Eye: Vision
Special Sense (Viva)
Q.1 Define special senses.
The complex sensations are called special sensations or special senses.
Q.2 Name the special senses.
- Visual sensation
- Auditory sensation
- Gustatory or taste sensation
- Olfactory sensation or sensation of smell.
Q.3 What is the optic axis?
The line joining the anterior pole and posterior pole of the eyeball is called the optic axis.
Q.4 What is the visual axis?
The line joining a point in the cornea little medial to the anterior pole and fovea centralis (which is situated little lateral to the posterior pole) is known as the visual axis.
Q.5 What is the significance of the visual axis?
The significance of the visual axis is that the light rays from the object pass through this axis and reach the retina of the eye.
Q.6 What is conjunctiva? What are its parts?
Conjunctiva is a thin mucous membrane that covers the exposed part of the eye.
Its parts:
- Bulbar portion that covers the anterior surface of the eyeball
- Palpebral portion that covers the inner surface of eyelids.
Q.7 What is the lacrimal gland? Where is it situated?
Lacrimal gland is the glandular structure that secretes tears. It is situated in the bone that forms the upper and outer border of the eye socket.
Q.8 How is tear drained?
From the lacrimal gland, tear flows over the surface of the conjunctiva and drains into the nose via lacrimal ducts, lacrimal sac, and nasolacrimal duct.
Q.9 What are the layers of the wall of the eyeball?
- Outer layer or tunica externa or tunica fibrosa that includes cornea and sclera
- Middle layer or tunica media or tunica vasculosa that includes choroid, ciliary body, and iris
- Inner layer or tunica interna or tunica nervosa or retina.
Q.10 What is cornea?
The transparent structure that forms the anterior 1/6th of the outer layer of the eyeball is called the cornea.
Q.11 What is sclera?
Sclera is the posterior 5/6th of the outer layer of the eyeball.
Q.12 What is choroid? How is it formed?
Choroid is the posterior 1/6th of the middle layer of the eyeball. It is formed by capillary plexus, small arteries, and veins.
Q.13 What is the ciliary body?
Ciliary body is a ring-like structure formed by the anterior part of the middle layer of the eyeball.
Q.14 Name the parts of the ciliary body.
- Orbiculus ciliaris
- Ciliary body proper
- Ciliary processes.
Q.15 What is iris? And what is the pupil?
Iris is a circular diaphragm formed by anterior-most portion of the middle layer of the eyeball and it is placed in front of the lens. Pupil is the circular opening in the center of iris. The anterior and posterior chambers communicate through the pupil.
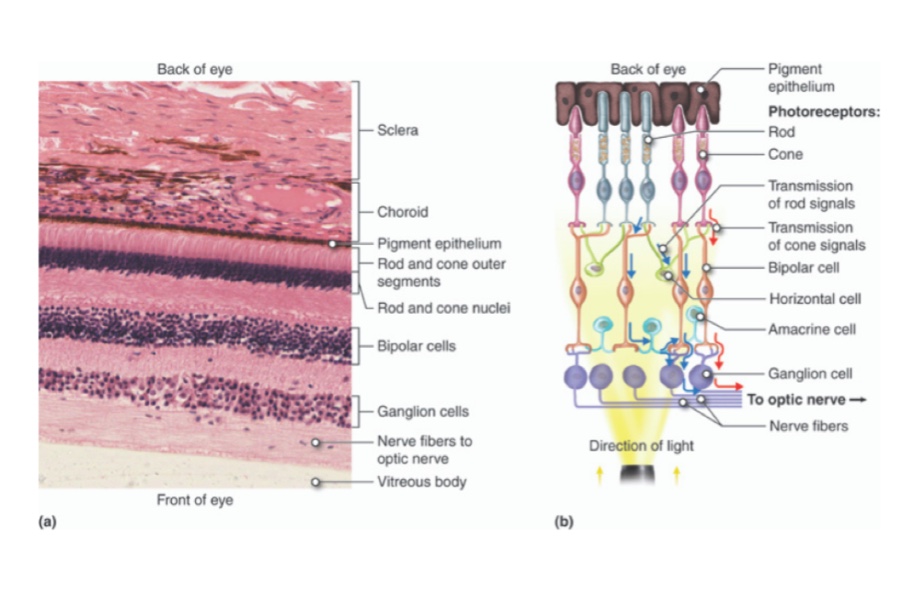
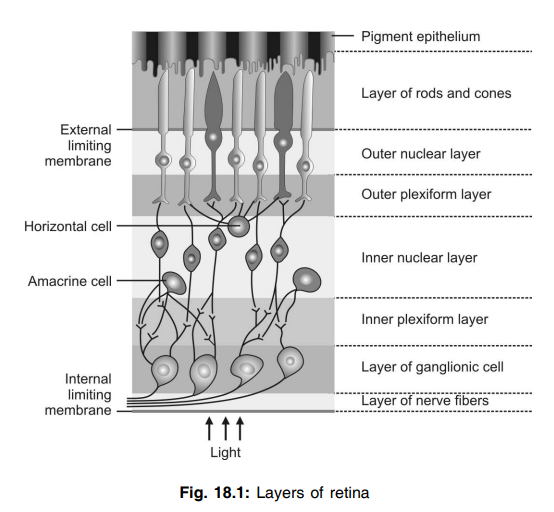
Q.16 What is retina? Name the layers of the retina.
Retina is the layer of the eyeball that forms the sensory part. It contains the receptors for vision.
Layers of retina
- Layer of pigment epithelium
- Layer of rods and cones
- External limiting membrane
- Outer nuclear layer
- Outer plexiform layer
- Inner nuclear layer
- Inner plexiform layer
- Ganglion cell layer
- Layer of nerve fibers
- Internal limiting membrane.
Q.17 What is fundus oculi? How is it examined?
The posterior part of the interior of the eyeball is known as fundus oculi or fundus. It is examined by using an ophthalmoscope.
Q.18 Name the important structures of fundus oculi.
- Optic disk
- Macula lutea.
Q.19 What is optic disk?
Optic disk is a pale disk-like structure situated near the center of the posterior wall of the eyeball. It is formed by the convergence of optic nerve fibers. It is also called a blind spot because it is insensitive to light since there are no rods and cones here.
Q.20 What is macula lutea?
Macula lutea is a yellow spot situated little lateral to the optic disk in the posterior wall of the eyeball. The yellow color is due to the presence of a yellow pigment. There is a small depression in the center of macula densa called fovea centralis.
Q.21 What is the importance of fovea centralis?
Fovea centralis is the region of acute vision because it contains only the cones.
Q.22 Name the intraocular fluids.
- Vitreous body
- Aqueous humor.
Q.23 What is the vitreous body? How is it formed?
A vitreous body is a gelatinous substance present in the space between the lens and retina. It is formed by a network of proteoglycan molecules.
Q.24 What is aqueous humor? How is it formed?
Aqueous humor is a thin fluid present in the space between lens and cornea. It is formed from plasma by diffusion, ultrafiltration and active transport of substances through epithelial cells lining the ciliary processes. After formation, aqueous humor reaches the posterior chamber by passing through suspensory ligaments. From here it reaches the anterior chamber via pupil.
Q.25 How is aqueous humor drained?
Aqueous humor is drained from anterior chamber into extraocular veins by passing through limbus (the angle between cornea and iris), the meshwork of trabeculae and canal of Schlemm.
Q.26 What is the physiological and clinical importance of canal of Schlemm?
Aqueous humor once formed from the ciliary process passes from the posterior chamber then via pupil enters into anterior chamber which then passes into the intrascleral venous plexus through canal of Schlemm, thereby this canal helps to drainage the aqueous humor continuously secreting from ciliary body. Blockade of the canal of Schlemm leads to increase intraocular pressure above 80 mm Hg resulting in pain and degeneration of blood vessels of retina and choroid. This condition is known as glaucoma.
Q.27 What are the functions of aqueous humor?
Aqueous humor:
- Maintains the shape of eyeball
- Maintains the intraocular pressure
- Provides nutrition, oxygen and electrolytes to avascular structures – lens and cornea.
Q.28 What is the normal intraocular pressure? How is it measured?
Normal intraocular pressure is 12 to 20 mm Hg. It is measured by tonometer.
Q.29 What are the changes taking place in lens during old age?
After 40 to 45 years of age, the lens looses its elastic property and presbyopia occurs. After 55 to 60 years, lens becomes opaque resulting in cataract.
Q.30 What is cataract?
Cataract is the opacity or cloudiness in natural lens of the eye.
Q.31 Name the ocular muscles.
- Superior rectus
- Inferior rectus
- Medial rectus
- Lateral rectus
- Superior oblique
- Inferior oblique.
Q.32 What are the nerves supplying ocular muscles?
- Oculomotor (III) nerve that supplies superior rectus, inferior rectus, medial rectus and inferior oblique muscle
- Trochlear (IV) nerve that supplies superior oblique muscle
- Abducent (VI) nerve that supplies lateral rectus muscle.
Q.33 What is the refractory power of cornea and lens?
Refractory power of cornea is 42 D (Diopter) and refractory power of lens is 23 D.
Q.34 What are the visual receptors? Explain their distribution briefly.
Visual receptors are rods and cones present in the retina of eyeball. In fovea centralis, only the cones are present. While proceeding from fovea towards periphery of retina, rods increase and cones decrease in number. At the periphery of retina, only rods are present.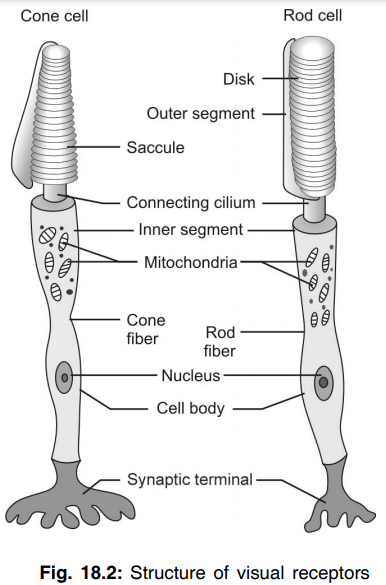
Q.35 What is the function of rods?
Rods have low threshold for light stimulus and are responsible for dim light vision or night vision or scotopic vision.
Q.36 What are the functions of cones?
Cones have high threshold for light stimulus and are responsible for bright vision or day light vision or photopic vision. Cones are also responsible for acuity of vision and color vision.
Q.37 What is rhodopsin?
Rhodopsin or visual purple is the photosensitive pigment present in the outer segment of rod cells.
Q.38. What is phototransduction?
Phototransduction or visual phototransduction is the process by which the light stimulus causes development of receptor potential in the visual receptors.
Q.39 What is the difference between the resting membrane potential in visual receptors and other cells of the body?
Resting membrane potential in visual receptors is very less and it is only about – 40 mV whereas in other cells of the body it is – 70 to – 90 mV.
Q.40 What is the difference between the receptor potential in rod cells and other sensory receptors?
Usually, the receptor potential is in the form of depolarization in the sensory receptors. But, in rod cells, it is in the form of hyperpolarization, i.e. the negativity increases to about – 70 to – 80 mV.
Q.41 What are the photosensitive pigments present in cone cells?
Porpyropsin, iodopsin and cyanopsin.
Q.42 What is dark adaptation? What are its causes?
When a person enters a room with dim light after spending long time in a bright light area, he cannot see any object in the beginning. After about 20 minutes time, he starts seeing the object. This process is called dark adaptation.
Causes:
- Increase in the sensitivity of rods due to resynthesis of rhodopsin
- Dilatation of pupil.
Q.43 What is light adaptation? What are its causes?
When a person enters a bright light area from a dim light area, he feels discomfort for some time due to dazzling effect of bright light. After about 5 minutes, he is able to see the objects without discomfort. This process is called light adaptation.
Causes:
- Reduction in the sensitivity of rods due to breakdown of rhodopsin
- Constriction of pupil.
Q.44 Define electroretinogram (ERG).
Electroretinogram (ERG) is the record of electrical activity produced in retina when it is stimulated by the light rays.
Q.45 Define acuity of vision.
Ability of the eye to determine the precise shape and details of any object is called acuity of vision or visual acuity.
Q.46 Name the receptors responsible for acuity of vision.
Cones are responsible for acuity of vision.
Q.47 How is acuity of vision tested?
For distant vision : By using Snellen’s chart
For near vision : By using Jaeger’s chart.
Q.48 Define field of vision.
Part of external world seen by one eye when it is fixed in one direction is known as field of vision.
Q.49 What is binocular vision?
In man and some animals in whom the eyeballs are situated in front of head, the visual fields of both eyes overlap, i.e. a portion of external world is seen by both eyes. This is known as binocular vision.
Q.50 What is monocular vision?
In some animals like horse in whom the eyeballs are situated at the sides of head, the visual fields of both eyes overlap only to a very small extent, i.e. different portions of external world is seen by each eye. This is known as monocular vision.
Q.51 What are the divisions of visual field?
- Temporal field that extends to about 100° laterally
- Nasal field that extends to about 60° medially
- Upper field that extends to about 60° above i
- Lower field that extends to about 75° below.
Q.52 What are corresponding retinal points?
While looking at an object, the points of retina of both eyes on which the light rays from the object fall are called corresponding retinal points.
Q.53 What is diplopia? How does it occur?
Diplopia means double vision. While looking at an object, if the eyeballs are directed in such a way that the light rays do not fall upon the corresponding point of retina of both eyes, a double vision or diplopia occurs i.e., one single object is seen as double.
Q.54 What are the causes for permanent and temporary diplopia?
Permanent diplopia is caused by paralysis or weakness of ocular muscles. Temporary diplopia occurs due to imbalanced actions of ocular muscles in conditions like alcoholic intoxication.
Q.55 What is a blind spot?
The optic disk is called a blind spot. While looking at an object, if the image of the object falls upon the optic disk, the object cannot be seen because the visual receptors are absent in the optic disk. So, this part of the retina is called the blind spot.
Q.56. How is visual field determined?
By:
- Using perimeter
- Using Bjerrum’s screen
- Confrontation test.
Q.57 What is photopic, scotopic and mesopic vision?
- Photopic—It is daylight vision due to cone receptor.
- Scotopic—It is dim light vision and a function of rods.
- Mesopic—It is a full moon night vision where reading becomes difficult.
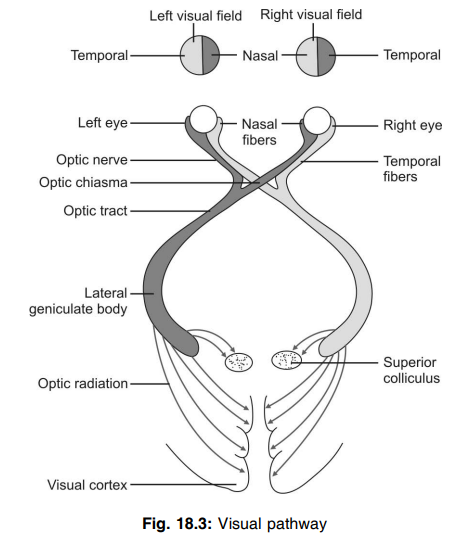
Q.58 Trace the pathway for visual sensation.
Visual pathway includes:
- Receptors – rods and cones
- First order neurons – bipolar cells in retina
- Second order neurons – ganglionic cells in retina
- Optic nerve – formed by axons of ganglionic cells
- Optic chiasma – crossing of medial fibers of optic nerve
- Optic tract – formed by crossed and uncrossed fibers of the optic nerve
- Third order neurons – lateral geniculate body
- Optic radiation
- Visual cortex
Q.59 Where is the cen ter for vision?
The Center for vision is in the visual cortex that is situated in a calcarine fissure in the medial surface of the occipital lobe.
Q.60 What are the areas of the visual cortex?
- Primary visual area – area 17
- Visual association area – area 18
- Occipital eye field – area 19
Q.61 What are the functions of areas of the visual cortex?
Primary visual area (area 17) is concerned with the perception of visual impulses.
Visual association area (area 18) is responsible for the interpretation of visual impulses.
Occipital eye field (area 19) is concerned with the movements of eyeballs.
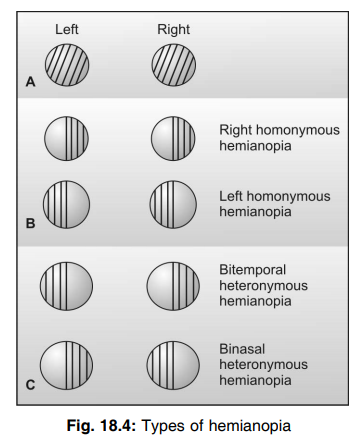
Q.62 Define the term anopia, homonymous hemianopia, heteronymous hemianopia, scotoma.
- Anopia—It is the complete loss of visual field in an eye
- Hemianopia—Refers to the blindness of half of the visual field
- Homonymous hemianopia—It refers to the loss of field of vision of the same halves in two eyes.
- Heteronymous hemianopia—When different halves of the field of vision in two eye are lost
- Scotoma—Loss of vision in an eye which is confined to the center of the visual field.
Q.63 Name the effects of lesion at different levels of the visual pathways.
- Lesion in optic nerve – total blindness
- Lesion in lateral fibers of optic chiasma on one side – nasal hemianopia
- Lesion in lateral fibers of both the sides of optic chiasma – binasal hemianopia
- Lesion in medial fibers of optic chiasma – bitemporal hemianopia
- Lesion in the left optic tract, left lateral geniculate body, left optic radiation or left visual cortex – right homonymous hemianopia
- Lesion in the right optic tract, right lateral geniculate body, right optic radiation, or right visual cortex – left homonymous hemianopia.
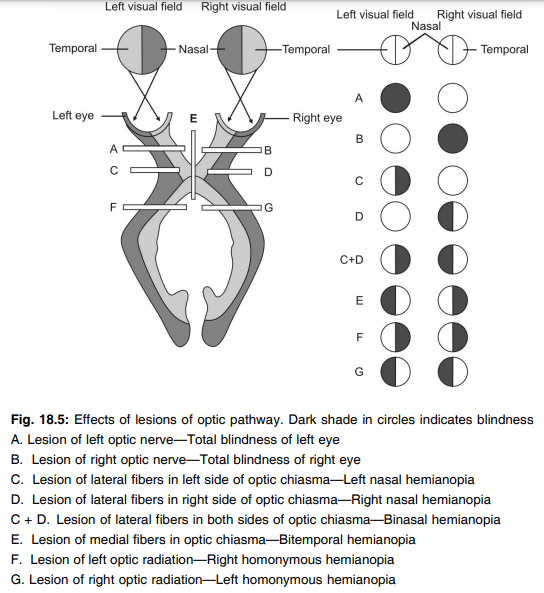
Q.64 What is macula sparing?
In homonymous hemianopia, the macular vision is not affected in spite of lesion in the visual cortex. This is called macula sparing. This is because the optic fibers from each eye are projected to the visual cortex of both sides.
Q.65 Define pupillary reflexes. Name them.
Pupillary reflexes are the reflexes, which cause the alteration in the diameter of pupil.
Pupillary reflexes:
- Light reflex
- Ciliospinal reflex
- Accommodation reflex.
Q.66 Define and classify light reflex.
Light reflex is the reflex in which, the flash of light into the eye causes constriction of pupil.
Light reflex is classified into two types:
- Direct light reflex in which, the flash of light in one eye causes constriction of pupil in the same eye
- Indirect or consensual light reflex in which the flash of light in one eye causes constriction of pupil in the same eye as well as in the opposite eye.
Q.67 What is Wernicke pupillary reflex?
In case of partial damage of light reflex fibers, when light is focused on the blind part of retina light reflex is lost and if light is focused on the sound retinal part light reflex persists. This reflex is known as Wernicke pupillary reflex.
Q.68 Trace the pathway for light reflex.
Pathway for light reflex includes:
- Afferent fibers – fibers from optic pathway ending in pretectal nucleus of midbrain
- Center – pretectal nucleus
- Efferent fibers – fibers from pretectal nucleus reach Edinger-Westphal nucleus of III cranial nerve. The fibers from this go to ciliary ganglion. Short ciliary nerves arising from this supply constrictor pupillae muscles of iris.
Q.69 What is ciliospinal reflex?
Stimulation of skin over the neck causes dilatation of the pupil. This is known as a ciliospinal reflex.
Q.70 What is the nerve supply to the muscles of the iris?
Constrictor pupillae muscle of the iris is supplied by parasympathetic nerve fibers from the Edinger-Westphal nucleus of III cranial nerve. Dilator pupillae muscle is supplied by sympathetic fibers.
Q.71 Define accommodation of eyeball.
Accommodation is the adjustments made in eyeballs while looking at near object.
Q.72 What is Argyll Robertson pupil and reverse Argyll Robertson pupil?
In the case of lesion in the aqueduct and superior colliculi, there is a loss of light reflex keeping the convergence accommodation reflex intact. This type of pupil is referred to as the Argyll Robertson pupil. Where as due to the lesion in the frontal lobe (bilaterally) or damage of its descending fibers to III nerve nucleus pupillary constriction in response to light is present but accommodation is lost. This is known as reverse Argyll Robertson pupil.
Q.73 What are the adjustments made in eyeballs during accommodation?
- Convergence of eyeballs – due to contraction of medial recti
- Constriction of pupil – due to contraction of constrictor pupillae
- Increase in the anterior curvature of the lens – due to contraction of the ciliary muscle.
Q.74 What is Young-Helmholtz theory of accommodation?
It describes how the curvature of the lens increases during accommodation.
Q.75 Explain briefly the mechanism of increase in the anterior curvature of the lens during accommodation.
During distant vision, the lens is flat due to the traction by suspensory ligaments. During near vision, ciliary muscle contracts and draws the choroid forward. So the ciliary processes are brought closer to the lens and the suspensory ligaments are slackened. Now, the tension on the lens is released. Due to the elastic property, the lens bulges forward so that the anterior curvature of the lens increases.
Q.76 What are Purkinje-Sanson images?
Purkinje-Sanson images are the images of the flame of a lighted candle held in front of the eye. These images are used to demonstrate the increase in the anterior curvature of the lens during accommodation.
Q.77 Trace the pathway for accommodation.
Pathway for accommodation includes:
- Afferent fibers – visual fibers from the retina to the visual cortex in the occipital lobe and the association fibers from there to the frontal eye field (area 8) in the frontal lobe.
- Center – frontal eye field
- Efferent fibers – fibers from frontal eye field to Edinger–Westphal nucleus of III cranial nerve. Fibers from this nucleus reach ciliary ganglion. Nerve fibers from this pass-through short ciliary nerves and supply constrictor pupillae. Some fibers from the frontal eye field reach the somatic motor nucleus of III cranial nerve and fibers from this supply the medial recti.
Q.78 What are the spectral colors? Name them.
Colors forming the spectrum are called spectral colors. Spectral colors are violet, indigo, blue, green, yellow, orange, and red (VIBGYOR).
Q.79 What are the primary colors? Name them.
Primary colors are those, which can produce white when combined together. The primary colors are red, green, and blue.
Q.80 What are the complementary colors? Give examples.
When two colors are mixed or combined in the right proposition, white is produced. Such two colors are called complementary colors.
Examples:
- Red and greenish-blue
- Orange and cyan blue
- Purple and green
Q.81 Name the theories of color vision.
- Thomas Young’s trichromatic theory
- Helmholtz trichromatic theory
- Granit’s modulator and dominator theory
- Hartridge’s polychromatic theory
- Hering’s theory of opposite colors.
Q.82 Define and classify the color blindness.
Failure to appreciate one or more color is known as color blindness.
Color blindness is classified into three types:
I) Monochromatism,
ii) Dichromatism,
iii) Trichromatism.
Q.83 What is monochromatism? What are its types?
Monochromatism is the condition in which the subject cannot appreciate any color and the whole spectrum is seen in different shades of gray.
It is divided into two types:
- Rod monochromatism
- Cone monochromatism.
Q.84 What is dichromatism? What are its types?
Dichromatism is the condition when only two of the three primary colors are appreciated. It is of three types:
- Protanopia in which the first primary color, red cannot be appreciated
- Deuteranopia in which green cannot be appreciated
- Tritanopia in which blue cannot be appreciated.
Q.85 What is trichromatism? What are its types?
Trichromatism is the condition in which all the three primary colors are appreciated but the perception of one of the colors is very weak.
It is divided into three types:
- Protanomaly in which perception of red color is weak
- Deuteranomaly in which perception of green is less
- Tritanomaly in which perception of blue is less.
Q.86 How is color blindness determined?
By using:
- Ishihara’s color charts,
- Colored wool,
- Edridge-Green lantern.
Q.87 Name the errors of refraction.
The errors of refraction are :
- Myopia
- Hypermetropia
- Anisometropia
- Astigmatism
- Presbyopia
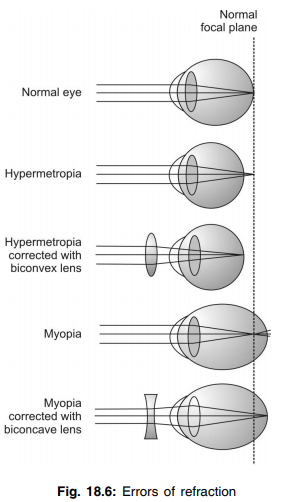
Q.88 Define emmetropia.
Emmetropia is the condition with normal refractory power of the eye.
Q.89 Define ametropia. What are its types?
Any deviation in the refractory power of the eye from normal condition is known as ametropia.
It is of two types:
- Myopia
- Hypermetropia.
Q.90 What is myopia or short-sightedness? What is its cause?
Myopia or short-sightedness is the condition in which the near vision is normal but the distant vision is defective. It is caused by an increase in the anteroposterior diameter of the eyeball. So, the image from distant objects is brought to a focus in front of the retina.
Q.91 How is myopia corrected?
By using a concave lens.
Q.92 What is hypermetropia or long-sightedness? What is its cause?
Hypermetropia or long-sightedness is the condition in which distant vision is normal but the near vision is affected. It is caused by the decrease in the anteroposterior diameter of the eyeball. So, the light rays are brought to a focus behind the retina.
Q.93 How is hypermetropia corrected?
By using a convex lens.
Q.94 What is anisometropia?
Anisometropia is the condition in which the refractory power of both the eyes are not the same.
Q.95 Define astigmatism. What is its cause?
Astigmatism is the defect in which the light rays are not brought to a sharp point upon the retina. It is caused by irregularity in the curvature of the lens and unequal refractory power of the lens in different meridians.
Q.96. What are the types of astigmatism?
Regular astigmatism:
In this, the refractory power is unequal in different meridians but, in one single meridian, it is uniform throughout
Irregular astigmatism:
In this, the refractory power is unequal not only in different meridians but also in different points of the same meridian.
Q.97 How is astigmatism corrected?
By using a cylindrical lens.
Q.98 What is presbyopia?
In old age, the amplitude of accommodation reduces and the near object cannot be seen clearly. Thus, the inability to see the near objects in old age is known as presbyopia.
Q.99 What are the causes for presbyopia?
- Decreased elasticity of lens that prevents the increase in the anterior curvature during near vision
- Decreased convergence of eyeballs due to weakness of ocular muscles.
Q.100 How is presbyopia corrected?
By using a convex lens.
EAR
Q.101 Name the parts of the ear.
- External ear
- Middle ear
- Internal ear.
Q.102 What is tympanic membrane?
The tympanic membrane is a semitransparent structure that separates the middle ear from the external auditory meatus.
Q.103 Define auditory ossicles. Name them.
Auditory ossicles are the miniature bones arranged in the middle ear in the form of a chain from the tympanic membrane to the oval window.
The auditory ossicles are:
- Malleus
- Incus
- Stapes
Q.104 What are the skeletal muscles attached to auditory ossicles?
Tensor tympani and stapedius.
Q.105 What is tympanic reflex? What is its significance?
The tympanic reflex is a reflex action in which loud sound causes contraction of muscles of the middle ear, tensor tympani and stapedius.
Significance:
- The tympanic reflex prevents rupture of the tympanic membrane by loud noise
- It also prevents fixation of footplate of stapes against oval window during exposure to loud noise
- It also protects the cochlea from loud noise.
Q.106 What is an auditory tube or Eustachian tube? What is its function?
The auditory tube or Eustachian tube is the flattened canal that connects the middle ear with the nasopharynx.
It is responsible for the equalization of pressure on either side of the tympanic membrane.
Q.107 Name the sense organs present in the internal ear or labyrinth.
- Cochlea for hearing
- Vestibular apparatus for equilibrium.
Q.108 What are the compartments of cochlea?
- Scala vestibuli
- Scala media or cochlear duct
- Scala tympani.
Q.109 What are the membranes, which divide cochlea into three compartments?
- Vestibular membrane or Reissner’s membrane that separates scala vestibuli and scala media
- Basilar membrane that separates scala media and scala tympani.
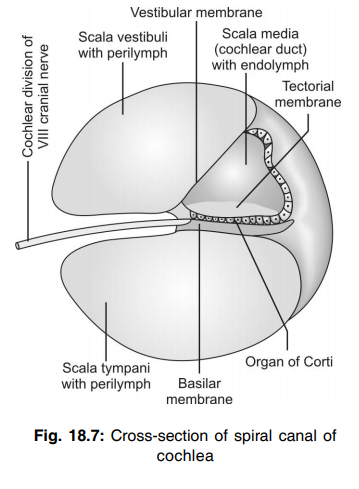
Q.110 Name the fluids present in the cochlea.
- Perilymph in scala vestibuli and scala tympani
- Endolymph in scala media.
Q.111 What is helicotrema?
Helicotrema is a small canal that connects the scala vestibuli and scala tympani at the apex of the cochlea.
Q.112 What is ductus reunions?
Ductus reunions is a slender canal that connects scala media with the saccule of the vestibular apparatus.
Q.113 What is the organ of Corti?
Organ of Corti is the sensory part of the cochlea situated in the upper surface of the basilar membrane.
Q.114 What is the Eustachian tube and what is its importance?
It connects the middle ear cavity with the pharynx. Normally its pharyngeal opening is closed but opens during the act of swallowing, chewing, or yawning and thereby helps the air to enter into middle ear. Therefore it serves to equalize the pressure on the two sides of tympanic membrane when atmospheric pressure changes.
Q.115 Why does there is pain in the ear and even loss of hearing in sore throat?
Due to infection during sore throat, there is an inflammation occurring in the pharynx causing closure of the pharyngotympanic tube. Thus middle ear cavity becomes a closed cavity due to the inability to open the eustachian tube. When the air within the middle ear gets absorbed, its pressure decreases resulting in inward bulging of the tympanic membrane that causes pain sensation, and in severe cases, there may be a rupture of the tympanic membrane resulting in loss of hearing.
Q.116 Name the receptor cells of the organ of Corti.
Inner and outer hair cells.
Q.117 What is the tectorial membrane? What is its function?
The tectorial membrane is the membrane present at the roof of the organ of Corti and it is in contact with the processes of hair cells of the organ of Corti. When sound waves reach the inner ear, the endolymph in scala media vibrates. This causes movements of the tectorial membrane. The movements of the tectorial membrane stimulate the hair cells.
Q.118 What are the divisions of the vestibulocochlear nerve (VIII cranial nerve)?
- Vestibular division that supplies the vestibular apparatus
- Cochlear division that supplies the cochlea.
Q.119 Trace the auditory pathway
The auditory pathway includes:
- Receptors – hair cells in the organ of Corti
- First order neurons – neurons in spiral ganglia Axons of these neurons form cochlear nerve
- Second order neurons – cells in ventral and dorsal cochlear nucleus
- Third order neurons – cells in superior olivary nucleus and nucleus of the lateral lemniscus
- Subcortical center – medial geniculate body of the thalamus
- Cortical centers – in the auditory cortex in the temporal lobe of the cerebral cortex.
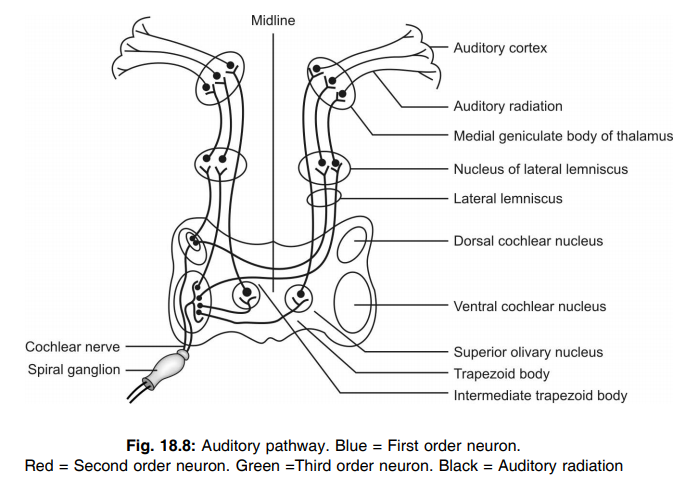
Q.120 What are the cortical areas for auditory sensation?
- Primary auditory areas – areas 41 and 42
- Wernicke’s area
- Auditopsychic area – area 22.
Q.121 What are the functions of cortical areas for auditory sensation?
Primary auditory areas (areas 41 and 42) are concerned with the perception of auditory impulses. Wernicke’s area and auditopsychic area (area 22) are concerned with the analysis and interpretation of auditory impulses.
Q.122 What is the role of external ear in hearing?
External ear directs the sound waves towards the tympanic membrane.
Q.123 What is role of middle ear in hearing?
The role of the middle ear in hearing is to conduct the sound waves. When sound waves reach the tympanic membrane, it vibrates. The vibrations from the tympanic membrane are transmitted by auditory ossicles in the middle ear to the perilymph of the internal ear through an oval window.
Q.124 What is sound impedance? How is impedance offered in the ear?
Impedance means obstruction or opposition to the passage of sound waves. In the ear, impedance is offered by the perilymph present in cochlea.
Q.125 What is impedance matching?
Impedance matching is the mechanism by which the sound impedance offered by the perilymph in the cochlea is decreased. This is done by the tympanic membrane and the lever system of auditory ossicles. These two factors convert the sound energy into mechanical vibration in the fluid of internal ear, which helps to overcome the impedance.
Q.126 Name the types of conduction of sound waves in the ear.
- Ossicular conduction
- Bone conduction
- Air conduction.
Q.127 What is traveling wave?
The vibrations from tympanic membrane reach the oval window and cause movement of fluid in scala vestibuli, scala media and scala tympani. The movement of fluid in scala tympani initiates a wave in basilar membrane near round window. This wave travels through basilar membrane towards the apex of cochlea. This wave is called traveling wave.
Q.128 What is the significance of traveling wave?
It produces the vibration in the basilar membrane, which in turn, causes stimulation of hair cells in the organ of Corti.
Q.129 Name the electrical potentials involved during the process of hearing.
- Receptor potential or cochlear microphonic potential
- Endocochlear potential or endolymphatic potential
- Action potential in auditory nerve fibers.
Q.130 What is cochlear microphonic potential or cochlear receptor potential?
The slight depolarization that develops in the hair cells of organ of Corti when stimulated is known as cochlear microphonic potential or cochlear receptor potential. The resting membrane potential in these cells is – 60 mV. When stimulated, it comes down to about – 50 mV causing the slight depolarization.
Q.131 What are the properties of cochlear microphonic potential?
It is:
- Monophasic
- Non-propagative.
Q.132 What is the significance of cochlear microphonic potential?
Cochlear microphonic potential causes generation of action potential in auditory nerve fiber.
Q.133 What is endocochlear or endolymphatic potential? What is its significance?
An electrical potential exists between endolymph and perilymph with endolymph having a potential of + 80 mV. This is known as endocochlear or endolymphatic potential. It increases the excitability and response of hair cells.
Q.134 What are the theories of hearing?
- Theories of the first group, according to which the analysis of pitch of the sound is the function of the cerebral cortex: – Telephone theory of Rutherford – Volley theory.
- Theories of second group, according to which the analysis of pitch of the sound is the function of cochlea: – Resonance theory of Helmholtz – Place theory – Traveling theory.
Q.135 Name the auditory defects or deafness.
- Conduction deafness
- Nervous deafness.
Q.136 What is conduction deafness? What are its causes?
Deafness due to the defect in conduction of sound in the external ear and/or middle ear is known as conduction deafness.
Causes:
- Obstruction of external auditory meatus by wax
- Thickening of the eardrum by repeated middle ear infection
- Perforation of eardrum by unequal pressure on either side i
- Otosclerosis – the fixation of footplate of stapes against oval window.
Q.137 What is nervous deafness?
Deafness due to damage of any structure in cochlea or lesion in auditory pathway is known as nervous deafness.
Q.138 Name the tests for hearing.
- Rinne’s test
- Weber’s test
- Audiometry
Q.139 What is the frequency of tuning fork that is used for hearing tests?
512 cycles/second.
Q.140 Which type of conduction is better in persons with normal hearing?
In persons with normal hearing, air conduction is better than bone conduction.
Q.141 Which type of conduction is better in conduction deafness?
In conduction deafness, bone conduction is better than air conduction.
Q.142 What does happen to conduction of sound in nerve deafness?
In nerve deafness, both air conduction and bone conduction are reduced or lost.
Q.143 What is audiometry?
Audiometry is a technique used to determine the nature and extent of auditory defects.
TASTE:
Q.144 Name the sense organs for taste or gustatory sensation.
Taste buds are the sense organs for taste sensation.
Q.145 Where are the taste buds situated?
Taste buds are situated on the papillae of tongue and in the mucosa of epiglottis, palate, larynx and proximal part of esophagus.
Q.146 What are the types of papillae on the tongue?
- Filiform papillae situated over the dorsum of tongue
- Fungiform papillae situated over the anterior surface of the tongue near the tip
- Circumvallate papillae arranged in the shape of ‘V’ over the posterior part of tongue.
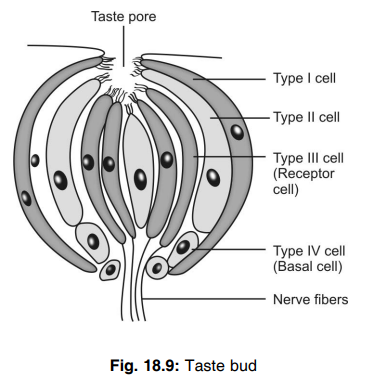
Q.147 Name the types of cells present in the taste buds. Which are the receptor cells?
The types of cells present in taste buds are
- Type I cells or sustentacular cells
- Type II cells
- Type III cells
- Type IV cells or border cells Type III cells are the receptor cells in taste bud.
Q.148 Trace the pathway for taste sensation. Pathway for taste sensation includes:
- Receptors – receptor cells in taste buds
- First order neurons – neurons in the nuclei of the cranial nerves namely, facial nerve, glossopharyngeal nerve, and vagus nerve
- Second order neurons – neurons in the nucleus tractus solitarius
- Third order neurons – neurons in the posteroventral nucleus of thalamus
- Taste center – opercular area of cerebral cortex.
Q.149 Name the nerves carrying taste sensation.
- Chorda tympani branch of facial nerve carries taste sensation from anterior two thirds of tongue
- Glossopharyngeal nerve carries taste sensation from posterior two thirds of tongue
- Vagus nerve carries taste sensation from other areas.
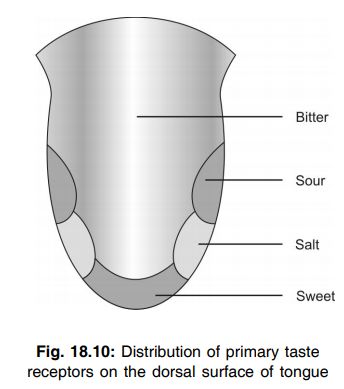
Q.150 Name the primary taste sensations.
- Sweet
- Salt
- Sour
- Bitter
Q.151 Name the chemical substances producing taste sensation.
Sweat taste:
Organic substances like monosaccharides, polysaccharides, glycerol, alcohols, aldehydes, ketones and chloroform and inorganic substances like lead and beryllium.
Salt taste:
Chlorides of sodium, potassium and ammonium, nitrates of sodium and potassium and some sulfates, bromides and iodides.
Sour taste:
Hydrogen ions in acids and acid salts.
Bitter taste:
Organic substances like quinine, strychnine, morphine, glucosides, picric acid and bile salts and inorganic substances like salts of calcium, magnesium and ammonium. Bitter taste is mainly due to cations.
Q.152 Name the taste sensations having very low threshold value and very high threshold.
Bitter taste has a very low threshold (quinine in 1 in 2,000,000 dilution) value and sweet taste has a very high threshold (sugar in 1 in 200 dilution) value.
Q.153 What is ageusia? What are its causes?
Loss of taste sensation is known as ageusia. Aqeusia in anterior two thirds of the tongue is caused by lesion in facial nerve, chorda tympani or mandibular division of trigeminal nerve. Aqeusia in anterior one thirds of tongue is caused by lesion in glossopharyngeal nerve.
Q.154 What is hypogeusia?
Decrease in taste sensation is called hypogeusia.
Q.155 What are the receptors for sensation of smell or olfactory sensation?
Receptors for sensation of smell or olfactory sensation are the expanded end of dendrite of bipolar neurons situated in olfactory mucus membrane.
Q.156 Trace the pathway for olfactory sensation.
Receptors are the ending of dendrite of bipolar cells in olfactory mucus membrane. Axons of these cells synapse with dendrites of mitral cells, which form the olfactory glomeruli in olfactory bulb. Axons from olfactory bulb form olfactory tract that terminates in the center situated in olfactory cortex. Olfactory cortex includes the structures of limbic system namely, olfactory nucleus, prepyriform cortex, olfactory tubercle and amygdala.
Q.157 What are the different types of odor? Give examples.
- Aromatic or resinous odor – camphor, lavender, clove and bitter almond
- Ambrosia odor – musk.
- Burning odor – burning feathers, tobacco, roasted coffee and meat
- Ethereal odor – fruits, ethers and bees wax
- Fragrant or balsamic odor – flowers and perfumes
- Garlic odor – garlic, onion and sulfur
- Goat odor – caproic acid and sweet cheese
- Nauseating odor – decayed vegetables and feces.
- Repulsive odor – bed bug.
Q.158 What is anosmia?
Loss of sensation of smell is known as anosmia.
Q.159 What is hyposmia? What is its common cause?
Reduction in olfactory sensation is called hyposmia. Its common cause is the constant exposure to a particular odor like that of perfume that is often used in excess.
Q.160 What is hyperosmia?
Increased olfactory sensation is called hyperosmia.
Also read: Physiology Questions & Answers

Comments (0)