MOUTH CAVITY
Q.1 What are the divisions of the oral cavity?
- Vestibule
- Oral cavity proper
Q.2 What the boundaries of vestibule?
External: Lips and cheeks
Internal: Teeth and gums
Q.3 How frenulum of lip is formed?
It is formed by a median fold of mucous membrane between lips and gums.
Q.4 What is the lymphatic drainage of lips?
Central part of the lower lip drains into submental nodes and rest of lip to submandibular nodes.
Q.5 What are the boundaries of the oropharyngeal isthmus (Isthmus of fauces)?
Superior: Soft palate
Inferior: Tongue
On each side: Palatoglossal arches.
Q.6 What do you understand by diphyodont teeth?
Two sets of teeth are present.
First dentition: Milk or deciduous teeth.
Second set: Permanent teeth.
Q.7 What is the dental formula for deciduous teeth?
Incisor 2/2,
Canine 1/1,
Molar 3/3.
Total No. 20
Q.8 What is the dental formula for permanent teeth?
Incisor 2/2,
Canine 1/1,
Premolar 2/2,
Molar 3/3.
Total No. 32
Q.9 Which is the first permanent tooth to appear?
First molar at 6 years of age.
Q.10 Which are wisdom teeth and what age they appear?
Third molar teeth and they appear at age of 17 years or above.
Q.11 What are the parts of a tooth?
3 parts:
- Crown: Projecting above gum
- Root: Embedded in jaw beneath the gum
- Neck: Between crown and root.
SALIVARY GLANDS
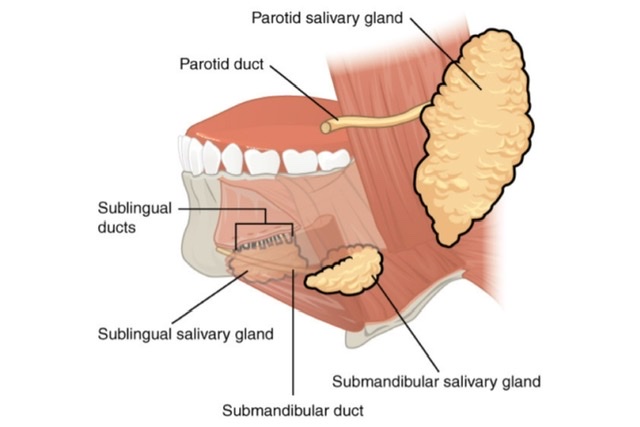
Q.1 Name the salivary glands.
- Parotid,
- Submandibular,
- Small glands in tongue, palate, cheeks, and lips.
Q.2 What is the type of salivary glands?
Exocrine
PAROTID GLAND
Q.1 What is the position of the parotid gland?
Between ramus of mandible and sternomastoid, below the external acoustic meatus
Q.2 What are the attachments of the ‘parotid capsule’?
It is formed by splitting of investing layer of deep cervical fascia between the angle of mandible and mastoid process.
Superficial lamina:
Attached above to the zygomatic arch.
Deep lamina:
To styloid process, mandible and tympanic plate. Also forms stylomandibular ligament.
Q.3 Name the structures within the parotid gland.
- Facial nerve:
Enters through the posteromedial surface and divides into branches that emerge from the anteromedial surface. - External carotid artery:
Enters through the posteromedial surface and divide into branches. - Retromandibular vein:
Formed within the parotid gland by superficial temporal and maxillary veins, superficial to the artery.
Q.4 Name the branches of the external carotid artery (ECA) within the parotid gland.
- Posterior auricular artery,
- Superficial temporal and
- Maxillary.
Q.5 Name the structures pierced by the parotid duct.
- Buccal pad of fat,
- Buccopharyngeal fascia and
- Buccinator muscle.
Q.6 Where the parotid duct opens?
In vestibule of mouth opposite the crown of upper second molar tooth.
Q.7 What are the nerves supplying the parotid gland?
Parasympathetic nerve through auriculotemporal nerve:
Secretomotor.
Sympathetic nerve from plexus around ECA:
Vasomotor
Auriculotemporal nerve:
Sensory
Greater auricular nerve (C2 fibers):
Sensory for parotid fascia.
Q.8 Why the parotid swellings are painful?
Because the parotid fascia is very dense and unyielding. Therefore, it cannot stretch on parotid swelling and causes increased tension beneath the fascia.
Q.9 What is the nature of the parotid gland?
Purely serous.
Q.10 How parotid gland is removed surgically?
In two parts, Superficial and deep, in order to preserve the facial nerve.
SUBMANDIBULAR AND SUBLINGUAL GLAND
Q.1 What is the position of the submandibular gland?
Anterior parts of the digastric triangle.
Q.2 What are the parts of the submandibular gland?
Superficial part:
Large and superficial to mylohyoid.
Deep part:
Small and deep to mylohyoid.
The two parts are continuous around the posterior border of mylohyoid.
Q.3 Name the structure separating the posterior end of the submandibular gland and parotid gland.
Stylomandibular ligament
Q.4 What is the lymphatic drainage of the submandibular gland?
Submandibular lymph nodes which in turn drain into jugulo-omohyoid nodes.
Q.5 Where is the opening of the Submandibular duct?
On the floor of the mouth, on the summit of the sublingual papilla, at the side of the frenulum of the tongue.
Q.6 What is the nerve supply of the submandibular gland?
Secretomotor: Chorda tympani
Sensory: Lingual nerve
Vasomotor: Sympathetic fibers from plexus on facial artery.
Q.7 What is the nature of the submandibular gland?
Mixed, but predominantly serous.
Q.8 Why the incision for removal of the submandibular gland is placed more than 1 inch below the angle of the mandible?
Because marginal mandibular nerve, a branch of VII nerve passes 1 inch behind the angle of the jaw before arching upwards over the body of the mandible.
Q.9 Which artery is likely to be injured in surgery on the submandibular gland?
Facial artery.
Q.10 What is the nature of the sublingual gland?
Mixed, but predominantly mucous.
Q.11 Where the ducts of sublingual gland upon?
About 15 ducts which open on the summit of sublingual fold in the floor of mouth.
Q.12 What is the blood supply of sublingual glands?
From sublingual branch of the lingual artery and submental branch of the facial artery.
Q.13 What is the developmental origin of salivary glands?
Parotid arises as an ectodermal outgrowth from buccal epithelium in relation to line along which maxillary and mandibular processes fuse i.e., just lateral to angle of mouth to form cheek.
Sublingual and submandibular glands are endodermal in origin, arising in relation to linguo-gingival sulcus.
PALATE
Q.1 Name the muscles of the soft palate
- Tensor palati,
- Levator palati,
- Musculus uvulae,
- Palatoglossus and
- Palatopharyngeus.
Q.2 What is the arterial supply of soft palate?
- Greater palatine branch of maxillary,
- Ascending palatine branch of facial and
- Palatine branch of ascending pharyngeal.
Q.3 What is the nerve supply of soft palate?
Motor nerves:
- Tensor palati: Mandibular nerve
- Other muscles: Pharyngeal plexus (Cranial part of accessory through vagus).
General sensory nerves:
- Greater and lesser palatine nerves
- Glossopharyngeal nerve
Special sensory nerve:
Lesser palatine nerve
Secretomotor:
Lesser palatine nerve.
Q.4 What are the functions of the soft palate?
It controls the opening of the pharyngeal and oropharyngeal isthmus, during chewing, coughing, sneezing, speech and swallowing.
Q.5 How is palatine aponeurosis formed? What is its importance?
It is an expanded fibrous band of tensor palati.
It is attached anteriorly to the posterior edge of the hard palate and in the midline, the aponeurosis of two sides fuse with each other
It forms fibrous basis of soft palate and gives attachment to other muscles of palate.
Q.6 What is Passavant’s muscle? What is its importance?
It consists of horizontal fibers of palatopharyngeus at the level of the hard palate, which meet with those of the opposite side. These contract and form a Passavant’s ridge at junction of nasopharynx with oropharynx. Acting along with levator palati, it closes the pharyngeal isthmus preventing food from entering nasopharynx.
Q.7 How is palate developed?
By
- Two palatal processes of the maxillary process and
- Frontonasal process, which is a median structure. These processes fuse and form palate.
The mesoderm of palate undergoes intramembranous ossification to form the hard palate. But, the ossification does not extend into the posterior-most portion, which remains as a soft palate.
Q.8 Which part of the palate is formed by the frontonasal process?
It forms the triangular anterior part of the hard palate which bears the incisor teeth
Q.9 What is cleft palate?
This results from defective fusion of various components of palate. It results in communication between the mouth and nose.

Comments (0)