THYROID GLAND
Q.1 What is the situation of thyroid?
In front and sides of the lower part of the neck.
Q.2 What is the extent of thyroid?
- C5,6,7 T1 vertebrae.
- Middle of thyroid cartilage to fifth tracheal ring.
Q.3 Name the capsules of thyroid?
True capsule:
Condensation of connective tissue of gland.
False capsule:
From pretracheal fascia.
Q.4 Why the thyroid is removed along with the true capsule?
To avoid hemorrhage because the capillary plexus is present deep to the true capsule.
Q.5 What is ‘Isthmus’? What are its relations?
It is part of the thyroid gland connecting two thyroid lobes in the lower part.
Extent:
Lies against II, III, and IV tracheal ring.
Relations:
Anterior surface: Strenothyroid Sternohyoid Anterior jugular veins Fascia Skin.
Posterior surface: II, III, and IV tracheal ring.
Upper border: Anastomosis between superior thyroid arteries.
Lower border: Inferior thyroid veins leave gland.
Q.6 What is the arterial supply to thyroid?
- Superior thyroid artery: Branch of the external carotid.
Supplies upper 1/ 3 of lobes and upper 1/2 of the isthmus. - Inferior thyroid artery:
Supplies lower 2/3 of lobes and lower 1/2 of isthmus. Branch of thyrocervical trunk - Thyroidea ima artery: From brachiocephalic trunk.
- Accessory thyroid arteries:
From vessels to esophagus and trachea.
Q.7 What is the venous drainage of thyroid?
- Superior thyroid vein,
- Middle thyroid vein,
- Inferior thyroid vein,
- Sometimes, Fourth thyroid vein (of Kocher).
The veins form a plexus deep to the true capsule of the gland.
Q.8 What is goiter?
Any enlargement of the thyroid gland.
Q.9 In partial thyroidectomy, why the posterior part of lobes are left behind?
- To avoid the risk of removal of parathyroids and
- To avoid post-operative myxedema.
Q.10 Why thyroid moves with deglutition?
Because thyroid is attached to the larynx (cricoid cartilage) by the suspensory ligament of Berry.
Q.11 What are the precautions to the taken during thyroidectomy?
- Ligate superior thyroid artery near gland to avoid injury to external laryngeal nerve.
- Ligate the inferior thyroid artery away from the gland to save recurrent laryngeal nerve.
- Remove thyroid along with its true capsule to avoid injury to venous plexus.
Q.12 How the thyroid is developed?
Immediately behind tuberculum impar (a midline swelling in mandibular arches) in the floor of pharynx a diverticulum called thyroglossal duct develops, which grows down into the neck and its tip bifurcates and proliferates to form thyroid gland. The developing thyroid also fuses with caudal pharyngeal complex.
Q.13 Name the common anomalies of thyroid?
- Pyramidal lobe present.
- Isthmus may be absent.
- One of the lobes may be absent.
- Thyroid gland may be found in an abnormal position, i.e. anywhere in its path of descent, e.g. in the tongue, above or below hyoid.
- Thyroglossal duct may persist and lead to the formation of thyroglossal cyst and fistula.
Q.14 Why enlarging thyroid tends to grow downward?
Because the sternothyroid muscles, which cover the thyroid gland in front, are attached above to the thyroid cartilage, limit the upward expansion of thyroid.
Q.15 Why the enlargements of thyroid produce compression symptoms earlier?
The thyroid is enclosed in pretracheal fascia which is much denser in front than behind. The enlarging gland, therefore, tends to push backward, burying itself around the sides of the trachea and esophagus and compress or displace them, with resulting difficulty in breathing and swallowing.
PARATHYROID GLANDS
Q.1 What is the number of parathyroid glands?
Four
Two superior and two inferior.
Q.2 What is the position of parathyroid glands?
Superior parathyroids:
Usually lies in the middle of the posterior border of lobe of thyroid above the level at which the inferior thyroid artery crosses recurrent laryngeal nerve.
Inferior parathyroids:
Usually below the inferior thyroid artery near the lower end of the posterior border of the thyroid gland.
Q.3 What type of cells are present in parathyroid glands?
- Chief cells or Principal cells: Majority of cells
- Oxyphil or eosinophil cells.
Q.4 How parathyroids are developed?
Superior parathyroids:
From the endoderm of the fourth pharyngeal pouch.
Inferior parathyroids:
From endoderm of third pharyngeal pouch.
The inferior parathyroids are carried down by the descending thymus, while superior parathyroids are prevented from going down because of its relationship to the thyroid.
PITUITARY GLAND (HYPOPHYSIS)
Q.1 What is the position of the pituitary gland?
It lies in the floor of middle cranial fossa in a depression on the superior surface of body sphenoid called sella turcica. It is suspended from the floor of the third ventricle of the brain by a narrow stalk called the infundibulum.
Q.2 What are the relations of the pituitary gland?
Anterosuperior: Optic chiasma
Inferior: Sphenoid air sinus
Lateral side: Cavernous sinus.
Q.3 What are the parts of the pituitary gland?
- Adenohypophysis:
Made up of Pars anterior, Pars intermedia and Pars tubularis - Neurohypophysis:
Made up of Pars posterior and Infundibulum
Q.4 What are the cell types in the pars anterior and what are their secretions?
- Acidophil cells (Alpha cells)
– Growth hormone
– Prolactin - Basophil cells (Beta cells)
– Adrenocorticotropic hormone
– Thyrotropic hormone
– Gonadotrophic hormones. - Chromophobe cells:
Granules are absent and some are stem cells that give rise to chromophil cells.
Q.5 Which hormone is produced by pars intermedia?
Melanocyte stimulating hormone.
Q.6 Which hormone is produced by pars posterior?
- Antidiuretic hormone (Vasopressin)
- Oxytocin
Q.7 Where the hormones of pars posterior are synthesized?
In the nuclei of the hypothalamus, vasopressin in the supraoptic nucleus and oxytocin in the paraventricular nucleus of the hypothalamus. These secretions pass down the axons through infundibulum into pars posterior.
Q.8 What is the function of gonadotrophic hormones?
- Follicle-stimulating hormone:
In females stimulate the growth of ovarian follicles and secretion of estrogens by the ovaries.
In males, it stimulates spermatogenesis. - Luteinizing hormone:
In females, stimulates maturation of corpus luteum and secretion by it of progesterone.
In males, it is called interstitial cell-stimulating hormone and stimulates the production of androgens by interstitial cells of testes.
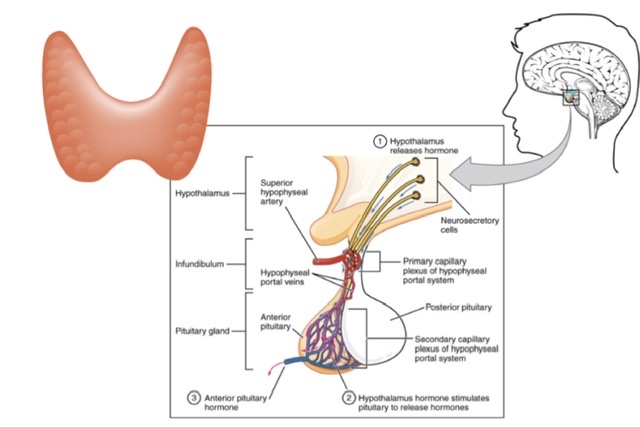
Q.9 What is the hypothalamohypophyseal portal system? What is its significance?
In these two sets of capillaries are present between arteries and veins. One of these is in the median eminence and upper infundibulum and the second set is in sinusoids of pars anterior.
Clinical significance:
Neurons in the hypothalamus produce releasing factors for hormones of the adenohypophysis in capillaries of median eminence and infundibulum. These are carried by the portal system to pars anterior which in turn stimulates to release appropriate hormones.
Q.10 What are ‘pituicytes’?
These are cells in pars posterior.
Q.11 What is the developmental origin of hypophysis?
Adenohypophysis:
Develops from Rathke’s pouch, which arises from the ectoderm lining roof of the primitive mouth (stomodeum).
Neurohypophysis:
Develops as downgrowth from floor of third ventricle.

Comments (0)