Portal Vein, Coeliac & Superior Mesenteric vessels (VIVA)
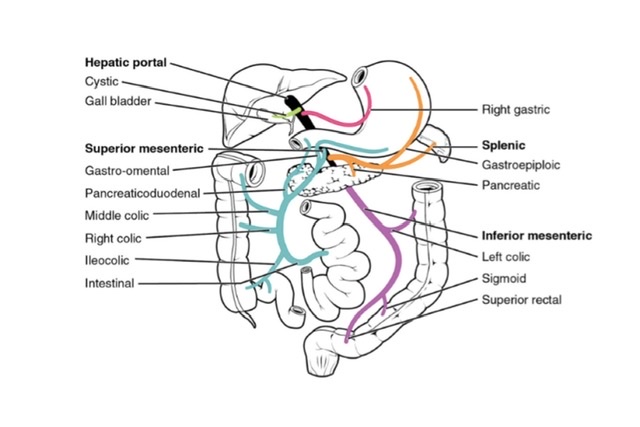
PORTAL VEIN
Q.1 What is the characteristic feature of the portal vein?
Portal vein is one vein that begins and also ends in capillaries, i.e. the vein formed from capillaries of an organ, enter another organ where they divide into another set of capillaries.
Q.2 Name the areas from which the blood is drained by the portal vein.
- Abdominal part of alimentary tract
- Spleen
- Gallbladder
- Pancreas
Q.3 What are the divisions of the portal vein?
The portal vein is divided into 3 parts: Intraduodenal, gastroduodenal, and supraduodenal.
Q.4 What are the relations of different parts of the portal vein?
- Infraduodenal part:
Anteriorly: Neck of pancreas
Posteriorly: Inferior vena cava - Retroduodenal part:
Anteriorly:
First part of duodenum
Gastroduodenal artery
Common bile duct
Posteriorly: Inferior vena cava - Supraduodenal part: Lies in the free margin of the lesser omentum.
Anteriorly: Bile duct Hepatic artery.
Posteriorly: Inferior vena cava.
Q.5 How does the portal vein form and terminate?
Formation:
The portal vein is formed at the level of the L2 vertebra behind the neck of the pancreas, by the union of superior mesenteric and splenic veins.
Termination:
It ends at the right end of porta hepatis by dividing it into a right and a left branch.
Q.6 What are the tributaries of the portal vein?
- Splenic vein
- Superior mesenteric vein
- Left gastric vein
- Right gastric vein
- Superior pancreaticoduodenal vein
- Cystic vein
- Paraumbilical veins.
Q.7 What are the sites of portal-systemic communications? The name also the portal and systemic veins forming these.
| Sites | Portal vein | Systemic vein |
| Umbilicus | The left branch of the portal vein through a paraumbilical vein | Veins of the anterior abdominal wall |
| The lower end of the esophagus | Oesophageal tributaries of left gastric vein | Oesophageal tributaries of the accessory hemiazygous vein |
| Anal canal | Superior rectal vein | Middle and inferior rectal vein |
| Bare area of liver | Hepatic vein | Phrenic and intercostal veins |
| Posterior abdominal wall | Veins of the duodenum, ascending and descending colon | Retroperitoneal veins of the posterior abdominal wall (renal, lumbar, and phrenic veins) |
| Liver | Rarely ductus venosus remains patent and then connects the left branch of the portal vein | Inferior vena cava |
Q.8 What is the importance of portal-systemic communications?
These communications form the important pathways of collateral circulation in portal obstruction and portal hypertension.
Q.9 What is the developmental origin of the portal vein?
- Infraduodenal part:
Part of left vitelline vein - Retroduodenal part:
Dorsal anastomosis between two vitelline veins - Supraduodenal part:
Part of the right vitelline vein.
COELIAC TRUNK
Q.1 Name the structures supplied by the coeliac trunk.
The coeliac trunk supplies derivatives of foregut, i.e.
- The lower end of the esophagus
- Stomach
- Upper 1½ parts of duodenum up to major duodenal papilla
- Liver
- Spleen
- The greater part of the pancreas
Q.2 How the coeliac trunk develops?
The coeliac trunk develops from one of the vitelline arteries (C7 segment).
Q.3 What are the branches of the coeliac trunk?
- Left gastric
- Hepatic and
- Splenic arteries
Q.4 What are the branches of the hepatic artery?
- Gastroduodenal artery: It divides into:
– Right gastroepiploic artery and
– Superior pancreaticoduodenal artery
- Hepatic artery proper
- Right gastric artery
- Supraduodenal artery
- Cystic artery
Q.5 What are the branches of the splenic artery?
- Pancreatic branches
- Short gastric arteries
- Left gastroepiploic artery
- Splenic branches
SUPERIOR MESENTERIC VESSELS
Q.1 Name the structures supplied by the superior mesenteric artery.
The superior mesenteric artery supplies the derivatives of the midgut, i.e.
- Lower 2½ parts of duodenum below the major duodenal papilla
- Jejunum
- Ileum
- Appendix
- Caecum
- Ascending colon
- Right 2/3 of the transverse colon
- Lower 1/2 of the head of the pancreas
Q.2 At what level does the superior mesenteric artery arise?
It arises from the abdominal aorta at the L1 vertebra behind the body of the pancreas.
Q.3 Name the branches of the superior mesenteric artery.
- Inferior pancreaticoduodenal
- Jejunal
- Ileal
- Ileocolic:
To the terminal part of the ileum, appendix, cecum, and lower one-third of ascending colon. - Right, colic:
To the upper two-thirds of ascending colon. - Middle colic:
To the right two-thirds of the transverse colon.
Q.4 What are the relations of the superior mesenteric artery?
- Above the root of the mesentery.
– Anteriorly:
Body of pancreas and splenic vein
– Posteriorly:
Aorta left renal vein,
Uncinate process of the pancreas, and
The third part of the duodenum
– To the right:
Superior mesenteric vein.
- Within the root of the mesentery
– It crosses:
Inferior vena cava
Right ureter
Right, psoas.
– To its right: |
Superior mesenteric vein
Q.5 What are the tributaries of superior mesenteric vein?
- Inferior pancreaticoduodenal
- Jejunal
- Ileal
- Ileocolic
- Right colic
- Middle colic and
- Right gastroepiploic vein.
INFERIOR MESENTERIC VESSELS
Q.1 What are the structures supplied by the inferior mesenteric artery?
It supplies the derivatives of the hindgut, i.e.
- Left 1/3 of the transverse colon
- Descending colon
- Sigmoid colon
- Rectum
- Anal canal above the pectinate line.
Q.2 What are the branches of the inferior mesenteric artery?
- Left colic: Left one-third of the transverse colon and descending colon.
- Sigmoid and
- Superior rectal artery.
Q.3 What is the ‘Marginal artery?
It is an arterial arcade situated along the concavity of the colon formed by anastomosis between ileocolic, right colic, middle colic, left colic and sigmoid arteries. Vasa recta arise from the marginal artery and supply the colon.
Q.4 What is the clinical importance of the marginal artery?
It forms extensive anastomosis, so it is capable of supplying the colon even in the absence of one of the main feeding trunks. This fact is utilized in the surgery of the colon.

Comments (0)