PERICARDIUM
Q.1 What is pericardium?
It is a fibroserous sac enclosing the heart and roots of great vessels.
Q.2 What are the parts of pericardium?
- Fibrous pericardium: Outer, single-layered, tough, and fibrous.
- Serous pericardium: Inner, double-layered, thin.
Q.3 What are the attachments of fibrous pericardium?
Fibrous pericardium is conical in shape.
Apex: Blunt and fused with roots of great vessels and pretracheal fascia.
Base: Blends with the central tendon of the diaphragm.
Anteriorly: By superior and inferior sternopericardial ligaments, attached to the body of the sternum.
Q.4 What are the different layers of serous pericardium?
- Parietal pericardium:
Outer, fused with fibrous pericardium. - Visceral pericardium:
Inner, fused to heart except where it is separated from the heart by blood vessels. Both layers are continuous at the root of great vessels.
Q.5 What is the pericardial cavity?
It is a potential space between the parietal and visceral layers. It contains a thin layer of serous fluid.
Q.6 What is oblique sinus of pericardium?
It is a space behind the heart between the left atrium, anteriorly and parietal pericardium, inferiorly.
Q.7 What are the boundaries of the oblique sinus of the pericardium?
The boundaries of the oblique sinus of the pericardium are as follows:
Anteriorly: Posterior surface of left atrium converted by serous pericardium.
Posteriorly: Posterior surface of left atrium covered by serous pericardium.
Left wall: Formed by pulmonary veins covered by serous pericardium.
Floor: It is open inferiorly.
Q.8 What is transverse sinus of pericardium?
It is a horizontal gap between ascending aorta and pulmonary trunk anteriorly and superior vena cava and atrium posteriorly. On each side, it opens into pericardial cavity.
Q.9 What are the boundaries of the transverse sinus of the pericardium?
The boundaries of the transverse sinus are as follows:
Anteriorly: Ascending aorta and pulmonary trunk.
Posteriorly: Anterior surface of the left labia
Roof: Reflections of serous pericardium from the posterior surface of the great arterial trunk to the left atria.
Floor: Floor is devoid of serous pericardium.
Q.10 How will you introduce your fingers into the transverse sinus of the heart?
To introduce the finger into the transverse sinus, the superior vena cava is used as a guide. The sinus is located anterior to it and so pass your finger in front of the S.V.C.
Q.11 What is the surgical importance of transverse sinus?
Through this sinus, a temporary ligature is given to occlude pulmonary trunk and aorta during cardiac operations.
Q.12 What is the developmental origin of sinuses of pericardium?
Transverse sinus:
Develops due to degeneration of dorsal mesocardium.
Oblique sinus:
Develops due to the absorption of pulmonary veins into the left atrium.
Q.13 What is the nerve supply of pericardium?
- Fibrous and parietal pericardium:
By phrenic nerve. They are pain-sensitive. - Visceral pericardium:
By autonomic nerves of the heart.
Q.14 What is the arterial supply of pericardium?
- Visceral layer:
By coronary arteries. - Fibrous and parietal layer:
By branches of internal thoracic, musculophrenic, and descending thoracic aorta.
Q.15 What are the contents of the pericardium?
- Heart with cardiac vessels and nerves
- Ascending aorta
- Pulmonary trunk
- Lower half of superior vena cava
- Terminal part of inferior vena cava and
- Terminal part of pulmonary veins.
HEART
Q.1 What is the position of heart?
It is placed obliquely behind the body of the sternum and adjoining parts of costal cartilages of ribs. 1/3 of it lies to right and 2/3 of it lies to the left of the median plane.
Q.2 What are the divisions of the heart?
Heart is composed of four chambers:
- Two atria: Right and left
- Two ventricles: Right and left. T
he atria are separated from ventricles by coronary sulcus (atrioventricular groove). The atria are separated by interatrial groove and the ventricles by anterior and posterior interventricular grooves.
Q.3 Name the structures in anterior and posterior interventricular grooves.
In anterior interventricular groove:
- Interventricular branch of left coronary artery and
- Great cardiac vein.
In posterior interventricular groove:
- Interventricular branch of right coronary artery and
- Middle cardiac vein.
Q.4 Which chambers form the upper border of heart?
Two atria, chiefly left atrium.
Q.5 Which chambers form the left border of heart?
Mainly by left ventricle and Partly by left auricle.
Q.6 Name the chambers forming the surfaces of the heart?
Anterior surface:
Mainly, by the right ventricle and right auricle. Partly, by left ventricle and left auricle.
Inferior surface:
Left 2/3 by left ventricle and Right 1/3 by right ventricle.
Left surface:
Mostly by left ventricle and upper end by left auricle.
Posterior surface (Base):
Mainly by left atrium, Small part by posterior part of the right atrium.
Q.7 What is the right auricular appendage and what are its characteristic features?
It is the upper prolonged end of the right atrium, which covers the root of ascending aorta. Externally, it is notched and the interior is sponge-like.
Q.8 What is the clinical importance of the structure of the right auricular appendage?
Its sponge-like interior prevents the free flow of blood and favor thrombosis which may dislodge to cause pulmonary embolism.
Q.9 What are the parts of the right atrium and how they are developed?
Three parts:
- Smooth posterior part (Sinus venarum):
Derived from the right horn of sinus venosus. All large veins entering the right atrium open in this part. - Rough anterior part including auricle (Atrium proper):
Derived from primitive atrial chamber - Septal wall:
Derived from septum primum and septum secondum.
Q.10 Name the veins opening in the right atrium?
- Superior vena cava,
- Inferior vena cava,
- Coronary sinus
- Anterior cardiac veins and
- Venae cordis minimi.
Q.11 What is the Eustachian valve?
It is a rudimentary valve guarding the opening of inferior vena cava. During embryonic life, it guides the inferior caval blood to the left atrium through foramen ovale.
Q.12 What are the features of the septal wall of the right atrium?
It has
- Fossa ovalis:
Saucer shaped depression in lower part, formed by septum primum. - Limbus fossae ovalis:
It is a prominent margin of fossa ovalis and represents the free edge of septum secondum.
Q.13 What are the parts of the right ventricle?
- Inflowing part:
Rough and has muscular ridges called trabeculae carneae. - Outflowing part:
Smooth. Also called infundibulum.
Opens into the pulmonary trunk. The two parts are separated by a ridge, supraventricular crest and the inflow and outflow parts make an angle of about 90° with each other.
Q.14 What are the different types of trabeculae carneae?
- Ridges: Fixed elevations.
- Bridges: Fixed at ends but free in middle.
- Papillary muscles: Bases attached to the ventricular wall and apex project into the ventricular cavity and are connected to chordae tendineae.
Q.15 How the left atrium is developed?
- Greater part is smooth and is derived from the absorption of a pulmonary vein.
- Auricle develops from primitive atrial chamber.
Q.16 What are the parts of the left ventricle?
Outflow part: Known as aortic vestibule.
Opens into ascending aorta.
Inflow part same as the right ventricle. The inflow and outflow parts are at an acute angle.
Q.17 What is fossa lunata?
It is an impression in the septal wall of the left atrium, corresponding to fossa ovalis of the right atrium.
Q.18 What are the parts of the interventricular septum?
Its right side is convex and bulges into right ventricle.
Greater part of the septum is thick and muscular and a small area near the posterior margin is membranous.
Q.19 What is the developmental origin of ventricles?
The ventricles develop from:
- Bulbus cordis and
- Primitive ventricle
Q.20 How interventricular septum develops?
- Muscular part: Upgrowth from apex of heart.
- Membranous part: Downgrowth from interatrial septum.
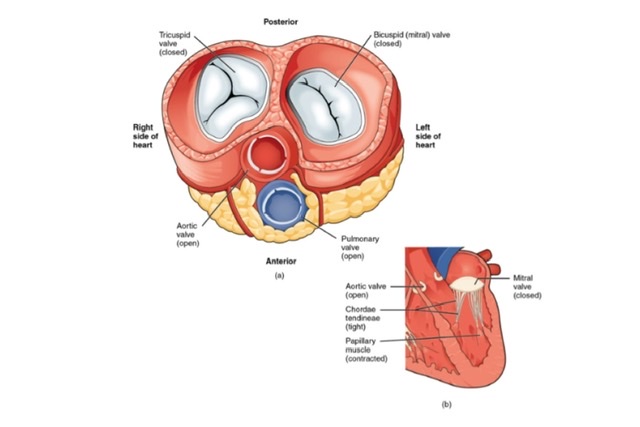
Q.21 What type of valves are present in the heart?
- Atrioventricular valves:
One pair Right atrioventricular valve: Tricuspid valve, made up of three cusps.
Left atrioventricular valve: Bicuspid or mitral valve, made up of two cusps.
- Semilunar valves:
One pair of Aortic and pulmonary valves. Each valve has 3 cusps.
Q.22 What is ‘stenosis’ of the valve?
Narrowing of valve orifice due to the fusion of valve cusps.
Q.23 What is the ‘incompetence’ of the valve?
The imperfect closure of the valve due to dilatation of valve orifice or stiffening of valve cusps.
Q.24 What are the septal defects?
These are the defects resulting from the involvement of interatrial or interventricular septum.
- Atrial septal defects include osteum secondum and osteum primum defects.
An osteum secondum defect lies high up in the atrial wall, while the osteum primum defect lies below. These result in communication between the left and right atria. - Interventricular septal defects which consist mainly of failure of development of the membranous part. These are often associated with other septal defects.
- Complete failure of a septum to form, resulting in the formation of a common atrium or common ventricle or both.
Q.25 What is dextrocardia?
This is a congenital anomaly in which the heart position is reversed and it lies on the right side of the thorax. This may be associated with the reversal of all the intraabdominal organs (situs inversus).
Q.26 What will be the effect of pulmonary stenosis?
There will be right ventricular hypertrophy because the heart tries to force blood through the narrowed valve. This will be associated with congestion in the right atrium followed by secondary right atrial hypertrophy.
Q.27 What is Fallot’s tetralogy?
This is the commonest cyanotic congenital anomaly of the heart and consists of
(1) pulmonary stenosis,
(2) right ventricular hypertrophy,
(3) ventricular septal defect and
(4) an overriding of the aorta over the septal defect.
So, the aorta receives blood from both ventricles.
Q.28 What is the complete transposition of great arteries?
It is a condition in which aorta arises from the right ventricle and pulmonary trunk from the left ventricle.
BLOOD SUPPLY OF HEART
Q.1 What is the origin of the right and left coronary arteries?
- The right coronary artery arises from the anterior aortic sinus. It is smaller than the left.
- The left coronary artery arises from the left posterior aortic sinus.
Q.2 What are the branches of the right coronary artery?
- Marginal branch,
- Posterior (inferior) interventricular branch,
- Nodal branch
- Right atrial branch
- Infundibular and
- Terminal branches.
Q.3 What are the branches of the left coronary artery?
- Anterior interventricular branch.
- Branch to the diaphragmatic surface of left ventricle and
- Left atrial branch.
The continuation of the left coronary artery after anterior interventricular branch is called the circumflex artery.
Q.4 What is the distribution of the right coronary artery?
- Large part of the right ventricle except area adjoining anterior interventricular groove.
- Most of the right atrium.
- Part of the left ventricle, near the interventricular septum.
- Posterior part of interventricular septum.
- SA node in 60% of the cases.
- AV node and Bundle of His except part of the left branch of the AV bundle.
Q.5 What is the distribution of the left coronary artery?
- Large part of the left ventricle
- Right ventricle adjoining anterior interventricular groove
- Left atrium
- Anterior part of interventricular septum
- SA node in 40% of the cases
- Part of the left branch of the AV bundle.
Both the interatrial and interventricular septa are supplied by branches of both coronary arteries.
Q.6 Do the coronary arteries anastomose?
They anastomose to a slight extent. The interventricular branches of the two coronary arteries anastomose near the apex of the heart and in the interventricular septum. Coronary arteries also anastomose with vasa vasora of aorta, internal thoracic artery, and bronchial arteries.
Q.7 What is the clinical importance of the anastomosis between the coronary arteries?
The anastomosis between the branches of the coronary arteries is inadequate to compensate for the sudden occlusion. A blockage therefore leads to death (infarction) of the affected cardiac tissue.
Q.8 What is ‘Angina pectoris’?
It is a clinical condition characterized by pain in front of the chest radiating to the ulnar side of the left arm and forearm. This is due to an incomplete obstruction of the coronary arteries.
Q.9 What are the tributaries of the coronary sinus?
- Great cardiac vein
- Middle cardiac vein
- Small cardiac vein
- Oblique vein of the left atrium
- Posterior vein of the left ventricle and
- Right marginal vein
Q.10 What are Thebsian veins?
These are small veins present in all chambers of heart-opening directly into cavity of chambers.
Q.11 How is the coronary sinus developed?
The coronary sinus is developed from the left horn of the sinus venosus
Q.12 Where does the coronary sinus open?
Into posterior wall of right atrium.
CONDUCTING SYSTEM OF THE HEART
Q.1 What are the functions of conducting system of heart?
- It is responsible for initiating and maintaining normal cardiac rhythm.
- Ensures proper coordination of atrial and ventricular contractions
Q.2 What is the sinuatrial (SA) node and where is it located?
The SA node is the pacemaker of the heart. It is situated in the right atrium along the anterior margin of the opening of the superior vena cava.
Q.3 What is the position of the AV node?
The AV node lies in the wall of the right atrium formed by interatrial septum near the opening of the coronary sinus. It receives an impulse from the SA node.
Q.4 What is Atrioventricular bundle? What are its divisions?
AV bundle forms the connection between atrial and ventricular musculature. It begins at the AV node and reaches the posterior margin of the membranous part of the ventricular septum. Here it divides into left and right branches, which descend on the left and right side of interventricular septum beneath the endocardium. Each branch divides and subdivides to form Purkinje fibers, which terminate in ventricles.
Q.5 What is the ‘moderator’ band?
The ‘moderator’ band also called the septomarginal trabecula (one of the trabeculae carneae) extends from the ventricular septum to the anterior papillary muscle. This is important as it carries the right branch of the atrioventricular bundle (bundle of His). It may assist in preventing the overdistension of ventricle.
Q.6 What is the nerve supply of the heart?
Nerve supply to the heart is by:
- Parasympathetic fibers via the vagus nerve. These are cardioinhibitory.
- Sympathetic fibers from T2-5 segments of the spinal cord. There are cardio accelerator and sensory.
Both types of nerves form superficial and deep cardiac plexus and supply the heart.
Q.7 How is the superficial cardiac plexus formed? What are its branches?
The superficial cardiac plexus formed by:
- The inferior cervical cardiac branch of the left vagus and The superior cervical cardiac branch of the left sympathetic trunk. It is located just below the arch of aorta close to ligamentum arteriosum. It gives branches to deep cardiac plexus, right coronary artery, and left pulmonary plexus.
Q.8 How is the deep cardiac plexus formed and what is its distribution?
The deep cardiac plexus is formed by:
- Cardiac branches of both vagus.
- Cardiac branches of both recurrent laryngeal nerves and
- The cardiac branches of cervical and thoracic branches of sympathetic trunk It gives branches to coronary and pulmonary plexuses and atria.
Also read: Anatomy Question Collection
Also read: Anatomy Questions & Answers
Also read: Anatomy notes

Comments (0)