
Minerals & Water (Viva)
Q .1 What is the average body water content?
60-70% of the body weight.
Q.2 What are the biological functions of water?
- Solvent power.
- Catalytic action.
- Lubricating action.
- High latent heat vaporization.
- High dielectric constant
Q.3 What is the distribution of water in the body?
Intracellular fluid—50% of the bodyweight
Extracellular fluid—20% of the body weight.
a. Plasma—4.5% of body weight.
b. Interstitial fluid and lymph fluids —8% of body weight.
c. Dense connective tissues—6% of body weight
d. Transcellular fluids—1.5% of body weight.
Q.4 What are the effects of dehydration?
- Dehydration leading to electrolyte imbalance due to loss of fluid with the electrolyte.
- Fall in circulating fluid volume leading to shock.
Q.5 What is the principal cation of extracellular fluid?
Sodium
Q.6 What is the principal cation of intracellular fluid?
Potassium
Q.7 What are the normal Na+ and K+ levels in the serum?
Na+=137–148 mEq/L.
K+=3.9–5.0 mEq/L
Q.8 What are the principal minerals required by the body?
Sodium, potassium, magnesium, phosphorus, sulfur, chloride, calcium.
Q.9 What are the trace elements required by the body?
Iron, iodine, copper, zinc, manganese, cobalt, molybdenum, selenium, chromium, fluoride.
Q.10 What are the general functions of minerals?
- As structural components of body tissues.
- In the regulation of body fluids.
- In acid-base balance.
- In the transport of gases.
- In muscular contractions.
Q.11 What are the functions of potassium?
- Intracellular cation in acid-base balance.
- In muscle contraction.
- Conduction of nerve impulse.
- Cell membrane function.
- Enzyme action.
Q.12 What are the conditions in which serum potassium level is increased?
Serum K+ level is increased in:
- Addison’s disease.
- Advanced chronic renal disease.
- Diabetic acidosis.
- Shock.
Q.13 What are the conditions in which serum potassium is decreased?
Serum K+ level is decreased in:
- Diarrhea.
- Metabolic alkalosis
- Familial periodic paralysis
Q.14 What are the functions of sodium?
- In the regulation of acid-base balance.
- In the maintenance of osmotic pressure of body fluids.
- In the preservation of normal irritability of muscles and permeability of the cells.
Q.15 What are the conditions in which serum sodium level is increased?
Serum Na+ is increased in:
- Cushing disease.
- Excessive sweating.
Q.16 What are the conditions in which serum sodium level is decreased?
Serum Na+ is decreased in
- Acute Addison's disease.
- Vomiting, diarrhea.
- Intestinal obstruction.
- Nephrosis.
- Severe burns
Q.17 What is the daily requirement of calcium?
800 mg
Q.18 What are the foods rich in calcium?
Milk, cheese, egg yolk, nuts.
Q.19 What is the normal serum calcium?
9-11 mg%
Q.20 What are the conditions in which serum calcium level is increased?
Serum Ca++ is increased in:
- Hyperparathyroidism.
- Hypervitaminosis-D
Q.21 What are the conditions in which serum calcium is decreased?
Serum Ca++ is decreased in:
- Hypothyroidism.
- Decreased dietary intake.
- Decreased absorption from the intestines.
- Increased loss of calcium due to kidney disease
Q.22 What is rickets?
It is a systemic disease of growing skeletons characterized by effective calcification due to the deficiency of vitamin D.
Q.23 What is the difference between rickets and osteomalacia?
Deficiency of vitamin D gives rise to rickets in children and osteomalacia in adults.
Q.24 What are the functions of calcium?
- In bones and teeth formation
- In nerve impulse transmission
- In muscle contraction
- In the clotting of blood
- In the coagulation of milk.
- Activates certain enzyme systems.
- In neuromuscular excitability.
Q.25 What should be the ideal calcium: phosphorous ratio in the diet?
Calcium: phosphorous ratio should be 1:1 in the diet for ideal absorption.
Q.26 What are the factors which affect calcium absorption?
- Vitamin D promotes the absorption of calcium.
- High protein diet promotes calcium absorption.
- Absorption of calcium requires acidic pH.
- Phylates, oxalates, and phosphates inhibit calcium absorption.
Q.27 What is the normal serum inorganic phosphorus level?
2.5–4.5 mg%.
Q.28 When is the phosphorus level lowered?
- Rickets.
- Hyperparathyroidism.
- Diabetic coma
Q.29 What are the functions of phosphorus?
- Formation of bones and teeth
- Formation of phospholipids.
- Formation of high energy compounds.
- Formation of co-enzymes.
- Formation of organic phosphates
Q.30 What are the sources of iron?
Liver, kidney, egg yolk, nuts, dates, spinach
Q.31 How iron is absorbed in the body?
Iron is present in the foodstuffs as Fe+++ form. Gastric HCl separates Fe+++ from the other combination. Fe+++ form is reduced to Fe++ form by the reducing substances of the food. Now Fe++ form is more soluble and easily absorbed.
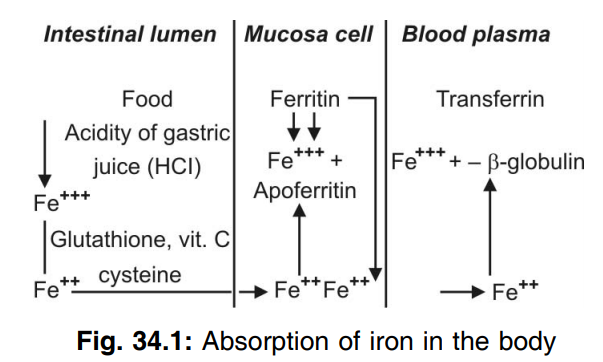
Q.32 What is the transported form of iron?
Transferrin
Q.33 What is the state of iron in transferrin?
Ferric form.
Q.34 Name a few iron-containing compounds.
Hemoglobin, myoglobin, ferritin, transferrin. Enzymes: catalases, peroxidases, cytochromes b, C1, c, a.
Q.35 What is ferritin?
It is the stored form of iron in the body.
Q.36 What is the state of iron in ferritin?
Ferric form
Q.37 What is the daily requirement of iron?
15-20 mg.
Q.38 What is hemosiderosis?
Excessive deposition of iron in the tissues leads to hemosiderosis.
Q.39 What is ceruloplasmin?
It is a transported form of copper in the plasma in combination with proteins.
Q.40 What are the functions of copper?
- Constituent of certain enzymes such as:
- Cytochromes.
- Cytochrome oxidase.
- Catalase.
- Peroxidase.
- Tyrosinase.
- In hemoglobin synthesis.
- Necessary for growth and bone formation.
- Helps in the absorption of iron from the gastrointestinal tract.
Q.41 What is Wilson’s disease?
In Wilson’s disease, copper is deposited in the liver and brain causing hepatolenticular degeneration.
Q.42 What are the functions of zinc?
- Necessary for certain enzymes such as:
- Carbonic anhydrase.
- Carboxy peptidase.
- Lactate dehydrogenase.
- Alkaline phosphatase.
- Necessary for protein synthesis and protein digestion.
- Necessary for optimum insulin action.
Q.43 What is fluorosis?
Excessive intake of fluorine causing mottling and discoloration of the enamel of the teeth.
Q.44 What is the deficiency of magnesium?
Magnesium deficiency can lead to:
- Mitral valve prolapse
- Migraine
- Attention deficient disorder
- Fibromyalgia
- Asthma
- Allergies
Q.45 What is the distribution of magnesium in the human body?
The adult human body contains 25 gm of magnesium. Over 60% of all magnesium is found in the skeleton, 27% in muscle, 6.7% is found in other cells and less than 1% is found outside the cell.
Q.46 What are the functions of magnesium?
- Energy production—Magnesium is required by the adenosine triphosphate (ATP) synthesizing protein in mitochondria.
- Synthesis of essential molecule— Required at number of steps during synthesis of nucleic acid (DNP and RNA), enzymes participating in the synthesis of carbohydrate and lipids.
- Structure roles—Play an important role in bone, cell membranes, and in chromosomes.
- Ion transport across the cell membranes.
- Cell signaling.
- Cell migration.
Q.47 What are iron disorders?
- Hemochromatosis.
- Acquired iron overload.
- Sickle cell anemia.
- Juvenile hemochromatosis.
- Thalassemia.
- Porphyria cutanea tarda.
- Sideroblastic anemia.
- Iron deficiency anemia
Also read: Biochemistry Questions & Answers

Comments (0)