CRANIAL NERVES
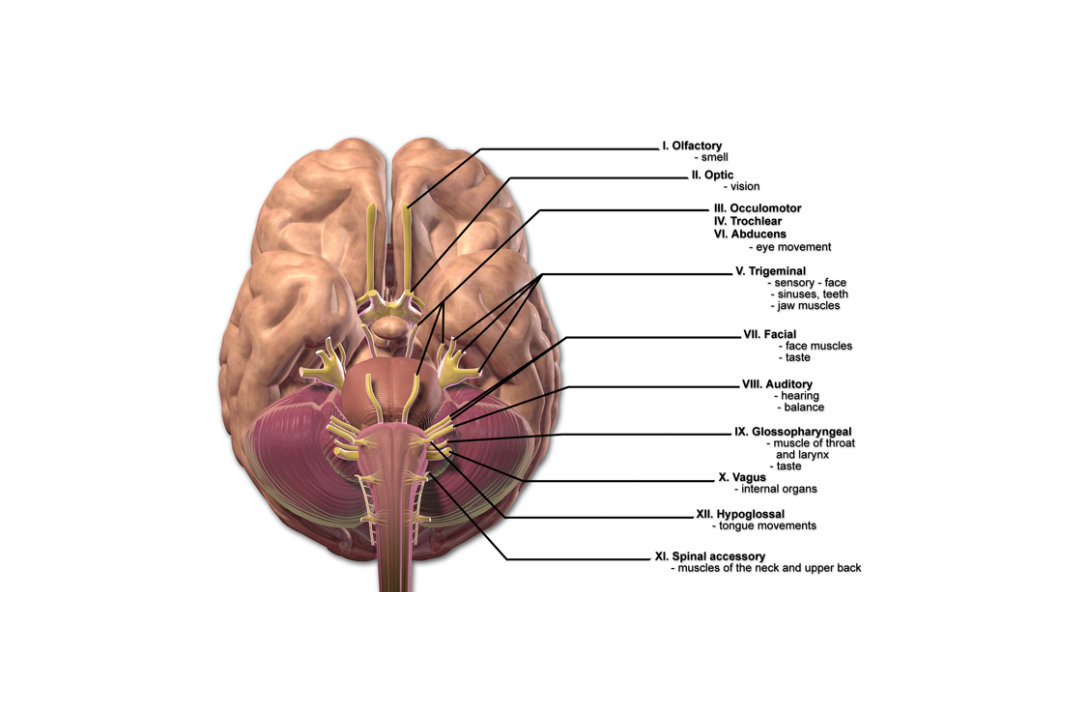
Q.1 Name the cranial nerves.
There are 12 pairs of cranial nerves:
- Olfactory
- Optic
- Oculomotor
- Trochlear
- Trigeminal
- Abducent
- Facial
- Vestibulocochlear (Auditory)
- Glossopharyngeal
- Vagus
- Accessory and
- Hypoglossal
Q.2 How the cranial nerves are classified?
- Purely sensory: I, II, and VIII
- Purely motor: III, IV, VI, and XII
- Mixed: V, VII, IX, X, and XI.
OLFACTORY NERVE
Q.1 Trace the pathway of the olfactory nerve.
Consists of two neurons: Olfactory cells (Receptors)
↓
1st order neuron: Olfactory nerve
↓
Pass through foramina in the cribriform plate of ethmoid
↓
Olfactory bulb
2nd order neuron: Olfactory tract
↓
Divides into
↓
| ↓ | ↓ | ↓ |
| Medial striae ↓ |
Lateral striae ↓ |
Intermediate striae (Sometimes present) ↓ |
| Ends in anterior perforated substance and some fibers cross to the opposite side | anterior perforated substance and primary olfactory cortex | Ends in anterior perforated substance |
| Secondary olfactory cortex |
Q.2 What is the characteristic feature of the olfactory nerve?
The fibers of the olfactory nerve are the central processes of olfactory cells and not the peripheral processes of central ganglion cells.
Q.3 What is hyperosmia?
It is morbid sensitiveness to smell.
Q.4 What is cacosmia?
It is a condition in which a person imagines of non-existent odors.
Q.5 What is the cause of unilateral anosmia (loss of sensation of smell)?
Frontal lobe tumor.
Q.6 What is the cause of bilateral anosmia?
Head injury leading to damage to both olfactory nerves.
OPTIC NERVE
Q.1 What is the length of the optic nerve?
40 mm horizontally and 25 mm vertically is in orbit, 5 mm in the optic canal and 10 mm in the cranial cavity.
Q.2 What are the relations of the intraorbital part of the optic nerve?
Intraorbital part:
- Surrounded by four recti
- Ciliary ganglion: Lateral
- Ophthalmic artery: Inferolateral in posterior part and then crosses above the nerve from lateral to medial side
- Nasociliary nerve: Crosses from medial to lateral side above the nerve.
- Branch of oculomotor nerve to medial rectus: Crosses from medial to lateral side below the nerve.
- Central artery of retina: Below.
Q.3 Trace the optic pathway.
Axons of ganglion cells of retina
↓
Optic nerve
Enters through optic canal
↓
Optic chiasma
(Decussation of fibers occur)
↓
Optic tract
(Has fibers from the nasal half of the macula and retina of the opposite side and temporal half of the same side)
↓
| ↓ Lateral Root | ↓ Medial Root |
| ↓ Terminates in lateral geniculate body | ↓ Terminates in Superior Colliculus, pretectal nucleus, and Hypothalamus |
| ↓ Optic radiation ↓ Pass through the retrolentiform part of the internal capsule ↓ Visual area of cerebral cortex No. 17, 18,19 |
Q.3.1 Trace the pathway of light reflex.
Retina
↓ Optic nerve
↓ Optic chiasma
↓ Optic tract
↓ Lateral geniculate body and pretectal nucleus
↓ Edinger-Westphal nucleus of III cranial nerve
↓ III Cranial nerve
↓ Ciliary ganglion
↓ Short ciliary nerve
↓ Constrictor pupillae muscle
Q.4 What is consensual light reflex?
Constriction of pupil of another eye when the light is flashed on one eye.
Q.5 Why does the consensual light reflex occurs?
- Fibers of each optic nerve enter both optic tracts as a result of partial crossing in chiasma.
- Fibers from each optic tract end in both pretectal nuclei.
- Fibers from each pretectal nucleus end in both the Edinger-Westphal nucleus.
Q.6 What is the pathway for accommodation reflex?
Retina
↓ Optic nerve
↓ Optic chiasma
↓ Optic tract
↓ Lateral geniculate body
↓ Optic radiation
↓ Visual area of cortex
↓ Superior longitudinal association tract
↓ Third nerve nucleus
↓ Ciliary ganglion
↓ Ciliaris and sphincter (constrictor) pupillae muscle
Q.7 What are the characteristic features of the optic nerve?
- It is not a true cranial nerve but is a brain tract that has developed as a lateral diverticulum of the forebrain.
- It is incapable of regeneration after section because it lacks neurilemmal sheath.
- Nerve is enclosed in all the three meningeal sheaths.
- Myelin sheaths are formed by glial cells as in the brain and not by Schwann cells.
Q.8 How the fibers from the optic tract terminate in the lateral geniculate body?
Fibers from the same eye end in laminae 2,3 and 5 and from the opposite eye end in laminae 1,4 and 6 of the lateral geniculate body. Macular fibers end in the central and posterior parts.
Q.9 What is the Argyll-Robertson pupil?
It is a condition in which pupillary light reflex is absent but the accommodation reflex is present. It is caused by cerebral syphilis. Lesion is in pretectal nuclei.
Q.10 What are the effects of lesions of different parts of the visual pathway?
| Site | Effect |
| Retina | Scotoma (loss of corresponding field) |
| Optic nerve | Blindness of same side Consensual light reflex retained |
| Optic chiasma | |
| -Peripheral lesion: | Binasal hemianopia (Bilateral) |
| -Central lesion | Bitemporal hemianopia. |
| Optic tract, lateral geniculate body, optic radiation | Homonymous hemianopia (Loss of temporal field of one side, and nasal field of other side) No macular sparing |
| Visual cortex | Homonymous hemianopia Macular sparing |
Q.11 Trace the pathway for corneal reflex.
Cornea
↓ Branches of ophthalmic division of V cranial nerve
↓ Main sensory nucleus of V cranial nerve
↓ Secondary fibers to motor nuclei of facial nerve of both sides
↓ Fibers of facial nerve nuclei
↓ Orbicularis oculi muscle
OCULOMOTOR NERVE
Q.1 What are the functional components of the oculomotor nerve?
- General visceral efferents (parasympathetic): For constriction of pupil and accommodation.
- Somatic efferent: For movements of the eyeball.
- General somatic afferent: For proprioceptive impulses from muscles of the eyeball.
Q.2 What is the position, subdivisions, and structures supplied by nerves of the oculomotor nucleus?
Position:
At the level of the superior colliculus in the ventromedial part of the central grey matter of midbrain, ventral to the aqueduct. The right and left nuclei fuse to form a midline complex.
Subdivisions:
- Edinger-Westphal nucleus: For ciliaris and sphincter pupillae muscle in a ciliary ganglion.
- Ventromedial nucleus: For superior rectus of both sides.
- Dorsolateral nucleus: For inferior rectus of the same side.
- Intermediate nucleus: For inferior oblique of the same side.
- Ventral nucleus: For medial rectus of the same side.
- Caudal central nucleus:For levator palpebrae superioris of both sides.
Q.3 Name the connections of the oculomotor nucleus.
To:
- Pretectal nuclei of both sides.
- Pyramidal tracts of both sides.
- IV, VI, and VIII nerve nuclei.
- Tectobulbar tract.
Q.4 What are the relations of the oculomotor nerve in superior orbital fissure?
Nasociliary nerve lies in between and abducent nerve inferolateral to, the two rami of the oculomotor nerve.
Q.5 What is ciliary ganglion and what is its position, connections, and branches?
It is a peripheral ganglion in the course of the oculomotor nerve. Has preganglionic fibers from the Edinger-Westphal nucleus.
Position:
Near apex of orbit between optic nerve and tendon of the lateral rectus muscle.
Connections:
- Motor root: From nerve to inferior oblique.
- Sensory root: From the nasociliary nerve.
- Sympathetic root: Branch from internal carotid plexus.
Branches:
Short ciliary nerves 8-10 pierce sclera.
Q.6 What is Weber’s syndrome?
It is a midbrain lesion causing:
- Paralysis of the 3rd cranial nerve of the same side.
- Hemiplegia of the opposite side.
Q.7 What are the effects of the intranuclear lesion of the 3rd cranial nerve?
- Ptosis (Drooping of upper eyelid).
- Lateral squint (Outward deviation of eyeball by lateral rectus and downwards by superior oblique).
- Mydriasis (Dilatation of pupil).
- Cycloplegia (Loss of accommodation).
- Proptosis (Abnormal protrusion of the eyeball).
- Diplopia (Double vision).
- Loss of light reflex and accommodation reflex.
TROCHLEAR NERVE
Q.1 Name the functional components of the IV cranial nerve.
- Somatic efferent: For movement of eyeball.
- General somatic afferent: For proprioceptive impulses from superior oblique muscle.
Q.2 What is the position of the trochlear nucleus?
In the ventromedial part of the central grey matter of the midbrain at the level of the inferior colliculus, ventral to the aqueduct. Fibers from the nucleus cross and emerge on the posterior surface of the brainstem just below the inferior colliculus.
Q.3 What is the effect of the lesion of the IV cranial nerve?
Diplopia occurs on looking downwards.
TRIGEMINAL NERVE
Q.1 What are the functional components of the trigeminal nerve?
- General somatic afferent: From skin and mucosa and proprioceptive from muscle.
- Special visceral efferent: Supplies muscles derived from the mesoderm of the first branchial arch.
Q.2 What is the position of the trigeminal nerve nucleus?
It is made up of:
- Main sensory nucleus: In the upper part of the pons.
- Spinal nucleus: Extends from pons down into the upper two segments of the spinal cord.
- Mesencephalic nucleus: Extends from the upper end of the main nucleus into the midbrain.
- Motor nucleus: In dorsal part of upper pons.
Q.3 What is the position of trigeminal ganglion?
The ganglion is placed in a depression called trigeminal impression in the anterior aspect of the petrous temporal bone and is enclosed in a pouch-like recess of the dura mater.
Q.4 What are the divisions of the trigeminal nerve?
- Ophthalmic nerve: Sensory
- Maxillary nerve: Sensory
- Mandibular nerve: Mixed
Q.5 What is the distribution of the trigeminal nerve?
- Motor: Muscles of mastication.
- Sensory: – Skin of head and face – Mucous membrane of mouth, nose, and paranasal air sinuses.
Q.6 Name the divisions of ophthalmic nerve and structures supplied by it.
Frontal nerve:
By supratrochlear and supraorbital divisions supply upper eyelid, scalp up to lambdoid suture, and skin of forehead in lower and medial part.
Lacrimal nerve:
To lacrimal gland and lateral part of conjunctiva and skin of the upper eyelid.
Nasociliary nerve:
Eyeball, to ciliary ganglion, medial half of lower eyelid, mucosa and skin of nose and dura of anterior cranial fossa.
Q.7 Name the divisions of the maxillary nerve and its distribution.
- Zygomatic nerve: Zygomatico-temporal and zygomatico-facial branches supply skin of temple and cheek.
- Superior alveolar nerves: Teeth of the upper jaw.
- Greater and lesser palatine nerves: Mucous membrane of hard and soft palates and tonsil.
- Nasal branch: Mucous membrane of nose.
- Sphenopalatine branch: Nasal septum.
- Pharyngeal branch: Mucosa of nasopharynx.
- Meningeal branch: Dura mater of middle cranial fossa.
- Palpebral branch: Lower eyelid
- Nasal branch: Skin on the lateral side of the nose
- Superior labial: Skin of upper lip and part of the cheek.
Q.8 What is the distribution of the mandibular nerve?
- Before division to anterior and posterior trunk:
– Nerve to medial pterygoid: Supplies medial pterygoid muscle and gives a branch to the optic ganglion.
– Nerve to tensor palati and tensor tympani.
– Meningeal branch: To dura mater of middle cranial fossa.
- Anterior trunk:
– Buccal nerve: Skin of cheek and mucous membrane on its inner aspect.
– Nerve to masseter, temporalis and lateral pterygoid
- Posterior trunk:
– Auriculotemporal nerve:
Sensory to skin of temple, auricle, external auditory meatus and tympanic membrane and secretomotor fibers to the parotid gland.
– Lingual nerve:
Mucous membrane of the floor of the mouth and anterior 2/3 of the tongue and secretomotor fibers to the sublingual and submandibular salivary glands.
– Inferior alveolar nerve:
Teeth and lower jaw, the skin over the chin and lower lip and nerve to mylohyoid and anterior belly of digastric.
Q.9 What is the effect of complete unilateral lesion of the trigeminal nerve?
Unilateral anesthesia of face and anterior part of the scalp, auricle and mucous membrane of nose, mouth, and anterior two-thirds of the tongue, with paralysis and wasting of muscles of mastication on the affected side.
Q.10 What is ‘trigeminal neuralgia’?
It is the disease of unknown etiology in which there is sudden severe pain in the area of distribution of the trigeminal nerve.
ABDUCENT NERVE
Q.1 Name the functional components of the abducent nerve.
- Somatic efferent: For lateral movement of eyeball.
- General somatic afferent: For proprioceptive impulses from lateral rectus muscle.
Q.2 What is the position of VI cranial nerve nucleus?
Upper part of the floor of the fourth ventricle beneath facial colliculus.
Q.3 What is the effect of paralysis of the abducent nerve?
- Medial squint
- Diplopia
Q.4 What is Raymond syndrome?
It is a pons lesion causing contralateral hemiplegia and paralysis of the abducent nerve on the same side.

Comments (0)