Important for viva
Q.1 Which blood is generally used in hematological practical–Capillary blood or Venous blood?
Capillary blood
Q.2 What is the difference between capillary blood and venous blood?
Capillary blood is obtained from punctured capillaries, smallest arterioles or venules by a skin puncture usually over a finger or ear lobe or the heel of the foot (in infants) and shows lower cell counts, lower hemoglobin concentration, and PCV values as some tissue fluid always dilute the blood, whereas the venous blood is obtained from a superficial vein by venopuncture which shows comparatively higher cell counts, higher Hb percentage and PCV values as it is not contaminated with tissue fluid.
Q.3 Why the capillary blood is called peripheral blood?
Capillary blood is called as peripheral blood as it comes from the peripheral blood vessels like venules or smallest arterioles or capillaries in contrast to venous blood.
Q.4 Why the thumb or little finger is not pricked for collecting blood?
It is because the underlying palmar fascia from these digits extends up to the forearm. So in case of any infection at the site of injury, there is a chance of the infection to spread up to the forearm.
Q.5 In the case of infants, from where is the capillary blood collected?
It is collected from either big toe or heel as the fingers are too small.
Q.6 What measures will you take to prevent the spreading of hepatitis infection following the pricking of fingers?
The needle used to prick the finger should be heated over flame.
Q.7 Why should the pricked finger not to be squeezed?
Squeezing the finger results in coming out of the tissue fluid that dilutes the capillary blood and thus giving lower values.
Q.8 What are the features of ideal blood film?
These are:
- It should be tongue-shaped, uniformly thick, neither too thick nor too thin, and should occupy the middle 2/3rd of the slide.
- Microscopically all the cells should be separate without any overcrowding and rouleaux formation.
Q.9 What is the composition of Leishman stain? What are the function of each constituent and why the stain should be acetone-free?
The composition and function of each constituent is:
- Leishman powder: 0.15 gm
– Eosin: An acidic dye stains the basic part of cell e.g.; cytoplasm
– Methylene blue: A basic dye stains acid part of the cell e.g. nucleus - Methyl alcohol (Acetone Free): 100 ml (as a fixative and solvent)
Acetone free methyl alcohol is used because the acetone being a strong lipid solvent can even destroy the cell by lysing the cell membrane.
Q.10 Why buffer solution is used instead of distilled water in Leishman’s staining?
The pH of the buffer solution is adjusted at 6.8 and at this particular pH the ionization of stain is optimum, so the stain particles can easily penetrate the cell to stain it.
Q.11 Why is Leishman’s stain diluted after 1-2 min?
During the initial 1-2 min, staining does not take place, as the stain particles cannot enter the cell as long as they are not ionized by the addition of water. During this period the absolute alcohol of Leishman’s stain serves two functions:
- Fixes the blood cells on the glass by precipitating the plasma proteins, which act as glue.
- Preserves the normal shape and chemistry of cells.
Q.12 Can tap water be used for diluting the stain after fixation?
It should not be used as methylene blue of Leishman’s stain may be unable to stain the cells because of improper pH.
Q.13 Name any other stain that can be used to stain the blood film.
Geimsa’s stain
Q.14 What do you mean by ‘Vital Staining’?
It is the special staining method to stain the living cells.
Q.15 Why is cedarwood oil required to use oil immersion lens?
It is because the refractive index of this oil is similar to that of glass avoiding the refraction of the light. Otherwise, the image will be faint and blurred.
Q.16 Which part of the blood film should be avoided for counting the cells?
“Head’ and extreme “Tail” part of the slide as the cells present in these areas are few in number and also distorted.
Q.17 How do you differentiate between RBC pipette and WBC pipette?
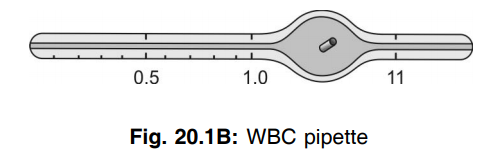
| Parameter | RBC pipette | WBC pipette |
| Upper gradation | 101 | 11 |
| Diameter of bulb | More | Less |
| Color of mouthpiece | Red | White |
| Color of bead in the bulb | Red | White |
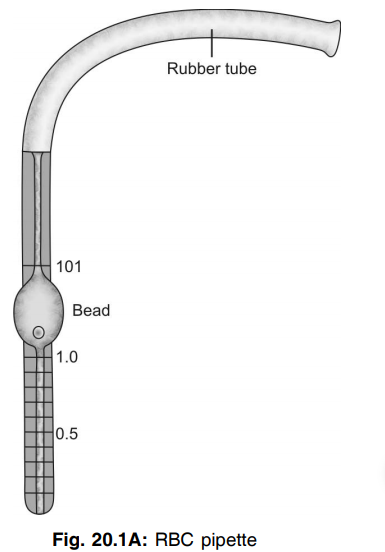
Q.18 What are the functions of the bulb in a diluting pipette?
It helps the blood to be diluted and also to be mixed with the diluting fluid.
Q.19 What are the functions of the bead present inside the bulb of the diluting pipette?
It:
- Helps to mix the blood with the diluting fluid.
- Helps to identify the pipette by just glancing it.
- Gives an idea of whether the pipette is wet or dry. If it is dry the bead rolls freely inside the bulb.
Q.20 Why it is important to discard the first two drops of diluted blood from the pipette before charging the counting chamber?
The stem of the pipette contains only the cell-free diluent which is to be discarded before charging the chamber; otherwise, the count will be low and thus erroneous.
Q.21 Why any small excess of blood drawn into the pipette should not be removed by a piece of cotton?
If the cotton is used to remove the excess blood drawn in the pipette then it will absorb only the fluid, not the cells. This will result in higher RBC/WBC count than the actual value.
Q.22 How will you clean the pipette in case of clotting of the blood inside the stem of the pipette?
It is to be kept in strong nitric acid or alkali or H2O2 for 24 hrs and then washed in the running tap water. A flexible suitably thick metal wire is now inserted to clean the capillary bore, finally rinse with alcohol or ether to dry it.
Q.23 How will you clean the pipette?
It is by sucking up and blowing out distilled water several times followed by sucking up and blowing out acetone for drying it.
Q.24 How will you clean the chamber and coverslip?
It is by washing it first with soap and water and then with alcohol.
Q.25 Can these pipettes be used for any other purpose?
The RBC pipette can be used for counting platelets, WBCs (when their count is very high as in leukemia), and also for counting the spermatozoa in the semen.
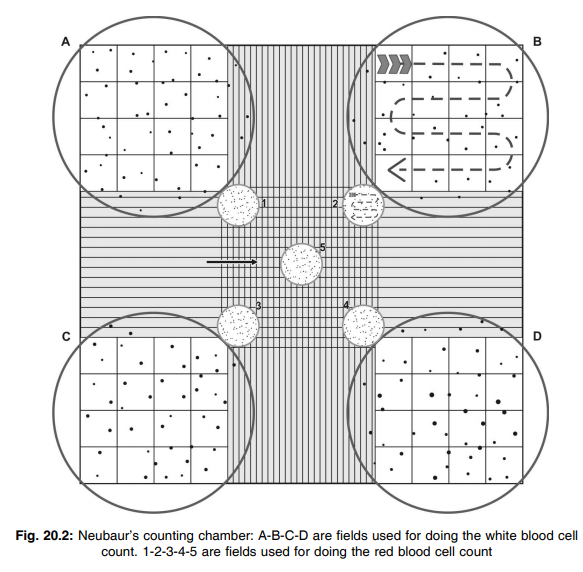
Q.26 What is a Neubauer’s counting chamber?
Neubauer’s double-counting chamber is a thick rectangular glass with a polished transverse bar in the center, separated from the rest of the slide by two parallel grooves on either side. The polished bar is divided into two equal platforms by a groove in the middle resulting in ‘H’ shaped depression. The surface of the platforms is 1/10 mm below the surface of the rest of the slide. So if a cover glass is placed over the surface of the counting chamber, the under surface of the coverglass remains 1/10 mm above the polished surface of the platform. The counting area is in the form of a central ruled area on the polished surface of each platform. It is a square, with each side measuring 3 mm. This square is divided into 9 equal squares, each having a side of 1 mm. Of these, the four corner squares are used for WBC counting. The central 1 mm square is divided into 25 equal small squares of 1/5 mm side, by means of triple lines of which the 4 corner ones and the central one are used for RBC counting. Each of these squares is subdivided into 16 smallest squares each of 1/20 mm side.
Q.27 Describe the procedure of filling the pipette for doing RBC/ WBC count.
The right type of pipette must be chosen, WBC pipette or the RBC pipette. The correct type of diluting fluid must be then selected (Turk’s fluid for WBC count and Hayem’s fluid for the RBC count). The blood must be sucked up to the mark of 0.5 of the pipette and the dilution fluid must be filled up to the 101/11 mark depending on whether the RBC or WBC pipette is used. The contents must be mixed by gently rolling the pipette. This fluid is then used for charging the Neubaur’s counting chamber.
Q.28 Describe the procedure of charging the chamber for doing RBC/ WBC count.
A pipette filled with blood is provided to you. Firstly the chamber and the coverslip are cleaned. The chamber is then mounted on the mechanical stage of the microscope. The initial few drops of the solution are discarded and the tip of the pipette is wiped. The pipette is then placed at a 45° angle at the edge of coverslip and the chamber is charged. The counting chamber must be kept undisturbed for 2-3 minutes, on the stage so that the cells settle down on the ruled area. The WBC count is done under the low power, whereas the RBC count is done under high power. A chart of the squares must be drawn on the paper and the number of cells in each square must be counted and written down.
Method of Total leukocyte count
Let the number of cells counted in 64 squares be “N”
Therefore the number of cells in one square = N/64
Side length of 1 square = 1/4 mm
Area of 1 square = 1/16 mm2
Depth of fluid film = 1/10 mm
So Volume of fluid in 1 square 1/16 × 1/10 =1/160 mm3
Number of cells in 1/160 cu.mm of diluted blood = N/64
Number of cells in 1 cu.mm of diluted blood = N × 160/64
Dilution factor = 1/20
Therefore, no. of cells in 1 cu.mm of undiluted blood =(N × l60 × 20)/64 = N × 50 cells/ cu.mm
Method of RBC count
RBC count is done under the high power objective of the microscope after identifying the RBC counting area.
At least 5 squares, each having 16 smallest squares (preferably 4 corners and 1 central) should be counted to obtain a satisfactory value. While counting each small square, cells touching the top and left margin of each square should be omitted and cells touching the bottom and right margin of each square should be counted. Draw a chart of the counting squares on the paper and record the number of cells in each square.
Calculation
Let the number of cells counted in (5 × 16) = 80 smallest squares be “N”
Number of cells in 1 smallest square is N/ 80 Side of 1 square = 1/20 mm
Area of 1 square = 1/400 mm2
Depth of fluid film in the counting chamber is 1/10 mm
Volume of diluted blood in 1 square
= 1/ 400 × 1/10
= 1/4000 mm3
Number of cells in 1/4000 mm3 diluted blood = N/80
Number of cells in 1 mm3 of diluted blood
= (N/ 80 × 4000)
= (N × 4000)/ 80
(Total diluted volume in bulb of the pipette is 100 parts, out of which 0.5 is blood. So dilution is 0.5 in 100, i.e.1 in 200)
So number of cells in 1 mm3 of undiluted blood
= (N × 4000 × 200)/ 80
= N × l0000
Q.29 What are the dimensions of WBC and RBC squares?
• Each smallest square for RBC counting:
– Area: 1/20 mm × 1/20 mm = 1/ 400 mm2
– Volume: 1/400 mm2 × 1/10 = 1/4000 mm3
• Each smallest square for WBC counting:
– Area: 1/4 mm × 1/4 mm =1/16 mm2
– Volume: 1/16 mm2 × 1/10 mm = 1/160 mm3
Q.30 What are the features of an ideally charged chamber?
These are:
- No flowing of blood into the trenches
- No air bubbles
Q.31 When blood is taken to the mark 0.5 and the diluting fluid to mark 101, why is the dilution 1 in 200 and not 1 in 202?
The dilution of the blood occurs not in its stem but in the bulb of the pipette, the volume of which is 101-1 =100. Hence half volume in hundred gives a dilution of 1 in 200.
Q.32 If Hayem’s fluid is not available can you use any other?
0.9 gm% normal saline can be used but the cells have to be counted within an hour after filling the pipette, even though the red cells are likely to form rouleaux.
Q.33 How do you differentiate red cells from dust particles?
The red cells are appeared in round discs of uniform size and light pink in color whereas the dust particles are angular with varying size and colors
Q.34 What is the composition of Turk’s fluid? What is the function of each constituent?
The composition and function of each constituent is;
- Glacial acetic acid: 1.5 ml (hemolyses the red cells)
- Gentian violet : 1.5 ml (stains the nuclei of WBCs)
- Distilled water: up to 100 ml (as a solvent).
Q.35 What is the composition of Hayem’s fluid?
The Hayem’s fluid is composed of the following substances:
- Sodium chloride 0.5 gm
- Sodium sulphate 2.5 gm
- Mercuric perchloride 0.25 gm
- Distilled water 100 ml
Sodium chloride and sodium sulphate together helps in maintaining the isotonicity of fluid. Sodium sulphate also prevents the clumping of red cells. Mercuric perchloride fixes the cells and acts as a preservative.
Q.36 Name any other accurate method to do RBC count?
Use of electronic cell counter.
Q.37 Why is it necessary to follow the rules of counting?
It is to avoid the error of missing some cells and counting others more than once.
Q.38 What is the fate of leukocytes in this experiment?
The leukocytes in this experiment are as much diluted that its number are considered very negligible to consider because:
- The low count of WBC in comparison to RBC.
- Dilution of the WBC by 100 times.
Occasionally leukocyte may be seen but its concentration is very less (1 WBC for every 600-700 RBCs, i.e. one WBC in 80 squares). So even if it is counted along with the RBCs the RBC count will not vary too much (i.e. 10,000/cmm of blood).
Q.39 What do you mean by the term ‘Glacial’? Why it should be glacial acetic acid in Turx's fluid?
Glacial means pure. Only the pure form of acetic acid can give the refractivity around the WBCs that helps the WBC to be differentiated from the dust particles (which are opaque).
Q.40 What is the fate of the RBCs in this experiment (Total count of leukocytes)?
RBCs are hemolyzed by the glacial acetic acid otherwise it would not be possible to count the WBCs.
Q.41 Can any other agent be used to hemolyze the RBCs?
No, any strong agent will also lyse the WBCs and any weak agent will take a long time to lyse them completely.
Q.42 What is the difference between DLC and absolute leukocyte count?
In DLC the percentages of different leukocytes are determined whereas in absolute count the actual number of different leukocytes per cu.mm of blood is calculated.
Q.43 How does the DLC of a child differ from that of an adult?
In adults, the granulocytes (mostly neutrophil) predominate whereas in children the lymphocytes predominate.
Q.44 Can you get a rough idea of TLC by doing DLC?
Yes, if the cells appear more frequently amongst the RBCs the TLC will be high and vice versa.
Q.45 Enumerate the sources of error in hemocytometry?
These are:
- Pipette error, i.e. inaccuracy in calibration and in measurement.
- Field error, i.e. unequal distribution of cells over the counting chamber due to:
– Overcharging or undercharging of the chamber.
– Presence of grease or oil on slides or coverslip. - Personal error, i.e. wrong counting of cells.
- Statistical error: It is inversely proportional to the square root of the number counted.
Q.46 Can you use oxalate mixture in the Westergren method and citrate solution in Wintrobe’s method?
No, the anticoagulants used for each method can not be interchanged as both the methods are standardized with the specific anticoagulant.
Q.47 What are the advantages and disadvantages of Wintrobe’s and Westergren method?
Wintrobe’s method:
- Advantage:
Same sample of oxalated blood can be used for ESR first and then after one hour for PCV by centrifuging it. - Disadvantage:
The method is less sensitive as the column of blood is not high.
Q.48 Why ESR reading is taken after one hour?
This is because more than 95-98 % of RBCs settle down by the end of this time and after that the rate of sedimentation of RBCs does not affect the ESR significantly.
Q.49 Why the normal values of ESR are more in Wintrobe’s method than that of the Westergren method?
It is because of:
- Effect of atmospheric pressure over the blood column as the tube is kept open in it’s top.
- Nature of powdered mixture of oxalate solution used as an anticoagulant.
Q.50 What is the importance of determining hematocrit?
It is a simple but more accurate test for determining the presence of anemia or polycythemia. It is also used for determining various absolute corpuscular values.
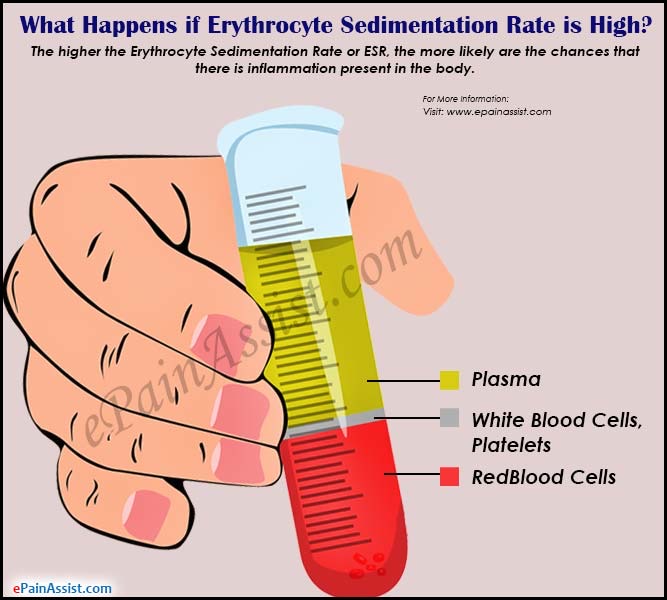
Q.51 Which cells make up the buffy layer? How thick it is? When it’s thickness increases?
The buffy layer consists of packed leukocytes and platelets. It is 1 mm thick. It’s thickness increases in severe leukocytosis, leukemia, and thrombocytosis.
Q.52 What is the difference between PCV of arterial blood and venous blood? What is the reason behind this difference?
The PCV of venous blood is higher than that of arterial blood. It is because in the venous blood the RBCs gain an extra weight due to the entry of water within it resulted due to chloride shift.
Q.53 Why color index is not an appropriate index of hemoglobin content of RBC?
It is because of the wide range of normal values of RBC.
Q.54 Which absolute corpuscular value is most useful?
It is MCHC because:
- It expresses the actual Hb concentration in RBCs only, not in whole blood.
- It does not consider the RBC count for its calculation.
Q.55 Is it possible to know the sex of a person from the blood film?
Yes, in the blood film of females of the Barr body, i.e. chromatin of the sex chromosome is seen in some neutrophils.
Q.56 What are the features of a senile neutrophil?
These are less motile and least effective. These cells commonly break up during the spreading of the blood film.
Q.57 Which stage of neutrophil is most effective?
3-lobed neutrophil is the most motile and functionally most effective in killing the bacteria.
Q.58 Why Cook-Arneth count is not used as a routine investigating tool?
This is because:
- During some physiological conditions neutrophils used to enter the circulation from various storage pools, whereas during some other conditions there is shifting of neutrophils to the storage pools, resulting in a shift to the left or right. This normal phenomenon may give a false indication about the status of bone marrow if we totally depend on this investigating tool.
- Besides this, the better method like bone marrow biopsy are now available for assessing bone marrow function.
Q.59 What are the indications of doing reticulocytes count?
It is to assess the red cell forming and releasing activity of the bone marrow.
Q.60 How does a reticulocyte differs from the RBC?
The reticulocytes are comparatively larger than RBCs and also contain dots, strands, and filaments of bluish stained material.
Q.61 Why does the ABO incompatibility rarely produce hemolytic disease on the newborn?
This is because the anti-A and anti-B antibodies are IgM type of immunoglobulins that do not cross the placenta because of their large MW and thus there is no chance of antigen-antibody reaction.
Q.62 What do you mean by zone phenomenon?
For agglutination to occur the concentration of antigen and antibody has to be the same, otherwise there will be no antigen-antibody reaction. This is termed as zone phenomenon.
Q.63 What are the earliest effects of a mismatched transfusion?
These are: Severe pain anywhere in the body, sense of suffocation, feeling of tightness in the chest, shivering, and even fever.
Q.64 Which blood substitutes may be used to restore blood volume if a suitable donor is not available?
Crystalloid solution (glucose saline) and colloid solutions like human albumin, dextrose with NaCl, etc.
Q.65 Why does calcium deficiency not cause a bleeding disorder though it is essential in blood coagulation?
It is because the calcium required for the blood clotting is in minute quantities.
Q.66 What is a thrombocytopenic purpura and thromboasthenic purpura?
Purpura with normal platelet count is called as athrombocytopenic purpura and purpura with normal count but abnormal circulating platelets are called as thromboasthenic purpura.
Q.67 What do you mean by fragility and hemolysis?
Fragility means the susceptibility of red cells to be broken down by osmotic or mechanical stresses. Whereas the hemolysis means the breaking down of red cells resulting in the release of hemoglobin into the surrounding fluid.
Q.68 What is the effect of 5% glucose, 10% glucose, urine, and urea solution of any strength on red cells?
- 5% glucose: It is isotonic with blood, so no change in size and shape of RBC.
- 10% glucose: It is hypertonic, so there is shrinkage of red cells due to exosmosis.
- Urine: Urine is hypotonic so the red cells will swell up due to the entry of some water.
- Urea solution: Hemolysis of red cells due to entry of urea followed by water into the red cells.
Q.69 Describe the procedure of estimation of hemoglobin by Sahli’s method.
Firstly N/10 HCl solution is taken and put until the 2 gm % mark in the hemoglobin tube. Next, the capillary pipette is selected and the patient’s blood is sucked up to the mark of 20 in the pipette. After placing the pipette in the lower part of the hemoglobin tube, the blood is gently transferred into the HCl solution and the contents are gently stirred. The hemoglobin tube must be placed in the stand so that the scale is turned away from the site and cannot be seen. Dilute the contents with the pure water until the color is the same as that of the standard. The results must be read exactly three minutes after blood has been added to the HCl solution. Hemoglobin values are read at the meniscus of the brown solution.
Q.70 Can strong acids or alkalis be used instead of HCl to measure hemoglobin?
No. the strong acids will oxidize the hemoglobins and the strong alkalis will cause disruption of Hb. So in both cases, there will be no formation of acid hematin.
Q.71 What happens if more or less amount of N/10 HCl is taken instead of the required amount?
If less amount of acid is taken all the hemoglobin will not be converted to acid hematin resulting in a low value. Besides this, there may be clot formation due to improper mixing of blood with acid. On the other hand, if more than the required amount of acid is taken the final color developed in case of severe anemia would be much lighter than the standard.
Q.72 Why it is necessary to convert hemoglobin in acid hematin?
If hemoglobin is not converted into acid hematin then the color of oxyhemoglobin, which has a wide spectrum of colors, cannot be standardized.
Q.73 Can tap water be used for diluting and color matching?
No, as the salt present in the tap water may cause turbidity which will interfere with color matching.
Q.74 Can N/10 HCl be used for diluting and color matching?
Yes
Q.75 While matching the color why it is important to lift the stirrer above the solution but not take it out?
If the stirrer is kept in the solution it will lighten the color and thus matching will occur earlier resulting in low value. On the other hand, if it is taken out every time during the color matching, some solution will go out of the tube and thus again giving a low value.
Q.76 Classify the severity of anemia as per the Hb concentration?
Depending on the Hb level the anemia may be graded as:
- Mild: Hb 10-2 gm%
- Moderate: Hb 5-8 gm%
- Severe: Hb below 5 gm%
Also read: Physiology Questions & Answers

Comments (0)