Q.1 What is the normal respiratory rate?
12 to 16 per minute.
Q.2 What are the types of respiration?
External respiration that involves the exchange of respiratory gases, i.e. oxygen and carbon dioxide between the alveoli of the lungs and blood
Internal respiration involves the exchange of respiratory gases between blood and tissues.
Q.3 Define respiratory unit.
Respiratory unit is the terminal portion of the respiratory tract where the exchange of gases occurs.
Q.4 Name the structures of the respiratory unit.
- Respiratory bronchiole
- Alveolar ducts
- Antrum
- Alveolar sacs
- Alveoli.
Q.5 List the non-respiratory functions of the respiratory tract.
- Olfaction
- Vocalization
- Prevention of dust particles
- Defense mechanism
- Maintenance of water balance
- Regulation of body temperature
- Regulation of acid-base balance
- Anticoagulant function
- Secretion of angiotensin-converting enzyme (ACE)
- Synthesis of hormonal substances.
Q.6 What is the role of the lungs in defense mechanism?
- Lung’s own defense: Secretion of immune factors – defensins and cathelicidins
- Leukocytes: Neutrophils and lymphocytes kill the bacteria and virus
- Macrophages: Engulf dust particles and pathogens, act as antigen-presenting cells; secrete interleukins, tumor necrosis factors, and chemokines
- Mast cell: Produces hypersensitivity reactions
- Natural killer cell: First line of defense against virus
- Dendritic cells: Function as antigen-presenting cells.
Q.7 What are the characteristic features of pulmonary circulation?
- The wall of pulmonary blood vessels is thin
- These blood vessels are more elastic
- Smooth muscle coat is not well developed in these blood vessels
- True arterioles have less smooth muscle fibers
- Pulmonary capillaries are larger than systemic capillaries.
what is intrapleural pressure?
Q.8 What is the normal pulmonary blood pressure?
Systolic pressure: 25 mm Hg
Diastolic pressure: 10 mm Hg
Mean arterial pressure: 15 mm Hg
Capillary pressure: 7 mm Hg.
Q.9 Enumerate the factors regulating pulmonary circulation.
- Cardiac output
- Pulmonary vascular resistance
- Nervous factors
- Chemical factors.
Q.10 Name the primary inspiratory and primary expiratory muscles with the nerve supply.
Primary inspiratory muscles:
- Diaphragm—innervated by phrenic nerve
- External intercostal muscles—innervated by intercostal nerves.
Primary expiratory muscles:
- Internal intercostal muscles—innervated by intercostal nerves.
Q.11 Name the accessory respiratory muscles.
The accessory inspiratory muscles are sternomastoid, scalene, anterior serrati, elevators of scapulae, and pectorals. The accessory expiratory muscles are abdominal muscles.
Q.12 What are the movements of the thoracic cage during inspiration?
Thoracic cage enlarges during inspiration and its size increases in all diameters. Increase in anteroposterior diameter is due to the elevation of the upper costal series and the upward and forward movement of the sternum. Increase in transverse diameter is due to the elevation of the lower costal series. The increase in vertical diameter is due to the descent of the diaphragm.
Q.13 What is pump handle movement? What is its significance?
During inspiration, the upper costal series (second to sixth pair of ribs) are elevated and the sternum moves upward and forward. This type of movement of ribs and sternum is called pump handle movement.
Significance: It increases the anteroposterior diameter of the thoracic cage during inspiration.
Q.14 What is bucket handle movement? What is its significance?
During inspiration, the central portions (arches) of the upper costal series (second to sixth pair of ribs) and lower costal series (seventh to tenth pair of ribs) swing outward and upward. This is called bucket handle movement. Significance: It increases the transverse diameter of the thoracic cage during inspiration.
Q.15. What is the significance of the contraction of the diaphragm during inspiration?
When the diaphragm contracts, it is flattened. This increases the vertical diameter of the thoracic cage during inspiration.
Q.16 What is Dalton's law?
It states that total pressure exerted by a mixture of gases is equal to the sum of the partial pressures of all the gases present within it.
Q.17 What is Henry's law?
It states that if the temperature is kept constant, the amount of gas dissolved in any solution is directly proportional to the partial pressure of that gas.
Q.18 Give the normal value of intrapulmonary or intra-alveolar pressure.
It is about 760 mm Hg.
Q.19 Why intra-alveolar pressure is equal to that of atmospheric pressure? How is it affected during inspiration and expiration?
It is equal to the atmospheric pressure as during quiet breathing, at the end of expiration, and at the end of inspiration, no air is going in and out of the lungs. During inspiration it decreases 3 mm Hg below its normal value, i.e. 757 mm Hg and during expiration, it increases 3 mm Hg above its normal value, i.e. 763 mm Hg.
Q.20 What is the Valsalva maneuver and Muller's maneuver?
Forced expiration against a closed glottis may produce positive intrapulmonary pressure of > 100 mm Hg above the atmospheric value. This voluntary action is known as the Valsalva maneuver. Forced inspiration against closed glottis can reduce the intrapulmonary pressure to < 80 mm Hg below the atmospheric value. This voluntary action to reduce the intrapulmonary pressure is known as Muller's maneuver.
Q.21 What is the collapsing tendency of the lungs?
The constant threat of compression of the lungs is called the collapsing tendency of lungs.
Q.22 What are the factors causing the collapsing tendency of lungs?
- Elastic property of lung tissues that induces the recoiling tendency of lungs
- Surface tension exerted by the alveolar fluid.
Q.23 What are the factors preventing the collapsing tendency of lungs?
- Intrapleural pressure that overcomes the elastic recoiling tendency of lungs
- Surfactant that overcomes surface tension.
Q.24 What is surfactant? Name the cells secreting surfactant.
Surfactant is the lipoprotein substance that reduces the surface tension induced by the fluid lining in the alveoli. It is secreted by type II alveolar epithelial cells of lungs and Clara cells situated in bronchioles.
Q.25 What is the function of surfactant?
Surfactant prevents the collapsing tendency of lungs by reducing the surface tension in the alveoli.
Q.26 What is respiratory distress syndrome or hyaline membrane disease?
It is the condition in infants with the collapse of the lungs due to the absence of surfactant. In adults, it is called adult respiratory distress syndrome (ARDS).
what is intrapleural pressure
Q.27 Define and give normal values of intrapleural or intrathoracic pressure.
The intrapleural or intrathoracic pressure is the pressure existing in the pleural cavity. It is always negative. During inspiration, it is – 6 mmHg and during expiration, it is – 2 mmHg.
Q.28 What is the cause of negative intrapleural pressure?
The intrapleural pressure is negative because of the constant pumping of fluid (secreted by the visceral layer of pleura) from the intrapleural space into lymphatic vessels.
Q.29 What is the significance of intrapleural pressure?
The intrapleural pressure prevents the collapsing tendency of lungs. It is also responsible for the respiratory pump that increases venous return.
Q.30 How is intrapleural pressure measured?
By using an intraesophageal balloon.
Q.31 Define and give normal values of intraalveolar or intrapulmonary pressure.
The intraalveolar or intrapulmonary pressure is the pressure existing in the alveoli of the lungs. During inspiration, it is – 4 mm Hg During expiration it is + 4 mm Hg
Q.32 What is the significance of intraalveolar pressure?
- It causes the flow of air into alveoli during inspiration and out of alveoli during expiration
- It helps in the exchange of gases between alveoli and blood.
Q.33 What is transpulmonary pressure?
Transpulmonary pressure is the difference between the intraalveolar pressure and intrapleural pressure.
Q.34 What is compliance?
The expansibility of the lungs and thorax is known as compliance. It is defined as a change in volume per unit change in pressure.
Q.35 Define compliance in relation to intraalveolar pressure and give normal value.
In relation to intraalveolar pressure, compliance is defined as the volume increase in lungs per unit increase in intraalveolar pressure. Compliance of lungs and thorax = 130 ml/ cm H2O. Compliance of lungs alone = 220 ml/cm H2O.
Q.36 Define compliance in relation to intrapleural pressure and give normal value.
In relation to intrapleural pressure, compliance is defined as the volume increase in lungs per unit decrease in the intrapleural pressure.
Compliance of lungs and thorax = 100 ml/ cm H2O. Compliance of lungs alone = 200 ml/cm H2O.
Q.37 Define work of breathing.
The work done by respiratory muscles during breathing to overcome the resistance in the thorax and respiratory tract is known as work of breathing.
Q.38 What are the types of resistance for which energy is utilized during work of breathing?
- Airway resistance – that is overcome by airway resistance work.
- Elastic resistance of the lungs and thorax – that is overcome by compliance work.
- Nonelastic viscous resistance – that is overcome by tissue resistance work.
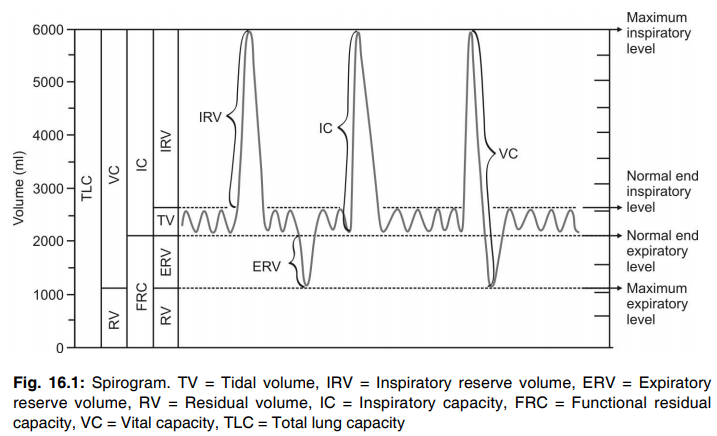
Q.39 Define and give normal values of lung volumes.
| Tidal volume: The volume of air breathed in and out of the lungs in a single normal quiet breathing. Normal value: 500 ml. |
| Inspiratory reserve volume: The additional amount of air that can be inspired forcefully beyond normal tidal volume. Normal value: 3,300 ml. |
| Expiratory reserve volume: The additional amount of air that can be expired forcefully after normal expiration. Normal value: 1,000 ml. |
| Residual volume: The amount of air remaining in the lungs even after forced expiration. Normal value: 1,200 ml. |
Q.40 What is lung capacity? Define and give normal values of lung capacities.
Two or more lung volumes together are called lung capacity.
Lung capacities:
| Inspiratory capacity: The maximum volume of air that can be inspired from the end-expiratory position. It includes tidal volume and inspiratory reserve volume. Normal value: 3,800 ml. |
| Vital capacity: The maximum volume of air that can be expelled out forcefully after a maximal (deep) inspiration. It includes inspiratory volume, tidal volume, and expiratory reserve volume. Normal value: 4,800 ml. |
| Functional residual capacity: The volume of air remaining in the lungs after normal expiration (after tidal expiration). It includes expiratory reserve volume and residual volume. Normal value: 2,200 ml. |
| Total lung capacity: The amount of air present in the lungs after a maximal (deep) inspiration. It includes all the four lung volumes i.e., inspiratory reserve volume, tidal volume, expiratory reserve volume, and residual volume. Normal value: 6,000 ml. |
Q.41 Why the 'Wheeze' sound is heard during expiration but not in the inspiration of an asthma patient?
During inspiration, the intrapleural and mediastinal negativity rises and as a result the bronchial diameter increases. Reverse occurs during expiration. Therefore resistance to airflow is normally low in inspiration and high in expiration. This is why in bronchial asthma inspiration may not be difficult but expiration becomes difficult. This explains why the "Wheeze" in bronchial asthma is heard during expiration but not in inspiration.
Q.42 What is the significance of residual volume?
- It helps in the exchange of gases in between breathing and during the expiration
- It maintains the contour of the lungs.
Q.43 What are the instruments used to measure lung volumes and lung capacities?
- Spirometer
- Respirometer.
Q.44 Name the lung volumes and capacities, which can not be measured by a spirometer.
- Residual volume
- Functional residual capacity
- Total lung capacity.
Q.45 How are residual volume and functional residual capacity measured?
- Helium dilution technique
- Nitrogen washout method.
Q.46 Define vital capacity. What is its importance?
It is the maximum volume of air that can be expired by forceful effort after a maximal inspiration. It provides useful information about the strength of respiratory muscles and also provides useful information about other aspects of pulmonary function through FEV1.
Q.47 In which posture VC is highest and why?
In standing posture, it is the highest as in standing position diaphragm descends down thereby increasing intrathoracic volume. This increases intra-alveolar volume during inspiration.
Q.48 In whom the vital capacity is more?
- Heavily built persons
- Athletes
- People playing musical wind instruments like bugle.
Q.49 Name the pathological conditions when vital capacity is reduced.
- Asthma
- Emphysema
- Weakness or paralysis of respiratory muscle
- Congestion of lungs
- Pneumonia
- Pneumothorax
- Hemothorax
- Pyothorax
- Hydrothorax
- Pulmonary edema
- Pulmonary tuberculosis.
Q.50 Why does VC decrease during pregnancy?
During pregnancy, the diaphragm is pushed up by the growing fetus resulting in a decrease of intrathoracic volume and thereby decrease of capacity to inspire air and thereby VC is decreased.
Q.51 What is respiratory minute volume (RMV)? Give its normal value.
Respiratory minute volume is the amount of air that is breathed in and out of the lungs during each minute. It is the product of tidal volume and respiratory rate.
Normal value: 6,000 ml (500 ml × 12).
Q.52 What is maximum breathing capacity (MBC) or maximum ventilation volume (MVV)? What is its normal value?
It is the maximum amount of air that can be breathed in and out of the lungs by forceful respiration (hyperventilation).
Normal value: In healthy – 150 to 170 liters/minute adult male
In females – 80 to 100 liters/minute.
Q.53 What is forced expiratory volume (FEV) or timed vital capacity?
The amount of air that can be expired forcefully (after deep inspiration) in a given unit of time is called forced expiratory volume (FEV) or timed vital capacity
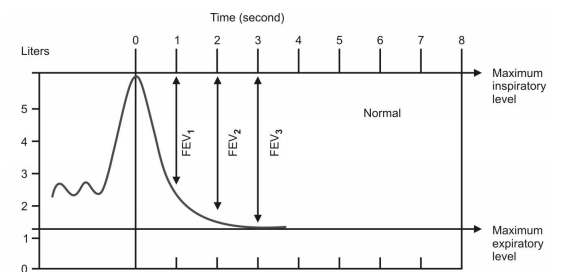
Q.54 What is FEV1?
The amount of air that can be expired forcefully after deep inspiration in the first second is called FEV1 (1 stands for ‘first second’).
Q.55 Give the normal values of FEV1, FEV2, and FEV3.
FEV1= 83%;
FEV2 = 94%;
FEV3 = 97%.
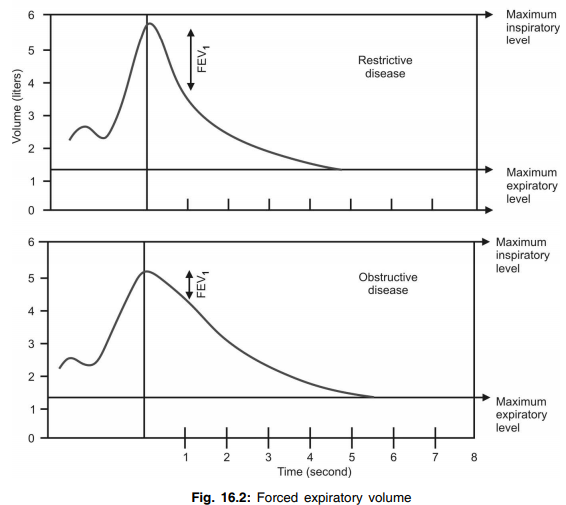
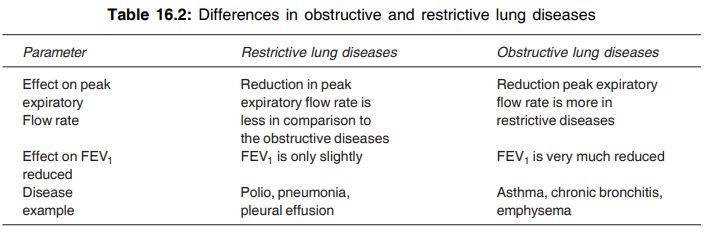
Q.56 What is the significance of determining FEV?
Vital capacity may be almost normal in some of the respiratory diseases. However, the determination of FEV has greater diagnostic value, as it is decreased significantly in some respiratory disorders, particularly in obstructive diseases like asthma and emphysema.
Q.57 Define and give normal value of peak expiratory flow rate (PEFR).
The maximum rate at which air can be expired after deep inspiration is known as peak expiratory flow rate (PEFR). Normal value: About 400 liters/minute.
Q.58 How is PEFR measured?
By using Wright’s peak flow meter or mini peak flow meter.
Q.59 What is the significance of measuring PEFR?
Measurement of PEFR is useful in assessing the respiratory diseases, especially to differentiate the obstructive and restrictive diseases. It is about 200 liters/ minute in restrictive diseases and it is only 100 liters/ minute in obstructive diseases. It is valuable when measured serially to establish the pattern of airway obstructive disease and to monitor its responses in treatments, especially asthma.
Q.60 What is pulmonary ventilation? Give its normal value.
Pulmonary ventilation is the cyclic process by which fresh air enters the lungs and an equal volume of air is expired. It is defined as the amount of air breathed in and out of the lungs in one minute. It is the product of tidal volume and respiratory rate. It is otherwise known as respiratory minute volume.
Normal value: 6,000 ml/minute.
Q.61 What is alveolar ventilation? Give its normal value.
Alveolar ventilation is the amount of air utilized for gaseous exchange every minute.
Alveolar = (Tidal volume – Dead space ventilation volume) × Respiratory rate.
Normal value: 4,200 ml.
Q.62 What is dead space? Give normal value.
The part of the respiratory tract where the gaseous exchange does not occur is known as dead space. The air present in the dead space is called dead space air.
Normal value: 150 ml.
Q.63 What are the types of dead space?
Anatomical dead space, which includes the volume of the respiratory tract from nose up to terminal bronchiole.
Physiological dead space which includes anatomical dead space and two additional volumes:
– The volume of air in those alveoli, which are not functioning
– The amount of air in those alveoli, which do not receive adequate blood flow.
Q.64 Why the physiological dead space is equal to anatomical dead space in normal conditions?
Because all the alveoli of both lungs are functioning and all the alveoli receive adequate blood supply in normal conditions.
Q.65 How is dead space measured?
By single breath nitrogen washout method.
Q.66 What is the ventilation-perfusion ratio? Give its normal value.
It is the ratio of alveolar ventilation (VA) and the amount of blood (Q) flowing through the lungs.
Ventilation-perfusion ratio = VA/Q = 4,200/5,000.
Normal value: About 0.84.
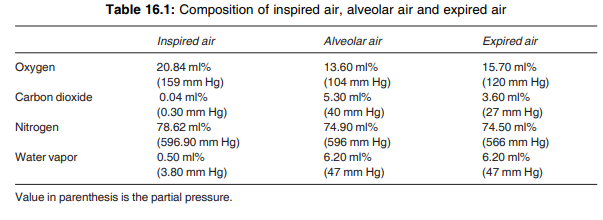
Q.67 What are the differences between inspired air and alveolar air?
- Oxygen content is more in inspired air than in alveolar air
- Carbon dioxide is less in inspired air than in alveolar air
- Inspired air is dry whereas alveolar air is humid.
Q.68 What is the composition of inspired air (atmospheric air), alveolar air, and expired air?
The composition of inspired air (atmospheric air), alveolar air, and expired air is tabulated in Table 16.1.
Q.69 How is alveolar air collected?
By using the Haldane-Priestly tube.
Q.70 How is inspired air collected?
Since the inspired air is the atmospheric air, it can be drawn from the atmosphere through the syringe.
Q.71 How is expired air collected?
By using a Douglas bag.
Q.72 What is the respiratory membrane?
The alveolar membrane and the capillary membrane in the lungs through which diffusion of gases takes place are together called the respiratory membrane.
Q.73 What are the layers of the respiratory membrane?
From within outside:
- Surfactant
- Fluid lining the alveoli
- Alveolar epithelial cells
- Interstitial layer
- Basement membrane
- Capillary endothelial cells
Q.74 What is diffusing capacity?
Diffusing capacity is the volume of gas that diffuses through the respiratory membrane each minute for a pressure gradient of 1 mmHg.
Q.75 Mention the diffusing capacity for oxygen and carbon dioxide.
Diffusing capacity for oxygen is 21 ml/ minute/mmHg and for carbon dioxide it is 400 ml/minute/mmHg. Thus, the diffusing capacity for carbon dioxide is about 20 times more than that of oxygen.
Q.76 What are the factors affecting the diffusing capacity?
Diffusing capacity is directly proportional to
- Pressure gradient of gases between alveoli and blood in pulmonary capillary
- Solubility of gas in fluid medium
- Total surface areas of the respiratory membrane.
Diffusing capacity is inversely proportional to:
- Molecular weight of the gas
- Thickness of respiratory membrane.
Q.77 State Hook's law in relation to lung.
Length is directly proportional to force within a physiological limit.
Q.78 Define lung compliance. What is the 'hysteresis' curve of lung compliance?
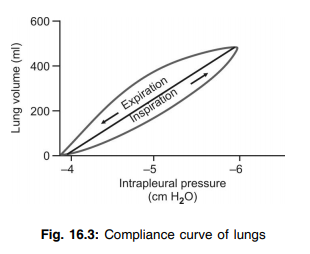
The change of lung volume per unit change in airway pressure is called as lung compliance. In the compliance curve, at identical intrapleural pressure, the volume of the lung is less in the inspiratory phase than in the expiratory phase. This different pressure-volume relationship curve during inspiration and expiration is known as 'hysteresis 'curve.
Q.79 What is specific compliance? What is its advantage to use?
Compliance when expressed as a function of FRC is known as specific compliance.
In individuals with one lung only, lung compliance is approximately half of the normal even if the normal distensibility of normal lung is present. Similarly in children compliance is lower than normal though the distensibility of lung remains normal. This fallacy is removed with specific compliance since FRC is proportionately reduced and specific compliance remains essentially constant.
Q.80 What is the oxygen content and partial pressure of oxygen (PO2) in the blood?
Arterial blood:
Oxygen content = 19 ml%
PO2 = 95 mm Hg
Venous blood:
Oxygen content = 14 ml%
PO2 = 40 mm Hg.
Q.81 What is the carbon dioxide content and partial pressure of carbon dioxide (PCO2) in the blood?
Arterial blood :
Carbon dioxide content = 48 ml%
PCO2 = 40 mmHg
Venous blood :
Carbon dioxide content = 52 ml%
PCO2 = 45 mmHg.
Q.82 What is the coefficient of utilization?
The percent of blood that gives up its O2 as it passes through the tissue capillaries is called as the coefficient of utilization. At rest, it is about 25 percent and during heavy exercise, it increases up to 75 percent.
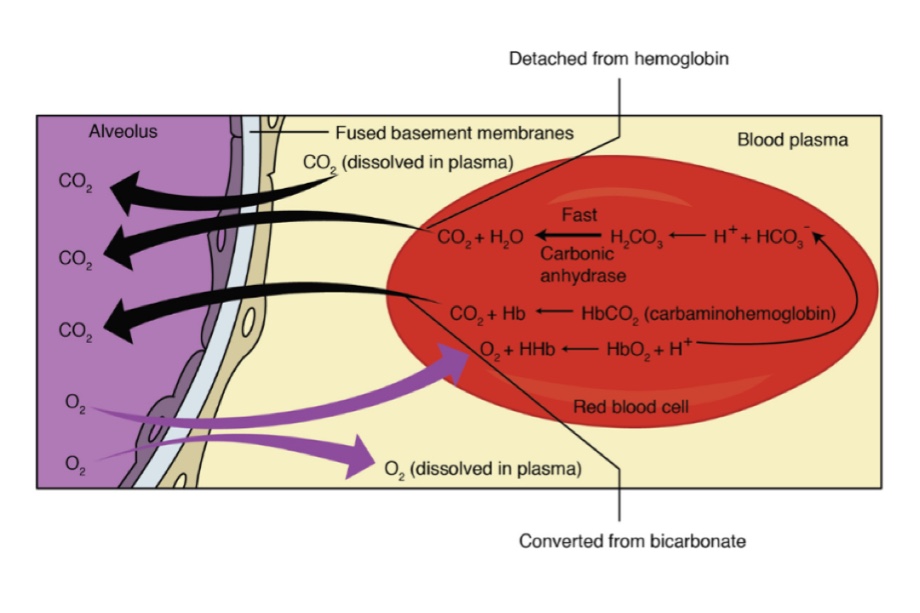
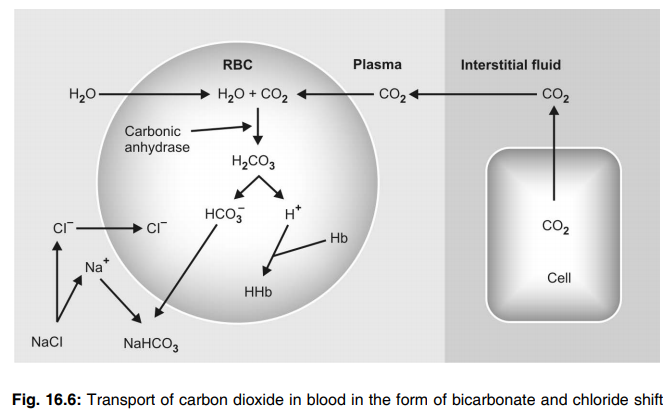
Q.83 In which form CO2 transported in blood?
Mainly in 3 forms:
- In dissolved form in plasma and RBC - 0.3 ml%
- As bicarbonate form of Na+ and K+ - 3 ml%
- As carbamino compound form - 0.7 ml%
Q.84 What is the CO2 content and partial pressure of CO2 in arterial and venous blood?
| CO2 content | PCO2 |
| Arterial blood-48 ml% | 40 mm Hg |
| Venous blood-52 ml% | 46 mm Hg |
Q.85 In which form the venous CO2 is mostly found?
In bicarbonate form.
Q.86 What are the effects of CO2 addition to blood?
It causes an increase in plasma bicarbonate ion, a decrease in plasma chlorides, and an increase in RBC chlorides.
Q.87 What do you mean by maximum venous point and arterial point?
In deoxygenated blood with maximum PCO2, 60-67 mm Hg, CO2 content is 65 ml% called as the maximum venous point.
In oxygenated blood at PCO2 40 mm Hg, CO2 content is 48 ml% called as the arterial point.
Q.88 What do you mean by physiological CO2 dissociation curve?
If we join maximum ‘venous point’ and ‘arterial point’ which corresponds to extreme CO2 level in the body respectively, it will roughly reflect changes between PCO2 and CO2 content in the blood and called the physiological CO2 dissociation as represented by curve.
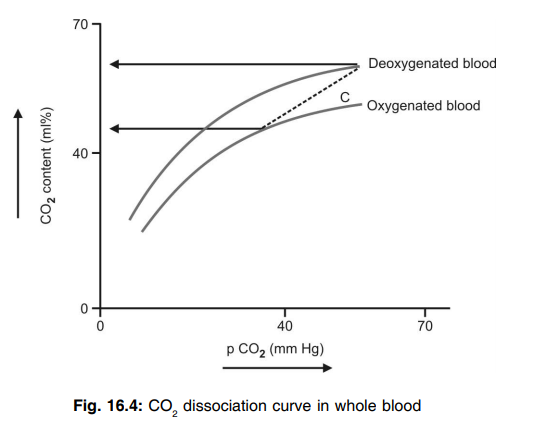
Q.89 What are the factors affecting the CO2 dissociation curve?
These are:
- Increase in body temperature shifts the curve to the left, i.e. at increased body temperature larger amount of CO2 can be taken by the blood at a given PCO2.
- Decrease in PO2 shifts the curve to the left and thereby helps in the loading of CO2 in blood.
Q.90 What is the respiratory exchange ratio? Give its normal value.
It is the ratio between the amount of oxygen consumed (uptake) and the amount of carbon dioxide given out by the tissues. It is 1.00 if only carbohydrate is utilized, 0.70 if only fat is utilized and 0.8 if only protein is utilized.
Q.91 How is oxygen transported by blood?
- As physical solution
- In combination with hemoglobin.
Q.92. What is the oxygen-carrying capacity of hemoglobin and blood?
The oxygen-carrying capacity of hemoglobin is 1.34 ml/g of hemoglobin. The oxygen-carrying capacity of blood is 19 ml/100 ml of blood when the hemoglobin content in blood is 15 g%. The oxygen-carrying capacity of blood is only 19 ml% because the hemoglobin in the blood is saturated with oxygen only for about 95%.
Q.93 What is the oxygen hemoglobin dissociation curve? What is its normal shape?
It is the curve that demonstrates the relationship between the partial pressure of oxygen and the percentage saturation of hemoglobin with oxygen. Normally, it is ‘S’ shaped or sigmoid shaped
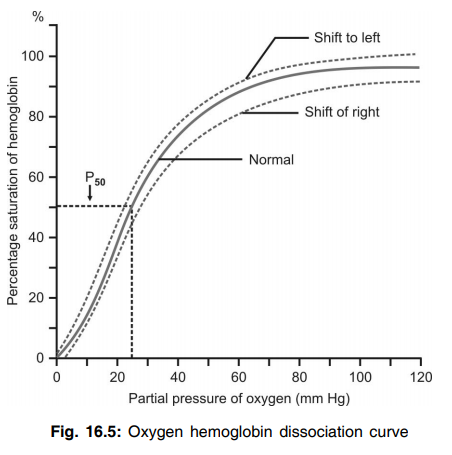
Q.94. Why this curve is sigmoid?
A Hb molecule contains 4 atoms of Fe++ each of which combines with O2 in varied affinity. The combination of 1st heme in the hemoglobin molecule with O2 increases the affinity of the 2nd heme for O2 and oxygenation of 2nd heme increases the affinity of the 3rd and so on. This shifting of affinity of Hb for O2 produces a sigmoid shape.
Q.95. What is the significance of the sigmoid shape of the O2 dissociation curve?
• O2 dissociation curve has the plateau above 60 mm Hg. This flat upper part indicates that even if the PO2 increases from 60 mm Hg to 300 mm Hg, the O2 content of the blood will not vary significantly. Similarly, the effect of O2 lack on the body will not be manifested until the PO2 goes down below 60 mm Hg.
• The steep slope of the curve indicates that the slight decrease of PO2 will cause a greater release of O2 from hemoglobin.
Q.96 What is the O2 content in arterial and venous blood?
Arterial blood-19 ml%;
venous blood - 14 ml%.
Q.97 What is the partial pressure of O2 in arterial and venous blood?
Arterial blood - 100 mm Hg;
Venous blood40 mm Hg.
Q.98 In which form O2 is carried from the lungs to tissues and in what amount?
- In dissolved form in plasma and RBC— 0.3 ml %
- In oxyhemoglobin form—18.7 ml %
Q.99 What do you mean by O2 carrying capacity of blood?
It is the O2 carrying capacity of the total hemoglobin of blood.
If the Hb content of a person is 16 gm% then his O2 carrying capacity will be 16 × 1.34 ml (each gram Hb carry 1.34 ml O2), i.e. 21 ml per deciliter of blood.
Q.100 What is the difference between O2 content and O2 capacity?
The O2 content refers to the amount of O2 actually present in a given sample of blood whereas O2 capacity refers to the total amount of O2 that can be carried by blood when the hemoglobin is fully saturated with O2.
Q.101 What is the indication of the shift to the right of the oxygen dissociation curve? Name some factors causing it.
Shift to the right of the oxygen dissociation curve indicates the dissociation or release of oxygen from hemoglobin.
It is caused by:
- Decrease in partial pressure of oxygen in blood
- Increase in partial pressure of carbon dioxide
- Increase in hydrogen ion concentration and decrease in pH (acidity)
- Increase in body temperature
- Excess of 2, 3 DPG (2,3, diphosphoglycerate).
Q.102 What is the indication of the shift to the left in the O2 dissociation curve? When does it occur?
Shift to the left of the oxygen dissociation curve indicates the acceptance (association or retention) of more amount of oxygen by hemoglobin.
It occurs:
- In fetal blood since fetal blood has more affinity for O2 than the adult blood
- When hydrogen ion concentration in the blood decreases causing an increase in pH (alkalinity).
Q.103 What is P50?
The partial pressure of oxygen at which the hemoglobin saturation is 50% is called P50. It is 25 mm Hg.
Q.104 What is Bohr’s effect?
The presence of carbon dioxide decreases the affinity of hemoglobin for oxygen and enhances the further release of oxygen to the tissues and the oxygen dissociation curve is shifted to the right. This is Bohr’s effect.
Q.105 How is carbon dioxide transported in the blood?
- As physical solution
- As carbonic acid
- As bicarbonate
- As carbamino compounds.
Q.106 Name the method by which the maximum amount of carbon dioxide is transported in the blood.
As bicarbonate (about 63%).
Q.107 What is chloride shift?
The negatively charged bicarbonate ions formed in the red blood cells diffuse out into the plasma. To maintain the electrolyte equilibrium, the negatively charged chloride ions move into the cells from plasma. This is known as the chloride shift.
Q.108 What is reverse chloride shift?
When the blood reaches the alveoli of the lungs, the bicarbonate ions diffuse into the red blood cells from plasma. To maintain electrolyte equilibrium, chloride ions move out of the cells into the plasma. This is known as reverse chloride shift.
Q.109 What is the carbon dioxide dissociation curve?
The curve that demonstrates the relationship between the partial pressure of carbon dioxide and the amount of carbon dioxide combined with blood is called the carbon dioxide dissociation curve.
Q.110 What is Haldane’s effect? What is its cause?
Excess of oxygen content in the blood displaces carbon dioxide from hemoglobin and shifts the carbon dioxide dissociation curve to the right. This is called Haldane’s effect. This is because, when more amount of oxygen combines, the hemoglobin becomes acidic. The highly acidic hemoglobin causes the displacement of carbon dioxide from hemoglobin.
Q.111 Name the mechanisms involved in the regulation of respiration.
- Nervous mechanism
- Chemical mechanism.
Q.112 What are the respiratory centers?
- Two medullary centers situated in medulla oblongata:
– Inspiratory center or dorsal group of neurons
– Expiratory center or ventral group of neurons. - Two pontine centers situated in pons:
– Pneumotaxic center
– Apneustic center.
Q.113 Mention the functions of each respiratory center.
Inspiratory center is concerned with inspiration. Expiratory center is concerned with expiration. Expiratory center is inactive during quiet breathing and becomes active during forced breathing or when the inspiratory center is inhibited. Apneustic center increases inspiration by activating the inspiratory center. Pneumotaxic center decreases inspiration by inhibiting the apneustic center. By inhibiting the apneustic center, it reduces the duration of inspiration and thereby increases the rate of respiration.
Q.114 What is inspiratory ramp?
Normally, the discharge of impulses from the inspiratory center is not uniform. To start with, the amplitude of action potential (impulse) is low because of the activation of only a few neurons. Later, when more and more neurons are activated, the amplitude increases gradually in a ramp fashion. The impulses are produced for 2 seconds during which inspiration occurs. This type of firing from the inspiratory center is called the inspiratory ramp.
Q.115 What is the significance of inspiratory ramp signals?
Significance of inspiratory ramp signals is that there is a slow and steady inspiration so that, the filling of lungs with air is also steady.
Q.116 What are the higher centers which alter the respiration by acting on the respiratory centers?
Anterior cingulated gyrus, genu of corpus callosum, olfactory tubercle, and posterior orbital gyrus of the cerebral cortex inhibit respiration. Motor area and Sylvian area of the cerebral cortex facilitate breathing.
Q.117 What is apneusis? How it can be resulted?
It is the arrest of respiration in the inspiratory phase. It can be experimentally resulted by transection in mid pons along with sectioning of vagus nerves.
Q.118 What are the various types of receptors in the lungs which alter the respiration?
- Stretch receptors present in the wall of bronchi and bronchioles of the lungs
- ‘J’ receptors or juxta capillary receptors situated in the wall of alveoli near the capillaries
- Irritant receptors present in the wall of bronchi and bronchioles.
Q.119 What is the function of stretch receptors present in the lungs?
Stretch receptors present in the lungs prevent overstretching of lungs by producing the Hering-Breuer reflex.
Q.120 What is the Hering-Breuer reflex? What is its significance?
Stretching of lungs during inspiration stimulates the stretch receptors in the lungs. The stretch receptors in turn send inhibitory impulses to the inspiratory center. So, inspiration stops and expiration starts. This is called the Hering-Breuer reflex. This reflex is a protective reflex because it restricts inspiration and prevents over-stretching of the lungs.
Q.121 What is the function of ‘J’ receptors?
Role of ‘J’ receptors in physiological conditions is not known clearly. However, these receptors are responsible for hyperventilation in patients affected by pulmonary congestion and left heart failure.
Q.122 What is the function of irritant receptors?
When harmful chemical agents like ammonia and sulfur dioxide enter the lungs, the irritant receptors are stimulated. The stimulation of irritant receptors results in reflex hyperventilation and bronchospasm so that further entry of harmful agents into the lungs is prevented.
Q.123 What is the effect of stimulation of baroreceptors on respiration?
When arterial blood pressure increases, the baroreceptors are activated and send inhibitory impulses to respiratory centers. So, the respiration is inhibited.
Q.124 What is the effect of stimulation of proprioceptors on respiration?
During exercise, the proprioceptors situated in muscles, tendons, and joints are stimulated and send impulses to the cerebral cortex. The cerebral cortex, in turn, activates the respiratory centers causing hyperventilation.
Q.125 What is the effect of stimulation of cold receptors (thermoreceptors) on respiration?
When the body is exposed to cold, the cold receptors are activated and send impulses to the cerebral cortex. Cerebral cortex, in turn, activates the respiratory centers causing hyperventilation.
Q.126 What is the effect of stimulation of pain receptors on respiration?
Whenever pain receptors are stimulated, the impulses from them are sent to the cerebral cortex via somatic afferent fibers. Cerebral cortex, in turn, activates the respiratory centers causing hyperventilation.
Q.127 What are chemoreceptors?
Chemoreceptors are the receptors, which give response to change in chemical constituents of blood such as O2, CO2, and H+.
Q.128 Classify chemoreceptors.
Depending upon the situation, the chemoreceptors are classified into two types:
- Central chemoreceptors situated in medulla oblongata near the inspiratory center and having close contact with blood and cerebrospinal fluid
- Peripheral chemoreceptors present in the carotid body and aortic body.
Q.129 Explain the function of central chemoreceptors briefly.
The activation of central chemoreceptors causes stimulation of the inspiratory center resulting in increased rate and force of respiration. The main stimulant for central chemoreceptors is the increased hydrogen ion concentration. However, if the hydrogen ion concentration increases in the blood, it cannot stimulate the central chemoreceptors because the hydrogen ions cannot cross the blood-brain barrier. But, if the carbon dioxide increases in the blood, it can cross the blood-brain barrier and enter the interstitial fluid of the brain or the cerebrospinal fluid. There, it combines with water forming carbonic acid that immediately dissociates into hydrogen ion and bicarbonate ion. Now, the hydrogen ions stimulate the central chemoreceptors causing an increase in rate and force of respiration.
Q.130 Explain the function of peripheral chemoreceptors.
The main stimulant for peripheral chemoreceptors is a reduction in partial pressure of oxygen (hypoxia). When the partial pressure of oxygen decreases, the peripheral chemoreceptors are stimulated and send stimulatory impulses to the inspiratory center. This causes an increase in the rate and force of respiration.
Q.131 What is pulmonary chemoreflex?
Injection of veratridine or nicotine like alkaloid substances into pulmonary capillaries stimulate chemoreceptors present in pulmonary vessels producing bradycardia, hypotension, and apnea followed by tachycardia. This response is called pulmonary chemoreflex.
Q.132 What do you mean by CO2 narcosis?
The accumulation of CO2 in the body depresses the CNS, including respiratory centers, and also produces headache, confusion, dizziness, apnea, and eventually coma. This ill effect of excess CO2 in the body is referred as CO2 narcosis.
Q.133 What are the types of respiratory diseases?
- Obstructive diseases like asthma and emphysema
- Restrictive diseases like pneumothorax and pneumonia.
Q.134 What is the difference between obstructive and restrictive diseases of the lungs?
Q.135 Define the following.
Eupnea: The normal respiration
Tachypnea: Increase in the rate of respiration
Bradypnea: Reduction in the rate of respiration
Polypnea: Rapid shallow breathing resembling panting in dogs; the rate of respiration is increased significantly but the force is not increased significantly.
Hyperpnea: Highly significant increase in pulmonary ventilation due to an increase in rate and force of respiration with more increase in rate.
Q.136 Define apnea. Name the conditions when apnea occurs.
Apnea is defined as a temporary cessation of breathing. It occurs:
- By voluntary effort – voluntary apnea or breath-holding
- After hyperventilation
- During the pharyngeal stage of deglutition – deglutition apnea
- During vagal stimulation – vagal apnea
- After adrenaline injection – adrenaline apnea.
Q.137 What is apnea time or breath-holding time?
The time during which a person can voluntarily stop breathing is known as apnea time or breath-holding time. It is about 40 to 60 seconds in a normal person.
Q.138 What is the breaking point? What is its cause?
At the end of voluntary apnea, the person is forced to breathe. The time when the person is forced to breathe is called breaking point. It is due to the accumulation of CO2.
Q.139 What is hyperventilation? When does it occur?
The increased pulmonary ventilation is known as hyperventilation. During this, both rate and force of respiration are increased.
Hyperventilation occurs in conditions like exercise when the partial pressure of carbon dioxide increases. It can also be produced voluntarily – voluntary hyperventilation.
Q.140 What are the effects of hyperventilation?
Carbon dioxide is washed out during hyperventilation leading to a reduction in the partial pressure of carbon dioxide in the blood. This causes suppression of respiratory centers resulting in apnea. Apnea is followed by Cheyne-Stokes breathing. After a period of Cheyne-Stokes breathing, normal respiration is restored.
Q.141 What is hypoventilation? When does it occur?
The decreased pulmonary ventilation due to reduction in rate and force of respiration is called hypoventilation. It occurs in the following conditions:
- During the suppression of respiratory centers.
- After the administration of some drugs.
- Due to partial paralysis of respiratory muscles.
Q.142 What are the effects of hypoventilation?
Hypoventilation causes hypoxia and hypercapnea. So, there is an increase in the rate and force of respiration leading to dyspnea. Severe hypoventilation leads to lethargy, coma, and death.
Q.143 Define hypoxia.
Hypoxia is defined as reduced availability of oxygen to the tissues of the body
Q.144 Why the term hypoxia is preferred than anoxia?
Anoxia means the absence of oxygen. Since there is no possibility for the total absence of oxygen in living conditions, the term hypoxia is preferred.
Q.145 Classify hypoxia.
- Hypoxic hypoxia
- Anemic hypoxia
- Stagnant hypoxia
- Histotoxic hypoxia
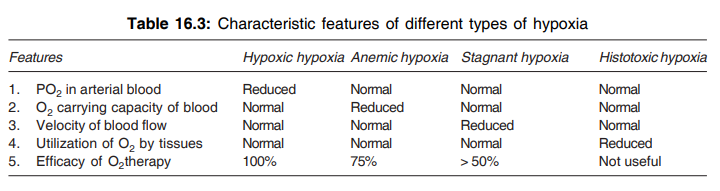
Q.146 Explain hypoxic hypoxia briefly. Name some important causes for it.
Hypoxic hypoxia or arterial hypoxia means the decreased oxygen content in the blood and it is characterized by reduced partial pressure of oxygen. Oxygen carrying capacity of blood, rate of blood flow, and utilization of oxygen are normal.
It is caused by:
- Low oxygen tension in inspired air (in atmosphere)
- Respiratory disorders
- Cardiac disorder.
Q.147 Explain anemic hypoxia briefly. Name some important causes for it.
The inability of the blood to carry enough amount of oxygen is known as anemic hypoxia. It is characterized by a reduced oxygen-carrying capacity of blood. Partial pressure of oxygen, rate of blood flow, and utilization of oxygen are normal.
Any condition that leads to anemia will cause anemic hypoxia such as:
– Decreased red blood cell count
– Decreased hemoglobin content
– Presence of altered hemoglobin
– Combination of hemoglobin with gases other than oxygen and carbon dioxide (like carbon monoxide).
Q.148 Explain stagnant hypoxia briefly. Name some important causes for it.
Hypoxia due to decreased velocity of blood flow is known as stagnant hypoxia. It is characterized by a reduced rate of blood flow. Partial pressure of oxygen, the oxygen-carrying capacity of blood, and utilization of oxygen are normal.
It is caused by:
- Congestive cardiac failure
- Hemorrhage
- Surgical shock
- Vasospasm
- Thrombosis
- Embolism.
Q.149 Explain histotoxic hypoxia briefly. Name some important causes for it.
The inability of tissue to utilize oxygen is called histotoxic hypoxia. It is characterized by reduced utilization of oxygen. The partial pressure of oxygen, the oxygen-carrying capacity of blood, and the rate of blood flow are normal. It is caused by the destruction of cellular oxidative enzymes and complete paralysis of the cytochrome oxidase system due to cyanide or sulfate poisoning.
Q.150 What do you mean by O2 poisoning.
Inhalation of O2 in high O2 pressure that occurs when O2 is breathed at a very high alveolar oxygen pressure like in Caisson may result in seizures followed by coma in most people. The other symptoms include nausea, muscle twitching, dizziness, disturbances of vision, irritability, etc. This phenomenon is called as O2 poisoning.
Q.151 What are the effects of severe acute hypoxia?
Severe acute hypoxia causes unconsciousness. If it is not treated immediately brain death occurs.
Q.152 What are the effects of chronic hypoxia?
- Red blood cell count increases due to the release of erythropoietin from kidney
- Initially, the rate and force of contraction of the heart are increased. Later, the rate and force of contraction of the heart are decreased. There is a reduction in cardiac output and blood pressure also
- Initially, the rate of respiratory rate is increased. Then, respiration becomes shallow and periodic. Finally, the rate and force of respiration are decreased
- Loss of appetite, nausea, vomiting, and thirst occur.
- Urine becomes alkaline
- In mild hypoxia, symptoms of alcoholic intoxication like depression, apathy, and loss of self-control occur
- The subject starts shouting, singing, and crying. There is loss of orientation, discriminative ability, power of judgment, and memory.
Q.153 How is hypoxia treated?
Hypoxia is treated by oxygen therapy.
Q.154 What is the efficacy of oxygen therapy in different types of hypoxia?
Oxygen therapy is not equally effective in all types of hypoxia.
Hypoxic hypoxia: Oxygen therapy is 100% useful
Anemic hypoxia: Oxygen therapy is moderately useful, i.e. about 70%
Stagnant hypoxia: Oxygen therapy is less than 50% useful
Histotoxic hypoxia: Oxygen therapy is of no use at all.
Q.155 What is hypercapnea? When does it occur?
Increased carbon dioxide content in the blood is known as hypercapnea. It occurs in conditions leading to asphyxia and breathing air containing more amount of carbon dioxide.
Q.156 What are the effects of hypercapnea?
- Respiration: Respiratory centers are stimulated leading to dyspnea
- Blood: pH of blood is reduced
- Cardiovascular system: Heart rate and blood pressure are increased. There is flushing of the skin due to peripheral vasodilatation
- Central nervous system: Headache, depression, laziness, rigidity, fine tremors, generalized convulsions, giddiness, and loss of consciousness occur.
Q.157 What is hypocapnea? When does it occur?
Decreased carbon dioxide content in the blood is known as hypocapnea. It occurs in conditions associated with hypoventilation and prolonged hyperventilation.
Q.158 What are the effects of hypocapnea?
- Respiration: Respiratory centers are depressed. Respiratory alkalosis occurs
- Blood: pH of blood is increased
- Central nervous system: Dizziness, mental confusion, muscular twitching, and loss of consciousness occur.
Q.159 What is asphyxia? When does it occur?
Asphyxia is the condition characterized by a combination of hypoxia and hypercapnea due to obstruction of the air passage. It occurs in conditions like strangulation and drowning.
Q.160 What are the stages of asphyxia?
- Stage of hyperpnea
- Stage of convulsions
- Stage of collapse.
Q.161 What is dyspnea or air hunger?
The difficulty in breathing is called dyspnea or air hunger. It is defined as the consciousness of the necessity for increased respiratory effort.
Q.162 What is dyspnea point?
Dyspnea point is the increased level of ventilation (increased rate and force of respiration) at which the difficulty in breathing becomes severe.
Q.163 Name the physiological and pathological conditions when dyspnea occurs.
Physiological condition:
- Severe muscular exercise.
Pathological conditions:
- Respiratory disorders like hindrance to respiratory movements and obstruction of the respiratory tract
- Cardiac disorders like left ventricular failure and mitral stenosis
- Metabolic disorders like diabetic acidosis, uremia, and increased hydrogen ion concentration.
Q.164 What is the dyspneic index? What is the level of dyspneic index at which dyspnea occurs?
The Dyspneic index is the index between breathing reserve and maximum breathing capacity. Breathing reserve is the difference between maximum breathing capacity (MBC) and respiratory minute volume (RMV).
Dyspneic index MBC – RMV = × 100 MBC Dyspnea occurs when the dyspneic index is reduced below 60%.
Q.165 Define periodic breathing. Mention the types of periodic breathing.
The abnormal or uneven respiratory rhythm is called periodic breathing.
It is of two types:
- Cheyne–Stokes breathing
- Biot’s breathing.
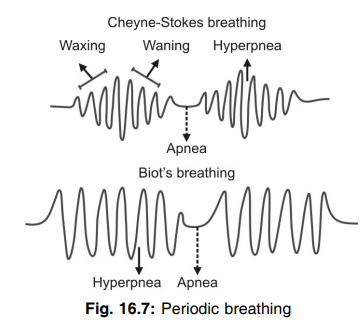
Q.166 What is Cheyne–Stokes breathing?
Cheyne–Stokes breathing is a type of periodic breathing characterized by two alternate periods namely, the hyperpneic period and apneic period. During the hyperpneic period, at the beginning, breathing is shallow. The force of respiration increases gradually and reaches the maximum. Then, it decreases gradually and reaches the minimum. This is called waxing and waning. When the force of respiration reaches the minimum apnea occurs. Then hyperpnea occurs and the cycle is repeated.
Q.167 What are the causes for waxing and waning during Cheyne-Stokes breathing?
During forced breathing, excess of carbon dioxide is washed out of the blood. When the carbon dioxide tension becomes very low, the respiratory centers become inactive and apnea occurs. During apnea, carbon dioxide is accumulated and oxygen tension is decreased. So, the respiratory centers are stimulated leading to a gradual increase in force of breathing.
Q.168 What are the conditions when Cheyne-Stokes breathing occurs?
Physiological conditions:
- Sleep
- High altitude
- After prolonged hyperventilation
- During hibernation in animals
- In newborn babies
- After severe muscular exercise.
Pathological conditions:
- Increased intracranial pressure
- Cardiac failure
- Uremia
- Narcotic poisoning
- In premature infants.
Q.169 What is Biot’s breathing?
Biot’s breathing is a type of periodic breathing characterized by two alternate periods namely, the period of apnea and period of hyperpnea. There is no waxing and waning. After the apneic period, hyperpnea occurs abruptly.
Q.170 What are the conditions when Biot’s breathing occurs?
Biot’s breathing occurs only in pathological conditions. It occurs in nervous disorders due to lesion or injury to the brain.
Q.171 Define cyanosis. What is its cause?
Cyanosis is defined as the diffused bluish discoloration of the skin and mucus membrane. It is due to the presence of a large amount of reduced hemoglobin in blood. At least 5 gm% of reduced hemoglobin must be present to cause cyanosis.
Q.172 What are the areas of the body where cyanosis is seen markedly?
Though cyanosis is distributed all over the body, it is more marked in areas where the skin is thin like lips, cheeks, ear lobes, nose, and fingertips above the base of nail.
Q.173 What are the conditions when cyanosis occurs?
Cyanosis occurs in:
- Arterial and stagnant hypoxia
- When altered hemoglobin is formed
- During sluggishness of blood flow as in the case of polycythemia.
Q.174 Why cyanosis does not occur in anemia?
Cyanosis usually occurs only when the amount of reduced hemoglobin is more than 5 to 7 gm% but in anemia, the hemoglobin content itself is less. So, cyanosis cannot occur in anemia.
Q.175 Compare the central and peripheral cyanosis?
Comparison between central and peripheral cyanosis
| Central cyanosis | Peripheral cyanosis |
| It is due to hypoxic hypoxia. | It is due to stagnant hypoxia. |
| Extremities become warmer due to increase blood flow to the tissue and hypertension which reflexly produce vasodilatation | Extremities become cooler due to decreased tissue blood flow and hypotension. |
Q.176 What do you mean by Caissons disease?
It is the condition caused by the sudden release of pressure if Caisson underwater is suddenly brought out. This results in abdominal pain, disturbance of the vital center in CNS, and even sudden collapse of a person present within the Caisson.
Q.177 What do you mean by N2 narcosis?
If the body is exposed to high atmospheric pressure, because of high N2 pressure larger amount of N2 will enter into the lungs and thereby in body fluids ultimately causing euphoria, impairment of mental function, and symptoms of alcoholic intoxication. These effects of N2 in higher pressure is called N2 narcosis.
Q.178 Define oxygen toxicity (poisoning). What is its cause?
Increased oxygen content in the tissues is called oxygen toxicity. It is because of breathing pure oxygen at atmospheric pressure for a long time or breathing pure oxygen at high pressure.
Q.179 What is the effect of breathing pure oxygen at atmospheric pressure for a long time?
Breathing pure oxygen at atmospheric pressure for more than 12 hours leads to poisoning of lung tissues and pulmonary edema. The other tissues are not affected very much because of the hemoglobin oxygen buffer system.
Q.180 What is hyperbaric oxygen?
Pure oxygen at a high pressure of about 1,500 mmHg is known as hyperbaric oxygen.
Q.181 What are the effects of breathing hyperbaric oxygen?
Breathing hyperbaric oxygen poisons the lung tissues first and causes pulmonary edema. Afterward, the failure of the hemoglobin buffer system occurs. So, the other organs like the brain are affected because of increased metabolic rate, production of excess of heat, destruction of cellular enzymes, and damage of tissues. When the brain is affected, hyperirritability occurs. It is followed by convulsions, coma, and death.
Q.182 What is acute mountain sickness?
In some instances, the compensatory mechanism to high altitude breaks down and gives rise to serious symptoms known as Monge's disease or acute mountain sickness characterized by:
- Considerable increase in red cell mass and PCV.
- High pulmonary arterial pressure.
- Right heart failure in some cases.
Q.183 What is chronic mountain sickness?
It is the disease occurring in case of failure of the long-term acclimatization process to the residents of high altitude.
The signs and symptoms are:
- Extreme polycythemia
- Increase in viscosity of blood that results in a fall of blood flow
- Increase in BP
- Cyanosis, fatigue, exercise intolerance
- Pulmonary edema.
Q.184 What are the acclimatization to the natives of high landers?
The acclimatization that occurs in the residents who are residing in the high altitude permanently for generations after generations are as follows:
- Short body stature and large-sized chest that results in a high ratio of ventilatory capacity to body mass.
- Hypertrophy of right heart.
- Polycythemia
- Shifting of O2 dissociation curve to right
- Increase in size of carotid bodies.
Q.185 What do you mean by CPR?
If the respiration fails along with the stoppage of heartbeat this procedure is followed until the person is not hospitalized for proper treatment.
The procedures are:
- Cleaning of the airways
- Mouth-to-mouth breathing at the rate of 16-18/min
- External cardiac massage by pressing the lower border of the sternum by 4-5 cm at the rate of 80-90 times/min.
- After every 15 cardiac massage two mouth-to-mouth (15:2) breathing (if two subjects are present. After every 5 cardiac massage 1 mouth-to-mouth (5:1) breathing (if one subject is available).
Q.186 What do you mean by Kussmaul breathing?
During some clinical conditions like diabetic coma, there is rapid and deep breathing eliminating CO2 and bicarbonate. This type of rapid and shallow breathing is known as Kussmaul breathing.
Q.187 What are the sources of carbon monoxide?
- Exhaust of gasoline engines
- Coal mines
- Gases from guns
- Deep wells
- Underground drainage system.
Q.188 What is the difference between the affinity of hemoglobin for carbon monoxide and oxygen?
Hemoglobin has got 200 times more affinity for carbon monoxide than for oxygen.
Q.189 What are the toxic effects of carbon monoxide?
- Carbon monoxide combines with hemoglobin and forms carboxyhemoglobin. This cannot take up oxygen so, anemic hypoxia occurs. The presence of carboxyhemoglobin decreases the release of oxygen from hemoglobin and the oxygen dissociation curve shifts to left
- Carbon monoxide destroys the cytochrome system in the cells.
Q.190 What are the effects of carbon monoxide poisoning?
Breathing air with 1% carbon monoxide causes headaches and nausea. Breathing air with more than 1% carbon monoxide causes loss of consciousness. When the percentage of carbon monoxide in the air is high, death occurs.
Q.191 What is atelectasis? What are its causes?
Atelectasis means the collapse of a part or whole of the lung.
Causes:
- Deficiency of surfactant
- Obstruction of bronchus or bronchiole
- Presence of air (pneumothorax), fluid (hydrothorax), blood (hemothorax) or pus (pyothorax) in pleural space.
Q.192 What are the effects of atelectasis?
- Decrease in the partial pressure of oxygen
- Dyspnea.
Q.193 Define pneumonia. What are its causes?
Pneumonia is the inflammation of lung tissues followed by the accumulation of blood cells, fibrin, and exudates in alveoli leading to the consolidation of the affected part of the lung.
Causes:
- Bacterial or viral infection
- Inhaling noxious chemical agents.
Q.194 What is delirium?
The extreme mental state due to cerebral hypoxia is called delirium.
Q.195 What are the features of delirium?
- Confused mental state
- Illusion
- Hallucination
- Disorientation
- Hyperexcitability
- Loss of memory.
Q.196 What is bronchial asthma?
Bronchial asthma is a respiratory disease characterized by difficulty in breathing with wheezing.
Q.197 What is wheezing? What is it due to?
Wheezing means the whistling type of respiration noticed in bronchial asthma. It is marked during expiration. It is due to obstruction of air passage by:
- Bronchiolar constriction
- Edema of mucus membrane in bronchioles
- Accumulation of mucus.
Q.198 What are the effects of bronchial asthma on the respiratory system?
- Increase in residual volume and functional residual capacity
- Reduction in tidal volume, vital capacity, FEV1, alveolar ventilation, and partial pressure of oxygen in blood
- Acidosis
- Dyspnea
- Cyanosis.
Q.199 What is pleural effusion?
Accumulation of large amounts of fluid in the pleural cavity is called pleural effusion.
Q.200 What is emphysema?
Emphysema is an obstructive respiratory disease in which lung tissue especially the alveolar membrane is damaged.
Q.201 What are the various factors affecting the body at high altitude?
- Hypoxia
- Expansion of gases
- Reduced atmospheric temperature
- Light rays.
Q.202 Why does hypoxia develop at high altitude?
Because of low atmospheric pressure in high altitude, the partial pressure of oxygen is reduced causing hypoxia.
Q.204 What is mountain sickness?
Mountain sickness is the condition characterized by ill effects of hypoxia at high altitude. It is common in persons going to high altitude for the first time.
Q.205 What are the symptoms of mountain sickness?
- Digestive system: Loss of appetite, nausea and vomiting
- Respiratory system: Breathlessness caused by pulmonary edema due to hypoxia
- Nervous system: Headache, depression, disorientation, irritability, lack of sleep, weakness, and fatigue.
Q.206 What is acclimatization?
The adaptation or the adjustment of the body to high altitude is known as acclimatization.
Q.207 What are the important changes in the body during acclimatization?
- Blood: Increase in red blood cell count, hemoglobin content, and oxygen-carrying capacity of blood
- Cardiovascular system: Increase in blood flow to vital organs like heart, brain, and muscles due to increased heart rate and cardiac output
- Respiration: Increase in rate and force of respiration, pulmonary ventilation, pulmonary blood flow, diffusing capacity of gases in alveoli, and uptake of oxygen in blood
- Tissues: Increase in the quantity of oxidative enzyme necessary for metabolism.
Q.208 Define decompression sickness. What are its other names?
Decompression sickness is the disorder that occurs when a person returns rapidly to normal surroundings (atmospheric pressure) after staying for a long time in a place with high atmospheric pressure like deep sea. Other names of this disease:
- Compressed air sickness
- Caisson sickness
- Bends
- Divers palsy.
Q.209 Explain the cause for decompression sickness briefly.
High barometric pressure at deep-sea compresses the gases causing a reduction in the volume of the gases. Oxygen is utilized and carbon dioxide is expired. But, since nitrogen is an inert gas it is neither utilized nor expired. So, after compression, it escapes from blood and gets dissolved in the fat of the tissues and tissue fluid. When the person ascends rapidly to atmospheric pressure, nitrogen is decompressed and escapes from tissues in the form of bubbles. The bubbles obstruct the blood flow producing the embolism and decompression sickness.
Q.210 What are the symptoms of decompression sickness?
- Severe pain, numbness, and itching
- Temporary paralysis and muscle cramps
- Occlusion of coronary artery and coronary ischemia
- Damage of brain tissue or spinal cord due to obstruction of blood flow
- Dizziness, shortness of breath and choking
- Unconsciousness and death.
Q.211 How is decompression sickness prevented?
While ascending from deep sea, ascent should be very slow with short stay at regular intervals. The person affected by decompression sickness is treated by recompression first and then he is brought slowly to atmospheric pressure.
Q.212 What is nitrogen narcosis? When does it occur?
Nitrogen narcosis is the unconsciousness or stupor (lethargy with suppression of sensations and feelings) produced by nitrogen. Its effects are similar to alcoholic intoxication. It occurs in persons like deep-sea divers or underwater tunnel workers who breathe pressurized air under high pressure.
Q.213 What is SCUBA?
SCUBA or self-contained underwater breathing apparatus is the apparatus used by deep-sea divers and the underwater tunnel workers to prevent the ill effects of increased barometric pressure in deep-sea or tunnels.
Q.214 What are the effects of sudden exposure of the body to cold?
When the body is exposed to cold, a large amount of heat is produced by increased metabolic activities and shivering. When the body is exposed to severe cold, the temperature regulating mechanism fails causing frostbite. And sleep or coma occurs.
Q.215 What is frostbite?
Freezing of the surface of the body due to exposure to severe cold is known as frostbite. It is common in ear lobes and digits of hands and feet.
Q.216 What are the effects of exposure of the body to heat?
- Heat exhaustion
- Dehydration
- Heat cramps
- Heatstroke.
Q.217 What is heat stroke?
When body temperature increases above 41°C (106°F) during exposure to severe heat, some severe symptoms occur which are together called heat stroke.
Q.218 What are the effects of heatstroke?
The effects of heat stroke are dizziness, abdominal pain, and unconsciousness. If not treated immediately, damage to brain tissue occurs resulting in death.
Q.219 What is sunstroke?
Prolonged exposure of the body to the sun during summer in desert or tropical areas leads to a condition similar to heatstroke. This is called sunstroke.
Q.220 What are the conditions when artificial respiration is required?
Artificial respiration is required whenever there is an arrest of breathing without cardiac failure. Arrest of breathing occurs during:
- Accidents
- Drowning
- Gas poisoning
- Electric shock
- Anesthesia.
Q.221 What are the methods of artificial respiration?
- Manual methods
- Mechanical methods.
Q.222 Name the manual methods of artificial respiration.
- Mouth-to-mouth breathing method
- Holger-Nielsen (backpressure arm lift) method.
Q.223 Name the mechanical methods of artificial respiration.
- Drinker’s method
- Ventilator method.
Q.224 What are the effects of exercise on the respiratory system?
- Increase in pulmonary ventilation
- Increase in diffusing capacity of oxygen
- Increase in the amount of oxygen consumption.
Q.225 What is oxygen debt?
After severe muscular exercise, the amount of oxygen required by the muscles is greater than the amount of oxygen available. This is called oxygen debt.
Q.226 What is VO2 max? Give values.
The amount of oxygen consumed under maximal aerobic metabolism is called VO2 max. It is the product of cardiac output and the maximal amount of oxygen consumed by the muscles.
During resting condition VO2 max is 35 to 40 ml/kg body weight/minute in males and 30 to 35 ml/kg body weight/minute in females. During exercise, it is increased by 50%.
Q.227 What is respiratory quotient?
The respiratory quotient is the ratio between the volume of carbon dioxide expired and the volume of oxygen consumed. In the resting condition, it is about 0.8. During exercise, it increases to 1.5 to 2.00.

Comments (0)