Perinium (Viva)
Q.1 What are the boundaries of the perineum?
Superficial :
Anterior:
Scrotum in male
Mons pubis in female
Posterior: Buttocks.
Lateral:
The upper part of the medial side of the thigh
Deep:
Anterior:
The upper part of the pubic arch
Arcuate pubic ligament.
Posterior: Tip of the coccyx.
Lateral:
Conjoined ischiopubic rami,
Ischial tuberosity, and
Sacrotuberous ligament
Q.2 What are the divisions of the perineum?
An imaginary transverse line joining the anterior parts of ischial tuberosities divides the rhomboid-shaped perineum into two triangular regions:
- Urogenital region: Anterior
- Anal region: Posterior.
Q.3 What are the boundaries of the urogenital triangle?
- Apex: By pubic symphysis.
- On either side: By ischiopubic ramus
- Base: Posteriorly, by an imaginary line joining two ischial tuberosities.
Q.4 What are the boundaries of the anal triangle?
- Apex: By coccyx
- On either side:
Sacrotuberous ligament,
Inferior margin of gluteus maximus, superficially - Base: Imaginary line joining two ischial tuberosities.
Q.5 What is the perineal body?
The fibromuscular structure in the median plane is about 1.25 cm in front of the anal margin. Supports pelvic organs in females.
Q.6 Name the muscles forming the perineal body.
Nine muscles:
- Unpaired:
– External anal sphincter
– Bulbospongiosus
– Fibers of longitudinal muscle coat of rectal ampulla and anal canal.
- Paired:
– Superficial transversus perinei
– Deep transversus perinei
– Levator ani.
Q.7 What is the clinical importance of the perineal body?
In females, it may rupture during childbirth, which if unrepaired may lead to prolapse of the urinary bladder, uterus, and rectum.
Q.8 What are the boundaries of the ischiorectal fossa?
It is a wedge-shaped space, on each side of the anal canal below the pelvic diaphragm between the obturator internus and levator ani.
| Base: Skin |
| Apex: Meeting of obturator fascia with an inferior layer of pelvic fascia. |
| Anterior: The posterior border of perineal membrane. |
| Posterior: Lower border or gluteus maximus and sacrotuberous ligament. |
| Lateral wall: Obturator internus with fascia, Medial surface of ischial tuberosity. |
| Medial wall: External anal sphincter, in the lower part, Levator ani fascia, in upper part. |
Q.9 What are the contents of the ischiorectal fossa?
- Ischiorectal pad of fat.
- Inferior rectal nerve and vessels.
- Posterior scrotal (or labial in females) nerves and vessels.
- Perineal branch of S4 nerve.
- Perforating cutaneous branches of S2,3 nerves.
- Pudendal canal with internal pudendal vessels and pudendal nerve.
Q.10 Why the infections of perianal space are very painful but those of ischiorectal space are much less painful?
Fat in perianal space is tightly arranged in small loculi formed by complete septa therefore little swelling due to infections causes increased tension and pain, but in ischiorectal space, fat is loosely arranged therefore swelling can occur without tension.
Q.11 Why infections are more common in the ischiorectal fossa?
Because of the presence of poorly vascularized fat in the fossa, this region is very vulnerable to infection. Infections usually reach the fossa from the anal canal.
Q.12 Why the unilateral ischiorectal abscess if not drained becomes bilateral?
Because of the extension of infection through the horse-shoe recess behind the anal canal which connects the fossa of both sides.
Q.13 What is Hiatus of Schwalbe?
This is the gap between the obturator fascia and the origin of the levator ani. Herniation of some pelvic contents can take place through the gap.
Q.14 Why in debilitating disorders prolapse of the rectum occurs?
Because of:
- Loss of fat from the ischiorectal fossa which normally acts as a support to the rectum and anal canal.
- Weakness of perineal muscles forming perineal body.
Q.15 Why the abscesses of the ischiorectal fossa can be drained by incision easily?
- Because the fossa has poor vascularity, so there is less blood loss.
- Fossa contains no important structures.
Q.16 Name the structures passing through the gap between the arcuate pubic and transverse perineal ligament.
- Deep dorsal vein of the penis.
- Dorsal nerve of the penis.
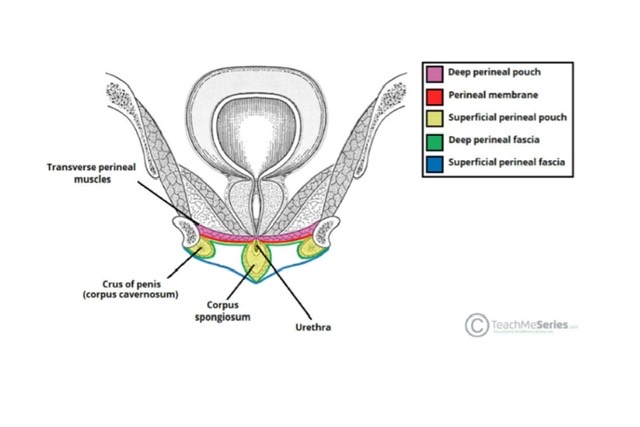
Q.17 How the deep perineal space is formed?
The deep perineal space is formed between the superior and inferior fascia of the urogenital diaphragm.
Q.18 What are the contents of deep perineal space in males?
- Sphincter urethrae
- Deep transverse perinei
- Bulbourethral glands of Cowper
- Internal pudendal artery and its branches
- Dorsal nerve and perineal nerve of the penis: Branches of the pudendal nerve.
Q.19 What are the contents of superficial perineal space in males?
- The root of the penis made up of bulbs and right and left crura
- Bulbospongiosus muscle
- Ischiocavernosus muscle
- Superficial transverse perineal
- Branches of the internal pudendal artery and pudendal nerve.
Q.20 Name the structures piercing the perineal membrane (inferior fascia of the urogenital diaphragm).
In males:
- Membranous urethra
- Branches of perineal nerve to superficial perineal muscles
- Ducts of bulbourethral glands
- Artery and nerve to the bulb (bilateral)
- Urethral artery (bilateral)
- Deep artery of the penis (bilateral)
- Dorsal artery of the penis (bilateral)
- Posterior scrotal nerves and vessels (bilateral).
In females:
- 1, 2 same as above
- Vagina
- Artery and nerve to bulb of vestibule
- Deep artery of clitoris
- Dorsal artery of the clitoris
- Posterior labial arteries and nerves.
Q.21 Name the structures forming the urogenital diaphragm.
- Deep transverse perinei
- The superior fascia of the urogenital diaphragm
- Inferior fascia of the urogenital diaphragm
- Sphincter urethrae.
Q.22 Name the female external genital organs.
- Mons pubis
- Labia majora
- Labia minora
- Clitoris
- Vestibule of the vagina having various openings
- Bulb of vestibule
- Greater vestibular glands (of Bartholin).
Q.23 What are the boundaries of the gynecological perineum?
The area between the posterior commissure (skin connecting prominent posterior ends of labia majora) and anus, constitutes the gynecological perineum.
Q.24 What is the position of glands of Bartholin?
These are homologous with bulbourethral glands (of Cowper) in males. Lie in the superficial perineal space at the vaginal orifice. The duct of each gland opens at the side of the hymen, between the hymen and labium minor.
Q.25 How pudendal canal is formed?
- By splitting of fascia lunata
- The fascial wall of the canal is fused with:
Laterally: Obturator fascia
Medially: Perineal fascia.
Inferiorly: Falciform process of the sacrotuberous ligament.
Superiorly: Arches over ischiorectal fat and fused with the inferior fascia of the pelvic diaphragm.
Q.26 What are the contents of the pudendal canal (Alcock’s canal)?
- Pudendal nerve (S2,3,4)
- Internal pudendal vessels (Fig. 5.55).
Q.27 What are the structures supplied by the pudendal nerve?
- Inferior rectal nerve:
Supplies the external anal sphincter, the skin around the anus, and the anal canal below the pectinate line. - Perineal nerve:
– Posterior scrotal nerves:
Posterior 2/3 of the scrotum in males and posterior labial nerves (sensory) in females to lower one inch of vagina and labium majora.
– Muscular branches:
To urogenital muscles, anterior parts of the external anal sphincter, and levator ani.
The nerve to bulbospongiosus supplies the corpus spongiosum of the penis and urethra.
- Dorsal nerve of the penis:
Supplies skin of the body of the penis and glans.
Q.28 Where is the ‘pudendal nerve block’ given in vaginal operations?
Near the ischial spine, a needle passed through the vaginal wall and then guided by a finger.
Q.29 What are the branches of the internal pudendal artery?
- Inferior rectal artery
- Perineal artery
- Artery of bulb of penis
- Deep and dorsal arteries of the penis

Comments (0)