles (inversely), viscosity, and velocity of blood directly.
Q.167 Define Poiseuille’s law.
It states that resistances to blood flow in a blood vessel proportionately varies with the length of blood vessels and viscosity of blood and inversely with the 4th power of the radius of the lumen of vessels.
Q.168 What is circulation time? Give the value of total circulation time.
It is time taken by blood to flow from one site to any other specific site. Normal total circulation time is 12-16 sec.
Q.169 Coronary blood flow fluctuates with each phase of the cardiac cycle, explain.
During systole, the coronary blood flow is reduced because of compression of coronary vessels due to the contraction of cardiac muscle whereas during diastole as cardiac muscle relaxes, there is distention of coronary vessels to its original diameter and thus blood flow through it to the heart muscle is increased
Q.170 Why does the subendocardial portion of the left ventricle is more prone for MI?
It is for two reasons as follows:
- No blood flows to this portion during systole because of poor blood supply in this region and also compression of blood vessels during systole.
- Anaerobic respiration goes on in the inner layer which increases further under stress.
Q.171 What is the normal time taken for coronary circulation?
It is about 8 sec.
Q.172 What are the factors on which coronary blood flow depends?
These are mainly the lumen of coronary vessels, mean aortic pressure, and also by cardiac output, HR, body temperature, CO2 concentration in blood and cardiac sympathetic stimulation.
Q.173 What is the normal pulmonary blood flow rate?
It is about 3-5 lit/min.
Q.174 What is the normal blood flow rate in the liver?
It is about 1500 ml/min.
Q.175 What is the normal coronary blood flow?
It is about 225 ml/min.
Q.176 Give the normal value of cerebral blood flow.
It is approx. 750 ml/min.
Q.177 Define shock. Classify it.
Shock is a syndrome characterized by low cardiac output which is inadequate to maintain normal tissue perfusion.
It is of 4 types—hypovolemic, vasogenic, cardiogenic and obstructive shock.
Q.178 What do you mean by cold shock?
When the amount of fluid in the vascular system is inadequate to fill it, resulting in a decrease in circulatory blood volume it is known as hypovolemic or cold shock.
Q.179 What is warm shock?
When the diameter of capacitance vessels is increased by vasodilatation, there is a decrease of cardiac output in spite of normal blood volume. This type of shock is vasogenic shock and in this type of shock as skin becomes warm it is also called as warm shock
Q.180 What is congested shock?
The cardiogenic shock causes congestion of the lungs, viscera and that is why it is called as congested shock.
Q.181 What is Bezold-Jarish reflex?
The ventricular receptors are sensitive to chemicals or partial occlusion of the aorta or coronary artery which are responsible for profound bradycardia, hypotension, and apnea. This response is known as ‘Coronary chemoreflex’ or Bezold Jarish reflex which is clinically associated with Myocardial infarction or vasovagal syncope.
Q.182 What is sinus arrhythmia?
During inspiration, HR is increased and during expiration, HR is reduced. This phenomenon is called as sinus arrhythmia.
Q.183 What is bradycardia? Where can you see the physiological bradycardia?
A decrease of heart rate below 60 beats/min is known as bradycardia which is physiologically seen in the following conditions.
- Athletes
- Males
- Emotional stimuli like shock, grief, depression, etc.
- During expiration.
Q.184 What do you mean by laminar and turbulent flow? How does turbulence produce?
Laminar or streamline flow:
It is fixed layer-wise i.e. each layer of blood remains at the same distance from the wall blood vessels flowing through a long vessel and the velocity of blood is maximum in the core of the blood vessels and minimum in its periphery or surface. This type of steady rate of blood flow is known as laminar blood flow.
Turbulent blood flow:
When the blood flows crosswise in the vessels by forming whorls in the blood is called as eddy current. This type of blood flow is known as turbulent blood flow. It is produced by obstruction of vessels or when it takes a sharp U-turn.
Q.185 What are the signs and symptoms of shock?
Different signs and symptoms manifested during shock are as follows:
- Reduction in arterial blood pressure.
- Reflex tachycardia and reduced stroke volume.
- Decrease in pulse pressure and appearance of thready pulse.
- Reduction in velocity of blood flow producing stagnant hypoxia and cyanosis.
- Pale and cold skin due to reflex vasoconstriction.
- Decreased urinary output due to reduced renal blood flow and GFR.
- Fainting due to reduced blood flow to the brain tissue.
- Feeling of intense thirst if the patient is conscious.
- Rapid and shallow breathing.
- Metabolic acidosis due to excessive production of lactic acid by the myocardium.
- Death due to cerebral or cardiac failure.
Q.186 What are the symptoms of left ventricular failure?
These are:
- Difficulty in breathing on exertion.
- Dyspneic attack at night.
- Dyspnea in supine position.
Q.187 What are the signs and symptoms of right ventricular failure?
These are:
- Engorgement of right atrium
- Increased venous pressure
- Swelling of liver
- Peritoneal and pleural effusion
- Cyanosis and dyspnoea
- Edema.
Q.188 What are the common causes of left ventricular failure?
These are: essential hypertension, coronary insufficiency, myocardial fibrosis, and mitral valve incompetence.
Q.189 What are the salient features of left ventricular failure?
These are:
- Decrease in cardiac output with vasoconstriction of peripheral vessels
- Pulmonary edema, dyspnea, and anoxia (cardiac asthma).
Q.190 How do you differentiate left and right cardiac failure broadly on the basis of edema?
In left heart failure, pulmonary edema is seen whereas, in right heart failure, edema is systemic in nature.
Q.191 Enumerate some of the effects of severe hemorrhage.
These are decreased blood volume, state of shock, increased heart rate, decreased systolic BP, vasoconstriction, hemodilution, rapid and shallow breathing, blurred vision, fainting, etc.

Comments (0)