Renal Physiology Viva
Q.1 What are the functions of the kidney?
The primary function of the kidney is homeostasis, i.e. the maintenance of the internal environment.
Various functions of the kidney:
- Role in homeostasis – by the formation of urine and excretion of water, electrolytes, and waste products through urine
- Hemopoietic function
- Endocrine function
- Regulation of blood pressure
- Regulation of blood calcium level.
Q.2 Name the layers of the kidney.
- Outer cortex containing renal corpuscles and convoluted tubules
- The inner medulla contains tubular and vascular structures arranged in the form of medullary pyramids
- The renal sinus contains the renal pelvis, major calyces, minor calyces, branches of nerves and arteries, tributaries of veins, loose connective tissue, and fat.
Q.3 What are uriniferous tubules? Name their parts.
Uriniferous tubules are the tubular structures forming the parenchyma of the kidney. Each uriniferous tubule consists of nephrons and collecting ducts.
Q.4 Define nephron.
A nephron is defined as a structural and functional unit of the kidney.
Q.5 How many nephrons are present in each kidney?
1 to 1.3 million nephrons.
Q.6 What are the two types of nephrons?
- Cortical or superficial nephrons whose renal corpuscles are situated in the outer part of the cortex
- Juxtamedullary nephrons whose renal corpuscles are situated in the inner part of the cortex near the medulla.
Q.7 What are the parts of the nephron?
- Renal corpuscle or Malpighian corpuscle
- Tubular portion or renal tubule.
Q.8 What are the structures of the renal corpuscle?
- Glomerulus
- Bowman’s capsule encloses the glomerulus.
Q.9 What is glomerulus?
The glomerulus is a tuft of capillaries formed from the afferent arteriole and drained by an efferent arteriole.
Q.10 What are the layers of Bowman’s capsule?
- Inner visceral layer
- Outer parietal layer.
Q.11 What are podocytes?
Podocytes are the epithelial cells of the visceral layer of Bowman’s capsule, which are connected to the basement membrane by means of foot-like projections called pedicles.
Q.12 What are the parts of the renal tubule?
- Proximal convoluted tubule
- Loop of Henle that includes the thick descending limb, thin descending limb, hairpin bend, thin ascending limb, and thick ascending limb
- The distal convoluted tubule.
Q.13 What is the unique feature of the wall of the proximal convoluted tubule?
The wall of the proximal convoluted tubule is formed by brush-bordered cuboidal epithelial cells.
Q.14 What is the advantage of brush-bordered cuboidal epithelial cells in proximal convoluted tubules?
The brush-bordered cuboidal epithelial cells increase the surface area for reabsorption.
Q.15 What is the juxtaglomerular apparatus?
It is a specialized organ situated near the glomerulus of each nephron.
Q.16 What are the parts of the juxtaglomerular apparatus?
The juxtaglomerular apparatus is formed by three different parts :
- Macula densa
- Extraglomerular mesangial cells
- Juxtaglomerular cells.
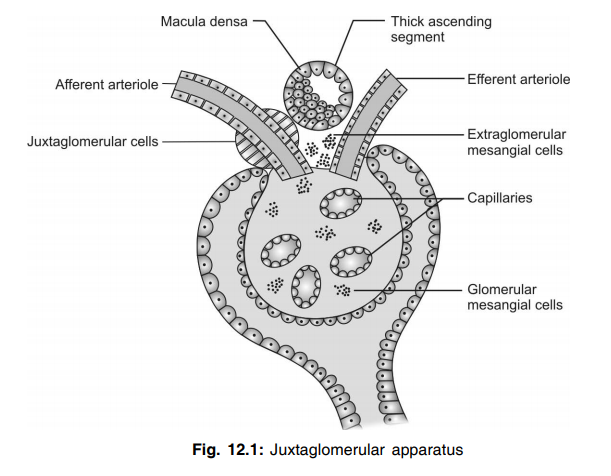
Q.17 What is macula densa?
Macula densa is the part of the distal convoluted tubule near the afferent arteriole, which is formed by tightly packed cuboidal epithelial cells.
Q.18 What are extraglomerular mesangial cells?
Extraglomerular mesangial cells are a special type of agranular or lacis cells situated in the triangular region bound by afferent arteriole, efferent arteriole, and macula densa.
Q.19 What are juxtaglomerular cells?
Juxtaglomerular cells are the specialized type of smooth muscle cells present in the afferent arteriole before it enters the Bowman’s capsule. This part of the afferent arteriole is thickened like a cuff called a polar cushion or polkissen.
Q.20 What are the functions of the juxtaglomerular apparatus?
- Secretion of renin
- Secretion of other substances – prostaglandin, cytokines, and thromboxane A2
- Regulation of glomerular blood flow and glomerular filtration rate.
Q.21 What is the role of renin in the body?
Renin converts inactive angiotensinogen into angiotensin I. Angiotensin I is converted into angiotensin II by the converting enzyme. Angiotensin II is converted into angiotensin III by angiotensinases. Angiotensin III is converted into angiotensin IV.
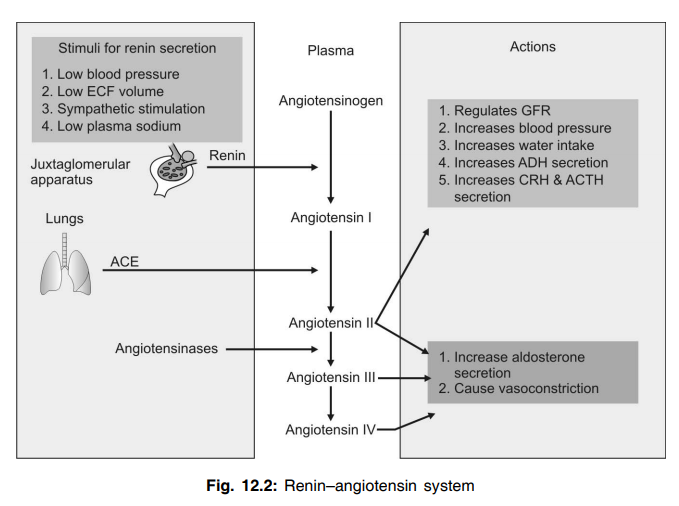
Q.22 Name the factors that stimulate renin secretion.
- Decreased arterial blood pressure
- Reduction in ECF volume
- Increased sympathetic activity
- Decreased load of sodium and chloride in macula densa.
Q.23 What are the functions of angiotensins?
Angiotensin I is physiologically inactive.
Angiotensin II:
- Increases blood pressure
- Increases aldosterone secretion
- Regulates glomerular filtration rate
- Inhibits response of baroreceptor reflex Angiotensins III and IV:
- Increase the blood pressure
- Increase the aldosterone secretion.
Q.24 How much of blood is supplied to both the kidneys?
1300 ml/minute.
Q.25 How is renal blood flow measured?
By renal clearance test using para amino hippuric acid.
Q.26 What is autoregulation? What are the mechanisms involved in renal autoregulation?
The intrinsic ability of an organ to regulate its own blood flow is called autoregulation. Renal autoregulation involves myogenic response and tubuloglomerular feedback.
Q.27 What are the special features (peculiarities) of renal circulation?
- Renal arteries arise directly from the aorta
- Kidneys receive the maximum amount of blood (1,300 ml/minute) next to the liver (1,500 ml/minute)
- Whole blood passes through the glomerulus
- Renal circulation has a portal system
- The capillary pressure in the glomerulus is very high (60 mm Hg)
- Peritubular capillaries form a low-pressure bed
- The autoregulation is well established in the kidney.
Q.28 What is the normal urinary output?
1 to 1.5 L/day.
Q.29 Name the processes involved in urine formation.
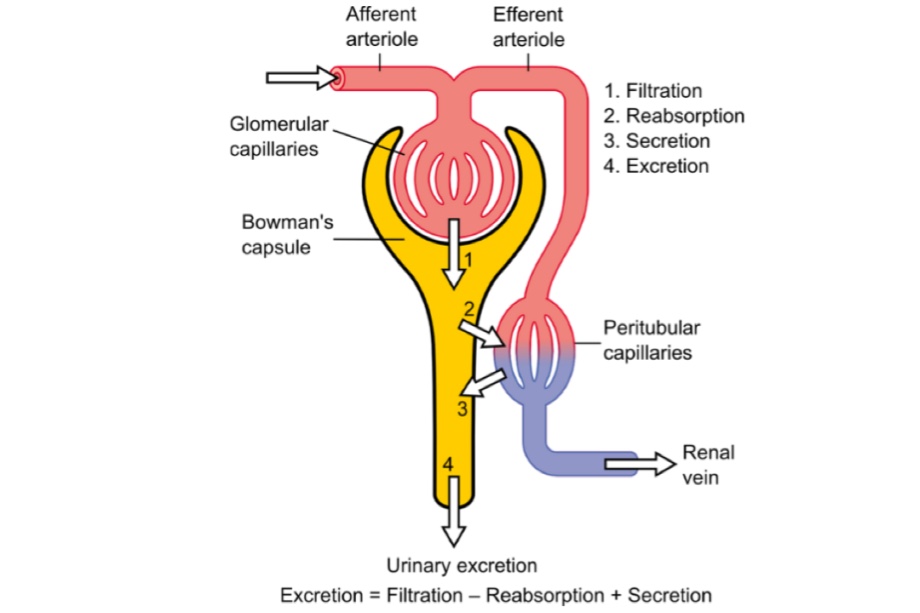
The processes involved in the formation of urine are:
- Glomerular filtration
- Tubular reabsorption
- Tubular secretion or excretion.
Q.30 What is glomerular filtration?
When the blood passes through the glomerular capillaries, the plasma is filtered into the Bowman’s capsule. This process is called glomerular filtration and the filtered fluid is called glomerular filtrate.
Q.31 What is the composition of glomerular filtrate?
The glomerular filtrate is the plasma without plasma proteins, i.e. all the substances present in the plasma are present in glomerular filtrate except plasma proteins.
Q.32 Why glomerular filtration is called ultrafiltration?
Glomerular filtration is called ultrafiltration because even the minute particles are filtered from the glomerular capillary into Bowman’s capsule.
Q.33. Define glomerular filtration rate.
The total amount of filtrate formed in all the nephrons of both kidneys per unit time is known as the glomerular filtration rate (GFR).
Q.34 What is the normal value of GFR?
125 ml/minute or 180 L /day.
Q.35 What is filtration fraction?
The fraction or part of the renal plasma that becomes the filtrate is called filtration fraction. Or, it is the ratio of renal plasma flow and glomerular filtration rate that is expressed in percentage.
Q.36 What is the normal filtration fraction?
15 to 20%
Q.37 Name the pressures, which determine the GFR.
- Glomerular capillary pressure (60 mmHg)
- Colloidal osmotic pressure in the glomeruli (25 mmHg)
- Hydrostatic pressure in the Bowman’s capsule (15 mmHg). The glomerular capillary pressure favors filtration. Colloidal osmotic pressure and hydrostatic pressure oppose or prevent
filtration.
Q.38 What is net or effective filtration pressure? How much is it?
The balance between the pressure favoring filtration and pressures opposing filtration is known as net or effective filtration pressure. Effective filtration pressure = 60 – (25 + 15) mm Hg Normally it is 15 to 20 mmHg.
Q.39 What is Starling’s hypothesis?
Starling’s hypothesis states that the net filtration through the capillary membrane is proportional to the hydrostatic pressure difference across the membrane minus the oncotic pressure difference.
Q.40 What is the filtration coefficient?
Filtration coefficient is the GFR in terms of net filtration pressure. It is the glomerular filtration rate per mmHg of effective filtration pressure.
Q.41 Name the factors affecting GFR.
- Tubuloglomerular feedback
- Glomerular capillary pressure
- Colloidal osmotic pressure
- Hydrostatic pressure in Bowman’s capsule
- Renal blood flow
- Constriction of afferent arteriole
- Constriction of efferent arteriole
- Systemic arterial pressure
- Sympathetic stimulation
- Surface area of capillary membrane
- Permeability of capillary membrane
- Contraction of glomerular mesangial cells
- Hormonal and other factors.
Q.42 What is tubular reabsorption?
When the glomerular filtrate passes through the renal tubule, a large quantity of water, electrolytes, and other substances are reabsorbed back into the blood in peritubular capillaries. This process is known as tubular reabsorption.
Q.43 Why the tubular reabsorption is called selective reabsorption?
The cells of the renal tubule selectively reabsorb the substances present in the glomerular filtrate according to the need of the body. So, the tubular reabsorption is called selective reabsorption.
Q.44 Name the substances reabsorbed in the proximal convoluted tubule.
Glucose, amino acids, sodium, potassium, calcium, bicarbonates, chlorides, phosphates, uric acid, and water.
Q.45 Name the substances reabsorbed in the loop of Henle.
Sodium and chloride.
Q.46 Name the substances reabsorbed in the distal convoluted tubule.
Sodium, bicarbonate, and water.
Q.47 What are the high threshold substances?
The substances which are completely reabsorbed from the renal tubules and do not appear in urine under normal conditions are known as high-threshold substances. These substances appear in urine only if their concentration in plasma is very high or in renal diseases when reabsorption is inhibited.
Examples: Glucose, amino acids, and vitamins.
Q.48 What are low-threshold substances?
The substances which are reabsorbed only to a minimum extent and appear in urine even in normal conditions, are known as low-threshold substances. Examples: Uric acid, phosphates, etc.
Q.49 What are non-threshold substances?
The metabolic end products that are not at all reabsorbed from renal tubules and appear in urine irrespective of their plasma level are known as non-threshold substances. Example: Creatinine.
Q.50 What is the tubular maximum (Tm)?
The maximum rate at which a substance is reabsorbed from the renal tubule is called tubular maximum (Tm).
Q.51 What is TmG?
The tubular maximum for glucose, i.e. the maximum rate at which glucose is reabsorbed from the renal tubule is called TmG. It is about 380 mg/minute.
Q.52 What is the threshold value?
The blood level of a substance below which it is completely reabsorbed and does not appear in urine is known as the threshold value for that substance. When the concentration increases above that level in blood, the excess amount is excreted through urine.
Q.53 What is the renal threshold for glucose?
180 mg%.
Q.54 What are the mechanisms involved in tubular reabsorption?
- Active reabsorption
- Passive reabsorption.
55 Name the substances reabsorbed actively from renal tubules.
Sodium, calcium, potassium, phosphates, sulfates, bicarbonates, glucose, amino acids, ascorbic acid, uric acid, and ketone bodies.
Q.56 Name the substances reabsorbed passively from renal tubules.
Chloride, urea, and water.
Q.57 How is water reabsorbed from renal tubules?
In two ways:
- Obligatory water reabsorption in proximal convoluted tubule
- Facultative water reabsorption in the distal convoluted tubule.
Q.58 What are the substances secreted into renal tubules?
Potassium is secreted in the distal convoluted tubule and collecting duct. Ammonia is secreted in the proximal convoluted tubule. Hydrogen ions are secreted in proximal and distal convoluted tubules.
Q.59 What are the factors, which determine the concentration of urine?
- Medullary gradient
- ADH mechanism.
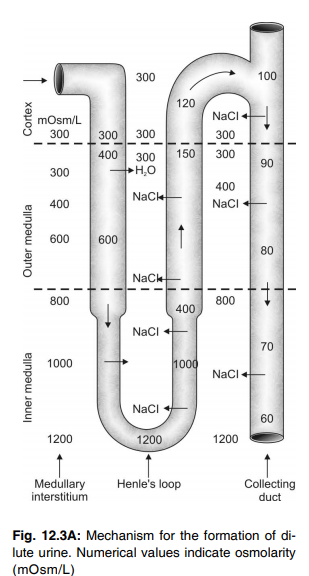
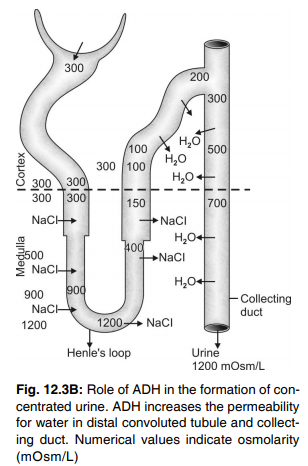
Q.60 What is medullary gradient?
The medullary gradient is the gradual increase in the osmolarity of medullary interstitial fluid from 300 milliosmoles/L near the cortex up to 1,200 milliosmoles/L at the innermost part of the medulla.
Q.61 How is medullary gradient developed and maintained?
The medullary gradient is developed and maintained by the countercurrent mechanism. The development of the medullary gradient is because of the counter-current multiplier and the maintenance of the medullary gradient is because of the counter-current exchanger.
Q.62 What is a counter-current system?
The flow of fluid in opposite directions through ‘U’ shaped tubules is known as a counter-current system.
Q.63 Name the divisions of the counter-current system in the kidney.
- Countercurrent multiplier that is formed by the loop of Henle
- Countercurrent exchanger that is formed by vasa recta.
Q.64 Why the loop of Henle is called a counter-current multiplier?
The loop of Henle is called a countercurrent multiplier because it is responsible for the increase or multiplication of osmolarity in medullary interstitium.
Q.65 Why vasa recta is called a counter-current exchanger?
Vasa recta is called a counter-current exchanger because it helps to exchange the sodium ions between the ascending limb and descending limb of the loop of Henle by which the hyperosmolarity of medullary interstitium and medullary gradient are maintained.
Q.66 What are the special features of vasa recta, which help it to act as a counter-current exchanger?
- It has got an ascending limb and a descending limb
- Only 5% of blood flow to the kidney passes through the vasa recta
- The velocity of blood flow through the vasa recta is very low.
Q.67 How does the final concentration of urine occur?
The final concentration of urine occurs under the influence of antidiuretic hormone (ADH). ADH increases the water reabsorption in distal convoluted tubule and collecting duct and causes concentration of urine.
Q.68 How is urine acidified?
Urine is acidified by the secretion of hydrogen ions in the distal convoluted tubule.
Q.69 How are the hydrogen ions secreted in renal tubules?
Hydrogen ions are secreted in the exchange of sodium ions and by the formation of ammonia in the renal tubules.
Q.70 Name the renal function tests.
- Routine examination of urine
- Examination of blood
- Examination of urine and blood.
Q.71 Define plasma clearance.
Plasma clearance is the amount of plasma that is cleared off a substance in a given unit of time.
Q.72 What are the advantages of determining plasma clearance?
Determination of plasma clearance helps to measure:
- Glomerular filtration rate
- Renal plasma flow
- Renal blood flow.
Q.73 Name the substances used to measure glomerular filtration rate and renal plasma flow by plasma clearance.
Inulin is used to measure glomerular filtration rate and para aminohippuric acid is used to measure renal plasma flow.
Q.74 Classify renal disorders.
- Acute renal failure
- Chronic renal failure.
Q.75 What is detrusor muscle?
The smooth muscle forming the body of the urinary bladder is known as the detrusor muscle.
Q.76. Mention the differences between the internal and external urethral sphincters.
- Internal urethral sphincter is formed by smooth muscle but the external urethral sphincter is formed by skeletal muscle
- Internal sphincter is innervated by sympathetic and parasympathetic fibers of the autonomic nervous system, whereas, the external sphincter is innervated by somatic nerve fibers
- The internal sphincter functions under reflex control and the external sphincter is under voluntary control.
Q.77 Name the nerves supplying the urinary bladder and sphincters.
Detrusor muscle and internal sphincter are supplied by parasympathetic fibers (pelvic nerve) and sympathetic fibers (hypogastric nerve). The external sphincter is supplied by somatic nerve fibers (pudendal nerve).
Q.78 What is the action of the parasympathetic nerve on the urinary bladder and internal sphincter?
When stimulated, the parasympathetic (pelvic) nerve causes contraction of the detrusor muscle and relaxation of the internal sphincter leading to micturition. Hence it is called the nerve of micturition or nerve of emptying.
Q.79 What is the action of the sympathetic nerve on the urinary bladder and internal sphincter?
Stimulation of the sympathetic (hypogastric) nerve causes relaxation of the detrusor muscle and constriction of the internal sphincter. This helps in filling of the urinary bladder and so it is called the nerve of filling.
Q.80 What is the action of the pudendal (somatic) nerve on the external sphincter?
The pudendal (somatic) nerve is always active and keeps the external sphincter constricted. When urine enters the urethra from the bladder, the pudendal nerve is inhibited and the external sphincter relaxes leading to micturition. Thus, the pudendal nerve is responsible for voluntary control of micturition.
Q.81 What is cystometrogram?
Cystometrogram is the graphical recording of pressure changes in relation to volume changes in the urinary bladder while filling.
Q.82 What is intravesical pressure?
The pressure in the urinary bladder is known as intravesical pressure.
Q.83 When does the desire for micturition arise?
The desire for micturition arises when about 300 ml of urine is collected in the urinary bladder and the intravesical pressure increases to about 10 to 15 cm H2O.
Q.84 What is the maximum amount of urine collected in the bladder and intravesical pressure up to which the voluntary control of micturition is possible?
Voluntary control of micturition is possible up to 600 to 700 ml of urine collection in the urinary bladder at which the intravesical pressure is about 35 to 40 cm H2O. When the volume of urine in the bladder increases beyond 700 ml, the pressure rises to 40 cm H2O. Now, the voluntary control of micturition fails.
Q.85 Explain briefly the micturition reflex.
Micturition reflex occurs in two phases. Initially, when 300 to 400 ml of urine is collected in the urinary bladder, the stretch receptors in the wall of the bladder are stimulated. This leads to contraction of detrusor muscles and relaxation of the internal sphincter and urine flows into the urethra from the urinary bladder.
In the second phase, when urine flows through the urethra, the stretch receptors present in the urethra are stimulated. This leads to inhibition of the pudendal nerve, relaxation of the external sphincter causing voiding of urine.
Q.86 Trace the pathway for micturition reflex.
First phase:
| Receptors – stretch receptors in the wall of the urinary bladder. |
| Afferent fibers – pass through the pelvic nerve. |
| Center – sacral segments of the spinal cord. |
| Efferent fibers – pass through the pelvic nerve. |
| Response – the contraction of detrusor muscles and relaxation of the internal sphincter. |
Second phase:
When urine flows through the urethra, stretch receptors present in the urethra are stimulated and send impulses through afferent fibers of the pelvic nerve. These impulses inhibit the pudendal nerve resulting in the relaxation of the external sphincter and voiding of urine.
Q.87 What is dialysis?
Dialysis means the diffusion of solutes from an area of higher concentration to an area of lower concentration through a semipermeable membrane. And, this is the principle of the artificial kidney.
Q.88 What is dialysate?
Dialysate is the dialyzing fluid that is used in an artificial kidney. Through this fluid, the blood is purified during dialysis.
Q.89 What is the composition of dialysate?
The dialyzing fluid contains less quantity of sodium, potassium, and chloride than in the patient’s blood. It contains more quantity of glucose, bicarbonate, and calcium. It does not contain urea, uric acid, sulfate, phosphate, and creatinine.
Q.90 What are diuretics?
Diuretics are the substances that increase the urine output.
Q.91 What are the glands present in the skin?
- Sebaceous glands which secrete sebum
- Sweat glands that secrete sweat.
Q.92 What is the function of sebaceous glands?
Sebaceous glands secrete an oily substance called sebum that has antibacterial action, antifungal action, and protective function. Sebum also prevents heat loss.
Q.93 What are sweat glands? Name them.
Sweat glands are the skin glands, which secrete sweat. Sweat glands are of two types, eccrine glands and apocrine glands.
Q.94 What are the functional differences between eccrine and apocrine glands?
Eccrine glands function throughout life since birth and secrete clear watery sweat. These glands play a major role in temperature regulation. Apocrine glands start functioning only during puberty and secrete thick and milky sweat. These glands do not play any role in temperature regulation.
Q.95 Name the nerves supplying the sweat glands.
Eccrine glands are supplied by sympathetic cholinergic fibers whereas, apocrine glands are supplied by sympathetic adrenergic fibers.
Q.96 What is the normal body temperature? 37°C (98.6°F). Q.97 What is core temperature?
The average temperature in deeper tissues of the body is known as core temperature and it is always more than the oral or rectal temperature. It is about 37.8°C (100°F).
Q.98 What are the pathological variations of body temperature?
- Hyperthermia – abnormal increase in body temperature
- Hypothermia – decrease in body temperature.
Q.99 What is heat balance?
The difference between heat produced in the body and the heat lost from the body is called heat balance.
Q.100 How is heat produced in the body?
By:
- Metabolic activities
- Muscular activity
- The actions of hormones
- Radiation of heat from the environment
- Shivering.
Q.101 How is heat lost from the body?
By:
- Conduction
- Radiation
- Convection
- Evaporation
- Panting.
Q.102 Name the centers for temperature regulation in the hypothalamus.
- Heat loss center in the anterior hypothalamus
- Heat gain center in the posterior hypothalamus.
Q.103 How is loss of heat from the body increased?
By secretion of sweat due to peripheral vasodilatation.
Q.104 How is heat increased in the body?
By the prevention of heat loss and by increase in heat production.
Also read: Physiology Questions & Answers

Comments (0)