What are the functions of pancreatic juice?
- Digestive functions: Digestion of proteins, lipids, and carbohydrates
- Neutralizing action: Neutralization of acidity of chyme in intestine.
Q.1 What are the different layers of the gastrointestinal (GI) tract?
Layers of GI tract from outside to inside:
- Serous coat
- Muscular coat
- Submucous coat
- Mucous coat.
Q.2 What are the nerves supplying the GI tract?
GI tract is supplied by two types of nerve fibers:
- Intrinsic nerves:
– Auerbach’s or myenteric nerve plexus present in the muscular layer
– Meissner’s plexus or submucous nerve plexus situated in between the muscular and submucous layers.
- Extrinsic nerves:
– Sympathetic nerve fibers
– Parasympathetic nerve fibers.
Q.3 Name the major salivary glands in human beings.
- Parotid glands
- Submaxillary or submandibular glands
- Sublingual glands.
Q.4 What are the properties of saliva?
Volume : 1000 to 1500 ml/day Reaction and
pH: Slightly acidic with a pH of 6.35 to 6.85
Specific gravity: 1.002 to 1.012.
Q.5 Name the organic substances present in saliva.
- Salivary enzymes:
– Amylase (ptyalin), maltase, lingual lipase, lysozyme, phosphatase, carbonic anhydrase, and kallikrein.
- Other organic substances:
– Proteins
– mucin and albumin
– Blood group antigens
– Free amino acids
– Nonprotein nitrogenous substances
– urea, uric acid, creatinine, xanthine, and hypoxanthine.
Q.6. Name the inorganic substances present in saliva.
Sodium, potassium, calcium, bicarbonates, bromide, chloride, fluoride, and phosphate.
Q.7 What are the nerves supplying the salivary gland?
Salivary glands are supplied by parasympathetic and sympathetic nerves.
Parasympathetic nerves to the parotid gland arise from the inferior salivatory nucleus and reach the parotid gland by passing through the glossopharyngeal nerve. The parasympathetic nerves to submandibular and sublingual glands arise from the superior salivatory nucleus and reach the glands by passing through the facial nerve.
Sympathetic nerves to the salivary glands arise from lateral horns of first and second thoracic segments in the spinal cord and reach the glands through the postganglionic fibers of superior cervical ganglion.
Q.8 What are the effects of stimulation of parasympathetic nerve fibers to salivary glands?
Stimulation of parasympathetic nerve fibers to salivary glands causes vasodilatation and an increase in the secretion of watery saliva.
Q.9 What are the effects of the stimulation of sympathetic nerve fibers to salivary glands?
Stimulation of sympathetic nerve fibers to salivary glands causes vasoconstriction and a decrease in the secretion of saliva that is thick and rich in mucus.
Q.10 How salivary secretion is regulated?
Salivary secretion is regulated by the reflex phenomenon in which both conditioned and unconditioned reflexes are involved.
Q.11 Name some conditions when hyposalivation occurs.
Temporary hyposalivation occurs in emotional conditions like fear, fever, and dehydration. Permanent hyposalivation occurs in sialolithiasis, congenital absence of salivary glands, and Bell’s palsy.
Q.12 What is xerostomia?
Dryness of the mouth due to hyposalivation or absence of salivary secretion (aptyalism) is called xerostomia.
Q.13 Name some conditions when hypersalivation occurs.
- Decay of tooth or neoplasm of mouth or tongue
- Diseases of esophagus, stomach, and intestine
- Neurological disorders like cerebral palsy and mental retardation
- Parkinsonism
- Psychological and psychiatric conditions
- Nausea and vomiting.
Q.14 What is chorda tympani syndrome?
It is the condition characterized by sweating while eating.
Q.15 Name the parts of the stomach.
- Cardiac region
- Fundus
- Body or corpus
- Pyloric region.
Q.16 What are the gastric glands? Mention the types of gastric glands.
Gastric glands are the exocrine glands of the stomach, which secrete gastric juice.
Types of gastric glands:
- Fundic glands situated in the body and fundus
- Pyloric glands situated in the pyloric part
- Cardiac glands situated in the cardiac region.
Q.17 Name the substances secreted by different cells of the gastric gland.
- Chief or pepsinogen cells: Enzymes – pepsinogen, rennin, lipase, gelatinase, and urease
- Parietal or oxyntic cells: Hydrochloric acid and intrinsic factor of Castle
- Mucus neck cells: Mucin
- G cells: Gastrin
- Enterochromaffin (EC) or Kulchitsky cells: Serotonin
- Enterochromaffin-like (ECL) cells: Histamine.
Q.18 What are the properties of gastric juice?
Volume : 1200 ml/day Reaction and
pH: Highly acidic with a pH of 0.9 to 1.2
Specific gravity: 1.002 to 1.004.
Q.19 What is the cause for the high acidity of gastric juice?
Gastric juice is highly acidic because of hydrochloric acid.
Q.20 Name the organic substances present in gastric juice.
- Enzymes – pepsin, rennin, gastric lipase, gelatinase, and urase
- Other organic substances – mucus and intrinsic factor of Castle.
Q.21 What are the functions of gastric mucus?
Mucus:
- Protects the stomach wall from irritation or mechanical injury
- Prevents the digestive action of pepsin on the wall of the stomach
- Protects the gastric mucosa from hydrochloric acid of gastric juice.
Q.22 Briefly explain the secretion of hydrochloric acid in the stomach.
Hydrochloric acid is formed in the canaliculus of the parietal cells of the gastric glands. In the parietal cell, carbon dioxide combines with water to form carbonic acid. Carbonic acid dissociates into hydrogen and bicarbonate ions immediately. The whole reaction is accelerated by the enzyme carbonic anhydrase. The bicarbonate ion diffuses from the cell to the extracellular fluid in exchange for chloride ions. The hydrogen and chloride ions move from the cell into the canaliculus and combine to form hydrochloric acid.
Q.23 What are the functions of gastric juice?
- Digestion of proteins and lipids
- Hemopoietic function – intrinsic factor helps in erythropoiesis
- Protective function – mucus protects the wall of the stomach from proteolytic enzymes and hydrochloric acid
- Antibacterial action – hydrochloric acid destroys the microorganisms entering the gastrointestinal tract through diet
- Activator function – hydrochloric acid activates pepsinogen into pepsin.
Q.24 What are the actions of pepsin?
Pepsin acts on proteins and converts them into proteoses, peptones, and polypeptides. It also causes curdling and digestion of milk (casein).
Q.25 How is pepsinogen converted into pepsin?
Pepsinogen is converted into pepsin by acid medium provided by hydrochloric acid.
Q.26 What is rennin?
Rennin is a milk curdling enzyme present in animals.
Q.27 Name the factors regulating the secretion of hydrochloric acid in the stomach.
Gastrin, histamine, and vagal stimulation increase the secretion of hydrochloric acid. Secretin, gastric inhibitory polypeptide, and peptide YY inhibit acid secretion.
Q.28 Briefly explain Pavlov’s pouch.
It is a small part of the stomach that is incompletely separated from the main portion and made into a bag-like pouch. Russian scientist Pavlov devised it. This pouch is fully innervated with both sympathetic and parasympathetic nerve supply intact. It is useful to study the hormonal and nervous regulation of gastric juice.
Q.29 What is sham feeding?
Sham feeding means false feeding, i.e. the animal eats the food but the food does not reach the stomach. This is done by cutting the esophagus transversely and the cut ends are brought out by making a hole in the neck. So, when the animal swallows the food, it comes out. It is useful to demonstrate the unconditioned reflex during the cephalic phase of gastric secretion.
Q.30 Name the phases of gastric secretion.
- Cephalic phase
- Gastric phase
- Intestinal phase.
Q.31 What is the cephalic phase of gastric secretion?
The sight, smell, or thought of food or the presence of food in the stomach stimulates the secretion of gastric juice. This is known as the cephalic phase of gastric secretion because the impulses are sent from the head. It is purely under nervous control and operates through conditioned and unconditioned reflexes.
Q.32 Briefly explain the gastric phase of gastric secretion.
The secretion of gastric juice when food enters the stomach is called the gastric phase. It is under nervous and hormonal control. Nervous control is operated through local myenteric reflex and vagovagal reflex. The hormonal control is operated through the secretion of gastrin.
Q.33 Briefly explain the intestinal phase of gastric secretion.
When the chyme reaches the small intestine from the stomach, initially there is secretion of gastric secretion due to the action of gastrin. Later, the gastric secretion is inhibited due to enterogastric reflex and GI hormones like secretin, cholecystokinin, gastric inhibitory polypeptide (GIP), vasoactive intestinal polypeptide (VIP), polypeptide YY and somatostatin.
Q.34 What are the effects of alcohol and caffeine on gastric secretion?
Alcohol and caffeine stimulate gastric secretion.
Q.35 What is fractional test meal (FTM)?
It is one of the methods of gastric analysis. After overnight fasting, a sample of gastric juice is collected. Then a test meal is given and the samples of gastric juice are collected at the interval of 15 minutes for about 2½ hours. All the samples are analyzed for peptic activity and gastric acidity.
Q.36 How is gastric juice collected in human beings?
By using Ryle’s tube.
Q.37 What is gastric atrophy?
Gastric atrophy is the condition in which the muscles of the stomach shrink and become weak.
Q.38 What is Zollinger-Ellison syndrome?
It is the condition characterized by the secretion of excess hydrochloric acid in the stomach.
Q.39 What are the basic structures of the exocrine part of the pancreas?
The alveoli or acini are the basic structures of the exocrine part of the pancreas.
Q.40 Name the pancreatic duct. How does it open into the intestine?
The pancreatic duct is called Wirsung’s duct. It joins the common bile duct and forms the ampulla of Vater that opens into the duodenum.
Q.41 What are the properties of pancreatic juice?
Volume : 500 to 800 ml/day Reaction and
pH: Highly alkaline with a pH of 8 to 8.3
Specific gravity: 1.010 to 1.018.
Q.42 What is the cause of the high alkalinity of pancreatic juice?
The presence of a large quantity of bicarbonate is responsible for the high alkalinity of pancreatic juice.
Q.43 Name the enzymes present in pancreatic juice.
- Proteolytic enzymes: Trypsin, chymotrypsin, carboxypeptidases, nuclease, elastase and collagenase
- Lipolytic enzymes: Pancreatic lipase, cholesterol ester hydrolase, phospholipases A and B, collapse and bile salt activated lipase
- Amylolytic enzyme: Pancreatic amylase.
Q.44 What are the different layers of the gastrointestinal (GI) tract?
Layers of GI tract from outside to inside:
- Serous coat
- Muscular coat
- Submucous coat
- Mucous coat.
Q.45 How is trypsinogen converted into trypsin?
Trypsinogen is converted into trypsin by the enzyme enterokinase. Once formed trypsin also converts trypsinogen into trypsin by means of autocatalytic action.
Q.46. What are the actions of trypsin?
- Digestion of proteins: It converts proteins into proteoses and polypeptides
- Curdling of milk: It converts caseinogens in the milk into casein
- Acceleration of blood clotting
- Activation of other enzymes of pancreatic juice: It converts chymotrypsinogen into chymotrypsin and procarboxypeptidases into carboxypeptidases.
Q.47 What are the actions of chymotrypsin?
Chymotrypsin:
- Hydrolyses the proteins into polypeptides
- Digests milk.
Q.48 What is the action of carboxypeptidase?
Carboxypeptidase converts polypeptides into amino acids.
Q.49 What is the importance of pancreatic lipase?
Pancreatic lipase is the strongest lipolytic enzyme in the gastrointestinal tract. 80% of the fat is digested by this enzyme. The absence of pancreatic lipase leads to steatorrhea.
Q.50 Name the hormones, which increase the secretion of pancreatic juice.
Gastrin, secretin, and cholecystokinin.
Q.51 What is the effect of secretin on pancreatic juice?
Secretin causes the secretion of large amounts of watery juice with a high concentration of bicarbonate ion.
Q.52 What is the effect of cholecystokinin on pancreatic juice?
Cholecystokinin causes the secretion of pancreatic juice with more amount of enzymes.
Q.53 What is steatorrhea?
Steatorrhea is the condition in which a large quantity of undigested fat is excreted in feces. It is due to the lack of pancreatic lipase.
Q.54 What is the biliary system or extrahepatic biliary apparatus?
It is the system formed by structures present outside the liver. It includes gallbladder and the extrahepatic bile ducts namely, right and left hepatic ducts, common hepatic duct, cystic duct, and common bile ducts.
Q.55 What are the sources of blood supply to the liver?
The liver receives blood from two sources, the hepatic artery and portal vein.
Q.56 What is the importance of hepatic portal vein?
The hepatic portal vein brings deoxygenated blood from the stomach, intestine, spleen, and pancreas to the liver. Deoxygenated blood contains a large amount of monosaccharides and amino acids.
Q.57 What is bile?
Bile is a golden yellow or greenish fluid produced by the liver.
58 What are the properties of bile?
Volume : 1200 ml/day Reaction and
pH: Alkaline with pH of 8 to 8.6
Specific gravity: 1.010 to 1.011.
Q.59 Name the organic substances present in bile.
Bile salts, bile pigments, cholesterol, fatty acids, lecithin, and mucin.
Q.60 What are the bile salts?
Bile salts are the sodium and potassium salts of bile acids. Bile acids are cholic acid and chenodeoxycholic acid.
Q.61 Explain briefly the formation of bile salts.
The primary bile acids namely, cholic acid and chenodeoxycholic acids are formed in the liver and enter the intestine. Due to the bacterial action in the intestine, the cholic acid is converted into deoxycholic acid and chenodeoxycholic acid is converted into lithocholic acid. Deoxycholic acid and lithocholic acid are called secondary bile acids. Now, these two acids from the intestine enter the liver through enterohepatic circulation. In the liver, the secondary bile acids are conjugated with glycine and taurine forming glycocholic acid and taurocholic acid. These two conjugated bile acids combine with sodium or potassium salt to form bile salts.
Q.62 Name the functions of bile salts.
- Emulsification of fat
- Absorption of fats
- Choleretic action
- Cholagogue action
- Laxative action
- Prevention of gallstone formation.
Q.63 What are the bile pigments?
Bile pigments are bilirubin and biliverdin and these pigments are the excretory products of bile.
Q.64 How are the bile pigments formed?
When the old red blood cells are destroyed in the reticuloendothelial system, hemoglobin is released. It is broken into globin and heme. Heme is split into iron and the pigment biliverdin. Biliverdin is reduced to bilirubin.
Q.65 Explain briefly the circulation of bile pigments.
Bilirubin formed in the reticuloendothelial system is released into blood. It is called free bilirubin. Through blood, it reaches the liver. There, the free bilirubin is conjugated by glucuronic acid to form conjugated bilirubin. Conjugated bilirubin is excreted through bile into the intestine. From the intestine, 50% of conjugated bilirubin enters the liver via enterohepatic circulation and excreted through bile. The remaining 50% of conjugated bilirubin is converted into urobilinogen. Urobilinogen is excreted through urine as urobilin and through feces as stercobilinogen.
Q.66 What is enterohepatic circulation?
The flow of blood from the intestine to the liver through portal vein is known as enterohepatic circulation. Bile salts and bile pigments are transported through enterohepatic circulation.
Q.67 Name the functions of bile.
- Digestive function
- Absorptive function
- Excretory function
- Laxative action
- Antiseptic action
- Choleretic action
- Maintenance of pH in the GI tract
- Prevention of gallstone formation
- Lubrication function
- Cholagogue action.
Q.68 Name the functions of the liver.
- Storage function
- Synthetic function
- Secretion of bile
- Metabolic function
- Excretory function
- Heat production
- Hemopoietic function
- Hemolytic function
- Inactivation of hormones and drugs
- Defensive and detoxification functions.
Q.69. What are the functions of the gallbladder?
- Storage of bile
- Concentration of bile
- Reduction of pH of bile
- Secretion of mucin
- Maintenance of pressure in the biliary system.
Q.70 What are the changes taking place in the bile when it is stored in the gallbladder?
- Reduction in volume due to reabsorption of water
- Concentration of bile due to reabsorption of water and electrolytes
- Reduction of pH of bile from 8 – 8.6 to 7 – 7.6
- Addition of mucin.
Q.71 What are the differences between liver bile and gallbladder bile?
- Liver bile is dilute and gallbladder is concentrated
- The pH of liver bile (8 to 8.6) is more than the pH in gallbladder bile (7 to 7.6)
- Concentration of bile salts, bile pigments, cholesterol, fatty acids, and lecithin is less in liver bile and more in gallbladder bile
- Mucin is absent in liver bile and present in gallbladder bile
- Sodium, chloride, and bicarbonate are more in liver bile than in gallbladder bile
- Calcium and potassium are less in liver bile than in gallbladder bile.
Q.72 What is the normal bilirubin content in blood and at what level jaundice occurs?
Normal bilirubin content in blood is 0.5 to 1.5 mg%. When it exceeds 2 mg% jaundice occurs.
Q.73 What are the types of jaundice?
Jaundice is classified into 3 types depending upon the causes.
- Pre hepatic or hemolytic jaundice – due to excessive destruction of red blood cells
- Hepatic or hepatocellular jaundice – due to damage of hepatic cells
- Posthepatic or obstructive jaundice – due to obstruction of bile duct.
Q.74 What are the causes of prehepatic jaundice?
- Liver failure
- Renal disorder
- Hypersplenism
- Burns
- Infections like malaria
- Hemoglobin abnormalities like sickle cell anemia or thalassemia.
Q.75 What are the causes of hepatic jaundice?
- Infection (infective jaundice) by virus resulting in hepatitis (viral hepatitis)
- Alcoholic hepatitis
- Cirrhosis of liver
- Exposure to toxic materials.
Q.76 What are the causes of posthepatic jaundice?
- Gallstones
- Cancer of biliary system or pancreas.
Q.77 What is cholelithiasis?
The formation of gallstone is called cholelithiasis. Gallstone is formed by the precipitation of cholesterol. Cholesterol in gallbladder bile combines with bile salts and lecithin. Now, cholesterol becomes soluble in water and it is precipitated by forming crystals. To these crystals, bile pigments and calcium ions get attached forming gallstones.
Q.78 What are the causes for gallstone formation?
- Reduction in bile salts and/or lecithin
- Excess of cholesterol
- Disturbed cholesterol metabolism
- Excess of calcium ions due to increased concentration of bile
- Damage or infection of gallbladder epithelium
- Obstruction of bile flow from the gallbladder.
Q.79 What are crypts of Lieberkuhn?
Crypts of Lieberkuhn are the intestinal glands.
Q.80 What are the cells present in the intestinal glands?
- Columnar epithelial cells called enteroctyes, which secrete enzymes
- Argentaffin or enterochromaffin cells which secrete intrinsic factor of Castle
- Goblet cells which secrete mucus
- Paneth cells that secrete defensins (cytokines).
Q.81 What are Brunner’s glands?
Brunner’s glands are the mucus glands present in the first part of the duodenum.
Q.82 What is succus entericus?
Digestive juice secreted by the small intestine is called succus entericus or small intestinal juice.
Q.83 What are the properties of succus entericus?
Volume : 1800 ml/day Reaction and
pH: Alkaline with a pH of 8.3
Q.84 Mention the composition of succus entericus.
- Succus entericus contains water, organic and inorganic substances
- Organic substances are enzymes, mucus, intrinsic factor, and defensins
- Inorganic substances are sodium, calcium, potassium, bicarbonate, chloride, phosphate, and sulfate.
Q.85 What are the enzymes present in succus entericus?
- Proteolytic enzymes: Peptidases – amino peptidase, dipeptidase and tripeptidase
- Lipolytic enzyme: Lipase
- Amylolytic enzymes: Sucrase, maltase, lactase, dextrinase, trehalase
- Enterokinase.
Q.86 What are the functions of succus entericus?
- Digestive function by enzymes
- Protective function by mucus
- Activator function by enterokinase
- Hemopoietic function by intrinsic factor
- Hydrolytic function by water.
Q.87 What are the functions of the small intestine?
- Mechanical function
- Secretory function
- Hormonal function
- Digestive function
- Activator function
- Hemopoietic function
- Hydrolytic function
- Absorptive function.
Q.88 How is succus entericus collected?
Succus entericus is collected by using multilumen tube.
Q.89 What are the properties of large intestinal juice?
Large intestinal juice is a watery fluid and highly alkaline with a pH of 8.0.
Q.90 What is the composition of large intestinal juice?
Large intestinal juice contains water and solids. Solids are organic and inorganic substances. Organic substances are albumin, globulin, mucin, urea, and debris of epithelial cells. Inorganic substances are sodium, calcium, potassium, bicarbonate, chloride, phosphate, and sulfate.
Q.91 What are the functions of large intestinal juice?
- Neutralization of acids
- Lubrication activity.
Q.92 What are the functions of the large intestine?
- Absorptive function: Absorption of water, electrolytes, glucose, alcohol, and drugs like anesthetic agents, sedatives, and steroids
- Formation of feces
- Excretory function: Excretion of mercury, lead, bismuth, and arsenic
- Secretory function: Secretion of mucin, chloride and bicarbonate
- Synthetic function: Synthesis of folic acid, vitamin B12, and vitamin K.
Q.93 What are the causes of constipation?
- Dietary causes – lack of fiber or water
- Irregular bowel habits
- Spasm of sigmoid colon
- Many types of diseases
- Dysfunction of myenteric plexus in large intestine (megacolon).
Q.94 What is megacolon or Hirschsprung’s disease?
Dysfunction of the myenteric plexus in the large intestine causes constipation and accumulation of a large quantity of feces in the colon. This leads to the distension of the colon to a diameter of 4 to 5 inches. This condition is known as megacolon or Hirschsprung’s disease.
Q.95 What are the significances of mastication?
- Breakdown of foodstuffs into smaller particles
- Mixing of saliva with food substances
- Lubrication and moistening of dry food by saliva so that, the bolus can be easily swallowed
- Appreciation of taste of the food.
Q.96 What is deglutition?
Swallowing of food is known as deglutition. In this process, the masticated food from the mouth enters the stomach via the pharynx and esophagus.
Q.97 What are the stages of deglutition?
- Oral stage – the entrance of food into the pharynx from the mouth.
- Pharyngeal stage – the entrance of food into the esophagus from the pharynx.
- Esophageal stage – the entrance of food into the stomach from the esophagus.
Q.98 Explain in brief how the entrance of bolus through different passages other than the esophagus is prevented.
- Return of bolus back into the mouth is prevented by the position of tongue against the roof of the mouth and the high intraoral pressure
- Movement of the bolus into the nasopharynx is prevented by the elevation of the soft palate
- Movement of bolus into the larynx is prevented by
– Approximation of vocal cords
– Forward and upward movement of larynx
– Backward movement of the epiglottis to close the larynx causing deglutition apnea.
Q.99 What is deglutition apnea or swallowing apnea?
The temporary arrest of breathing during the pharyngeal stage of deglutition is called deglutition apnea or swallowing apnea.
Q.100 What is the significance of deglutition apnea?
Deglutition apnea prevents the entrance of bolus into the larynx during swallowing.
Q.101 What are the movements of the esophagus during deglutition?
Movements of the esophagus during deglutition are the primary and secondary peristaltic contractions. Sometimes tertiary contraction may also occur.
Q.102 hat is dysphagia? What are its causes?
Difficulty in swallowing is called dysphagia.
Its causes:
- Mechanical obstruction of esophagus
- Decreased movement of the esophagus
- Muscular disorders.
Q.103 What is esophageal achalasia?
It is a neuromuscular disease characterized by the accumulation of food in the esophagus. It is because the lower esophageal (cardiac) sphincter fails to relax during swallowing.
Q.104 What is gastroesophageal reflux disease (GERD)?
GERD is a disorder characterized by the regurgitation of acidic gastric content into the esophagus. It is due to the weakness or incompetence of cardiac sphincter.
Q.105 Define peristalsis.
Peristalsis is the wave of contraction followed by wave of relaxation that travels in an aboral direction.
Q.106 What is the significance of peristalsis?
By peristalsis, the contents are propelled along the gastrointestinal tract.
Q.107 Trace the pathway for deglutition reflex.
The receptors are present in the pharynx. Afferent fibers pass through the glossopharyngeal nerve. The Center is in the medulla oblongata. Efferent fibers pass through hypoglossal, glossopharyngeal, and vagus nerves. Effectors are the muscles of the pharynx and the esophagus.
Q.108 What are the types of movements of the stomach?
- Hunger contractions which occur when the stomach is empty
- Peristalsis when the stomach is filled with food.
Q.109 What is receptive relaxation?
Relaxation of the upper part of the stomach when bolus enters the stomach from the esophagus is called receptive relaxation.
Q.110 What are the factors influencing the emptying of the stomach?
- Volume of gastric content
- Consistency of gastric content
- Chemical composition of gastric content
- pH of gastric content
- Osmolar concentration of gastric contents.
Q.111 What are the factors, which inhibit gastric emptying?
- Nervous factor – enterogastric reflex
- Hormonal factors – hormones VIP, GIP, secretin, and cholecystokinin.
Q.112 What is enterogastric reflex?
When the chyme enters the intestine, the gastric muscle is inhibited and the gastric movements are reduced or stopped. It causes stoppage of gastric emptying. This is known as enterogastric reflex and it involves the vagus nerve.
Q.113 What are the movements involved in vomiting?
Vomiting involves antiperistalsis in the intestine, stomach, and esophagus, relaxation of lower and upper esophageal sphincters, closure of glottis, and contraction of abdominal muscles.
Q.114 Trace the pathway for vomiting. Receptors are mostly in the gastrointestinal tract.
Afferent fibers are vagus and sympathetic afferent fibers. The Center is in medulla oblongata near tractus solitarius. Efferent fibers are the fibers of V, VII, IX, X, and XII cranial nerves and spinal nerves. Effectors are the muscles of the gastrointestinal tract and abdominal muscles.
Q.115 What are the movements of the small intestine?
- Mixing movements – segmentation movements and pendular movements
- Propulsive movements – peristaltic movements and peristaltic rush
- Peristalsis in fasting (migrating motor complex)
- Movements of villi.
Q.116 What is peristaltic rush? What is its cause?
Peristaltic rush is a powerful peristaltic contraction that begins in the duodenum, passes through the entire length of the small intestine, and reaches the ileocecal valve. It is by excessive irritation of the intestinal mucus membrane or extreme distention of intestine.
Q.117 What is the significance of the peristaltic rush?
Peristaltic rush sweeps the contents of the small intestine into the colon and thus it relieves the small intestine off irritant substances or excessive distention.
Q.118 What is peristalsis in fasting or migrating motor complex?
It is the most powerful peristaltic contraction involving a large portion of the stomach or intestine during the period of fasting or several hours after the meals. It starts in stomach and runs through the entire length of the small intestine.
Q.119 What is the significance of migrating motor complex?
It sweeps the excessive digestive secretions into the colon and prevents the accumulation of secretions in the stomach and small intestine.
Q.120 What are the movements of the large intestine?
- Mixing movements – segmentation contractions
- Propulsive movements – mass peristalsis.
Q.121 What is the significance of mass peristalsis or mass movement?
It propels the feces from the colon towards the anus.
Q.122 What is gastrocolic reflex?
The distention of the stomach with the entrance of food causes contraction of the colon and entrance of feces into the rectum. This is known as gastrocolic reflex.
Q.123 What is the nerve supply to internal and external anal sphincters?
Internal anal sphincter that is formed by smooth muscle fibers is innervated by parasympathetic fibers via the pelvic nerve. The external anal sphincter that is formed by skeletal muscle fibers is innervated by somatic nerve fibers via the pudendal nerve.
Q.124 Trace the pathway for defecation reflex.
Receptors are in the rectum.
Afferent fibers pass via pelvic nerve.
Center is in sacral segment of the spinal cord.
Efferent fibers pass via the pelvic nerve.
Effectors are muscles of the rectum and internal sphincter.
Q.125 What is the importance of the pudendal nerve?
The pudendal nerve always keeps the external anal sphincter constricted. During the defecation reflex, the pudendal nerve is inhibited by impulses arising from the cerebral cortex and this causes relaxation of the external anal sphincter and defecation.
Q.126 What are the gastrointestinal hormones?
Gastrointestinal hormones are the local hormones secreted in the stomach and intestine.
Q.127 Name the cells secreting the gastrointestinal hormones.
APUD (amine precursor uptake and decarboxylation) cells present in the gastrointestinal tract secrete the gastrointestinal hormones.
Q.128 Name the hormones secreted by the stomach.
Gastrin, GIP, somatostatin, and motilin.
Q.129 Name the hormones secreted by the small intestine.
Secretin, cholecystokinin, GIP, VIP, glucagon, glicentine, GLP-2. somatostatin, pancreatic polypeptide, peptide YY, neuropeptide Y, motilin, and substance P.
Q.130 What is the function of Gastric Inhibitory Peptide (GIP)?
GIP is secreted by the duodenum and inhibit the stomach motility and secretion.
Q.131 What is the function of Gastric Releasing Peptide (GRP)?
GRP stimulates the release of gastrin from G cell.
Q.132 What is Migrating Myoelectric Complex (MMC)?
It is the propulsive movement initiated during fasting which beings in the stomach and moves undigested material from the stomach to the small intestine and finally into the colon.
Q.133 Which are the enzymes secreted in the stomach in an inactive form?
| Inactive form | Active form | |
| Trypsinogen | enterokinase | Trypsin |
| Chymotrypsinogen | trypsin | Chymotrypsin |
| Procarboxy- peptidase | trypsin | Carboxypeptidase |
Q.134 What are micelle?
They are water soluble sphere with a lipid soluble interior.
Q.135 What are the functions of micelle?
They help in digestion, transport, and absorption of lipid soluble substance from the duodenum to the distal ileum.
Q.136 What are stercobilin?
Produced from the metabolism of bilirubin by interstinal bacteria. It gives brown color to the stool.
Q.137 What is the action of parasympathetic and sympathetic nerve supply on salivary glands?
The parasympathetic fibers are secretomotor in action, while the sympathetic fibers are vasoconstrictors in action.
Q.138 What are the digestive enzymes present in gastric juice?
These are pepsinogen, renin, and lipase.
Q.139 What are the function of HCl in gastric juice?
HCl is bactericidal in action; it hydrolyses the food and acids in digestion. It activates pepsinogen. It also helps in iron and calcium absorption.
Q.140 What is the action of pepsinogen?
Pepsinogen is activated into pepsin which along with HCl converts protein into peptones and proteoses.
Q.141 What is the role of renin?
Renin curdles the milk and converts caseinogen first into paracesinogen and the calcium paracaseinate.
Q.142 Which are the digestive enzymes present in the pancreatic juice?
These are trypsinogen, chymotrypsinogen, amylase (amylopsin), and (stypsin).
Q.143 What is the function of trypsinogen and chymotrypsinogen?
Trypsinogen is activated by enterokinase into trypsin, which in turn is activated chymotrysinogen into chymotrypsin. These convert proteoses and peptones up to the dipeptides stage.
Q.144 Name the various enzymes present in the succus entericus?
These are erepsin (peptidase), nuclease, nucleosidase, arginase, amylase, maltase, sucrase, lactase, and enterokinase.
Q.145 What is the role of nuclease, nucleosidase, and nucleotidase?
These are concerned with the digestion of nucleoproteins.
Q.146 What is the action of arginase?
Arginase converts arginine into urea and ornithine.
Q.147 What is the action of sucrase?
Sucrase splits sucrose into fructose and glucose.
Q.148 What is the action of maltase?
Maltase converts maltose into two molecules of glucose.
Q.149 What is the action of lactase?
Lactase converts lactose into glucose and galactose.
Q.150 What are the actions of secretin?
Secretin:
- Causes secretion of watery juice with more water and bicarbonate ions
- Inhibits secretion of gastric juice
- Inhibits motility of stomach
- Causes constriction of pyloric sphincter
- Increases the potency of action of cholecystokinin on pancreatic secretion.
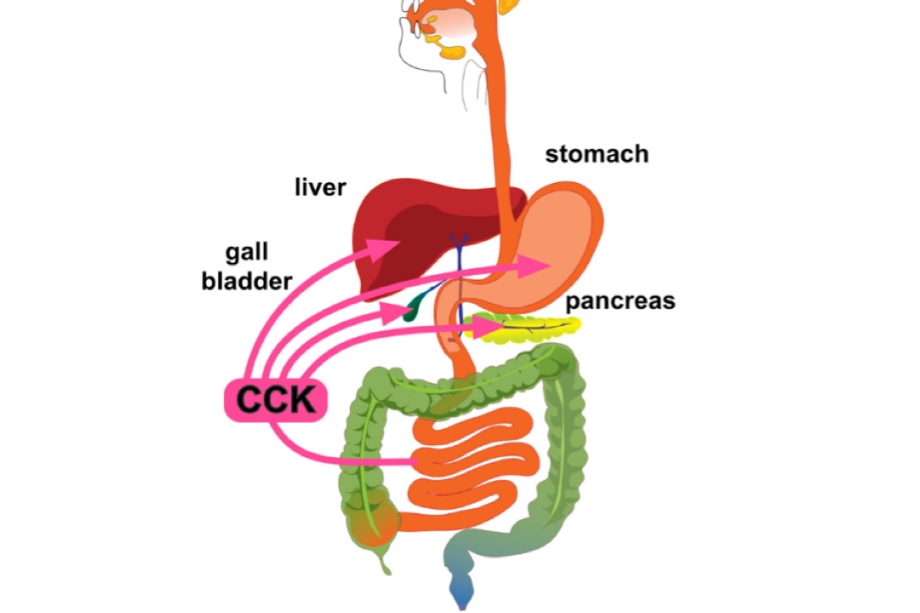
Q.151 What are the actions of cholecystokinin?
Cholecystokinin:
- Contracts gallbladder
- Causes secretion of pancreatic juice with a large amount of enzymes
- Accelerates the activity of secretin
- Increases the secretion of enterokinase
- Inhibits the gastric motility
- Increases the motility of the intestine and colon
- Augments contraction of pyloric sphincter
- Plays an important role in satiety by suppressing hunger
- Induces drug tolerance to opioids.
Q.152 How is carbohydrate digested?
Carbohydrate digestion starts in the mouth by ptyalin and continues in the stomach where gastric amylase also acts. Final digestion occurs in small intestine by pancreatic amylase, sucrase, maltase, lactase, dextrinase, and trehalase.
Q.153 How is carbohydrate absorbed from the small intestine?
Carbohydrate is absorbed from small intestine mainly as monosaccharides (glucose, galactose and fructose).
Q.154 How is protein digested?
Protein digestion starts only in the stomach. Pepsin breaks proteins into proteoses, peptones, and large polypeptides. In the small intestine, the final digestion of proteins occurs because of proteolytic enzymes in pancreatic juice and succus entericus.
Q.155 How is protein absorbed from the small intestine?
Protein is absorbed from the small intestine mainly as amino acids.
Q.156 How is lipid digested?
Lipid digestion starts in the stomach by gastric lipase. But it is a very weak lipolytic enzyme. In the small intestine, most of the lipid is digested by pancreatic lipase. Succus entericus also contains lipase but it is very weak and its action is negligible.
Q.157 Name the bile pigments present in the bile juice.
These are bilirubin and biliverdin.
Q.158 What is the nature of bile pigments? Is it excretory or secretory?
Bile pigments are excretory products of bile.
Q.159 What is the normal daily secretion of bile juice?
It is approximately 0.5-1 liter.
Q.160 What are the functions of bile salts?
Bile salts emulsify fat and render them water-soluble (hydrotropic action): activate lipase: help in absorption of fat, vitamin A, D, E, and K; stimulate peristalsis; and act as cholegogues.
Q.161 What is the cholagogues?
Cholegogue is the agent, which tends to increase the bile flow and its expulsion from biliary passages into the intestines.
Q.162 What is xerostomia?
Xerostomia is a dry mouth caused by mouth breathing or deficient salivary secretion in the mouth. Q.163 What is ptyalism? Ptyalism is excessive salivation produced reflexly by irritation of mouth or esophagus or by drugs.
Q.164 What is the normal daily secretion of bile?
It is 0.5 to 1 liter.
Q.165 What is hepatocrinin?
It is a hormone found in intestinal extract and acts as a stimulant for bile secretion.
Q.166 What is the role of bile salts in lipid digestion?
The lipid molecules are not soluble in water due to the surface tension. So, the lipids cannot be digested by any lipolytic enzymes. Due to the detergent action of bile salts in the small intestine, the lipid molecules become water-soluble. This action of bile salts is known as emulsification. During this, the bile salts convert the lipid substances into micelles. The emulsified fat molecules in micelles are easily digested by lipolytic enzymes.
Q.167 How is lipid absorbed from the small intestine?
Lipid is absorbed from the small intestine in two forms:
- In the form of fatty acids which are absorbed into the blood by diffusion.
- In the form of chylomicrons, which contain triglycerides, and cholesterol esters. Because of the larger size, chylomicrons cannot pass through the membrane of blood capillaries. And, these lipid materials are absorbed into lymph vessels and transferred into blood from lymph.
Q.168 What are lipoproteins?
Lipoproteins are the small particles in the blood that contain cholesterol, phospholipids, triglycerides, and proteins (beta globulins called apoproteins). Lipoproteins are very low-density lipoproteins (VLDL), intermediate low-density lipoproteins (IDL), low-density lipoproteins (LDL), and high-density lipoproteins (HDL).
Q.169 What are the importance of HDL and LDL?
HDL (good cholesterol) carries cholesterol and phospholipids from tissues and organs back to the liver for degradation and elimination. It prevents the deposition of cholesterol on the walls of arteries by carrying cholesterol away from arteries to the liver. A high level of HDL indicates a healthy heart because it reduces the blood cholesterol level. LDL (bad cholesterol) carries cholesterol and phospholipids from the liver to muscles, other tissues, and organs such as the heart. It is responsible for the deposition of cholesterol on walls of arteries causing atherosclerosis. A high level of LDL increases the risk of heart disease.
Q.170 What is lipid profile?
The lipid profile is a group of blood tests that are carried out to determine the risk of coronary artery diseases (CAD).
Q.171 What are the tests involved in the lipid profile? Give the normal values.
- Total cholesterol (200-240 mg%)
- Triglyceride (150-200 mg%)
- HDL (40-60 mg%)
- LDL (60-100 mg%)
- Total cholesterol—HDL ratio (2-6).
Also read: Physiology Questions & Answers

Comments (0)