SCALP
Q.1 What is the extent of the scalp?
Anterior: Supraorbital margins.
Posterior: External occipital protuberance and superior nuchal lines
On each side: Superior temporal lines.
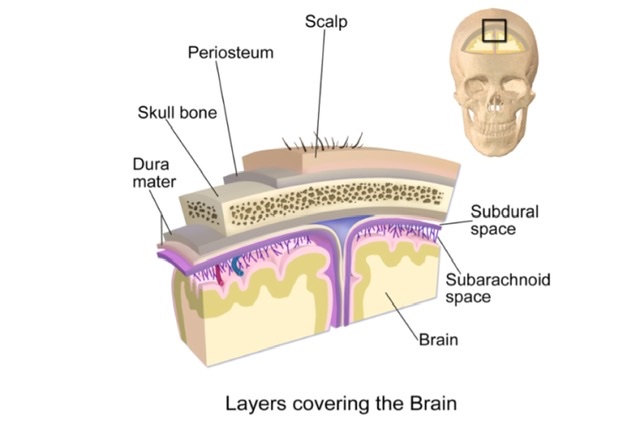
Q.2 Name the layers of the scalp.
- Skin.
- Superficial fascia.
- Epicranial aponeurosis with occipitofrontalis muscle.
- Loose areolar tissue and
- Pericranium (Periosteum)
Q.3 Why the wounds of scalp bleed profusely?
Because of:
- Rich blood supply of scalp and
- The torn vessels fail to retract because of attachment to fibrous fascia.
Q.4 Why the wound of scalp heal rapidly?
Because more vascular the area, the more rapid is healing.
Q.5 Why the infections of superficial fascia of scalp cause much pain?
Because it is dense and fibrous so, little swelling causes much increase in tension.
Q.6 What is the ‘dangerous area of scalp’ and why it is so-called?
Subaponeurotic space (loose areolar tissue).
Because:
- Emissary veins which open here, may transmit the infection from scalp to intracranial venous sinuses.
- Bleeding in this space causes generalized swelling of the scalp and may extend anteriorly into the root of the nose and eyelids, causing a black eye.
Q.7 Why the bleeding or pus collection beneath the periosteum is not extensive?
Because the periosteum adheres to the suture lines of skull bones, so the collection of blood or pus outlines the affected bone (Cephalhaematoma).
Q.8 What is ‘safety valve’ hematoma?
In children, dura and pericranium are more intimately attached to the skull. So, in fractures of vault of skull tearing of both dura and pericranium occurs and the intracranial hemorrhage may make its way through the line of fracture and collect in subaponeurotic space of scalp. No signs of compression of the brain develop until subaponeurotic space is full of blood, such a collection of blood is termed safety valve hematoma.
Q.9 How the hemorrhage from blood vessels of the scalp is arrested?
By pressing with the fingers firmly down on to the skull on either side of the wound, thus compressing the vessels.
Q.10 Which wounds of the scalp gape?
In scalp, skin and epicranial aponeurosis are firmly adherent, and fibers of aponeurosis run anteroposteriorly. A wound of scalp does not gape unless epicranial aponeurosis is divided. Anteroposterior cuts also do not gape because of the direction of fibers.
FACE
Q.11 Why the wounds of face bleed profusely?
Because of its rich vascularity.
Q.12 Why the edema in nephrotic syndrome appears first on face and eyelids?
Because, here the skin is very lax, which facilitates the rapid spread of edema fluid.
Q.13 Why do the wounds of the face tend to gape?
Because the facial muscles are inserted into the skin making it thick and elastic.
Q.14 Why the facial muscles are called ‘muscles of expression’?
They are subcutaneous muscles and they work under a fine control to bring about different shades of facial expressions.
Q.15 Name the muscle producing transverse wrinkles on the bridge of the nose.
Procerus.
Q.16 Name the facial muscle forming the cheek.
Buccinator
Q.17 Name the muscle producing vertical wrinkles on the forehead.
Corrugator supercilii
Q.18 What is the developmental origin of facial muscles?
Second branchial arch.
Q.19 What is the nerve supply of facial muscles?
Facial (VII cranial) nerve.
Q.20 Why headache occurs in sinusitis and cold?
Because of the same sensory nerve supply of face, nasal cavity, and paranasal air sinuses, i.e., trigeminal nerve.
Q.21 What are the branches of the facial artery?
In the neck:
- Ascending palatine
- Tonsillar
- Glandular
- Submental In the face:
- Inferior labial
- Superior labial
- Lateral nasal
- Angular artery: Terminal part.
Q.22 How the facial vein is formed?
By supratrochlear and supraorbital vein near the medial angle of the eye.
Q.23 Which is the ‘dangerous area of face’? Why it is so-called?
- Upper lip and
- Lower part of nose
Because infections of these sites are very common, which may spread in a retrograde direction in facial vein and cause infection and thrombosis of the cavernous sinus through deep connections of the facial vein.

Comments (0)