VAGINA
Q.1 What is the position and extent of the vagina?
It is situated behind the bladder and urethra and in front of the rectum and anal canal. It extends from the vulva to the uterus.
Q.2 What are the variations in the shape of the lumen of the vagina?
- At the upper end: Circular.
- In the middle part: Transverse.
- At the lower end: H-shaped.
Q.3 What are the relations of the vagina?
Anterior wall: 8 cm long
- Upper half:
The base of the bladder. - Lower half:
Urethra
Posterior wall: 10 cm long
- Upper 1/4: Separated from the rectum by a pouch of Douglas.
- Middle 1/2: Separated from the rectum by loose connective tissue.
- Lower 1/4: Separated from the anal canal by the perineal body.
Lateral wall: On each side
- Upper 1/3:
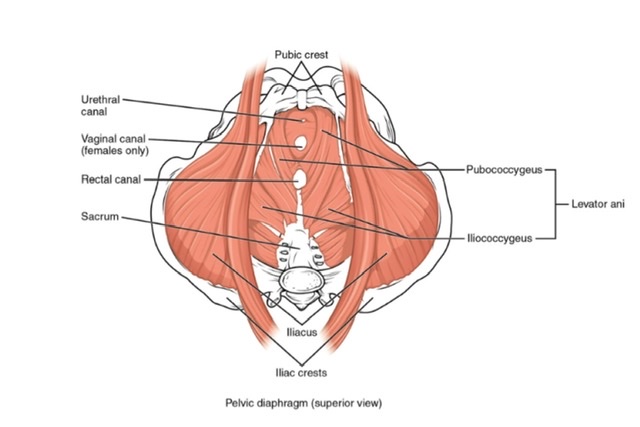
A transverse cervical ligament in which are embedded vaginal veins and ureter crossed by the uterine artery. - Middle 1/3: Levator ani
- Lower 1/3:
Urogenital diaphragm
Bulb of vestibule
Bulbospongiosus
Greater vestibular glands.
Q.4 What are the fornices of the vagina?
The upper part of the vagina is converted into a circular groove by protruding cervix, which is divided into four parts known as vaginal fornices: anterior, posterior and two lateral fornices. The anterior fornix is the shallowest and the posterior fornix deepest.
Q.5 What is the arterial supply of the vagina?
- Vaginal branch of the internal iliac, mainly.
- Upper part: Also by a cervicovaginal branch of the uterine artery.
- Lower part: Also by middle rectal and internal pudendal arteries.
These vessels form anterior and posterior midline vessels called vaginal azygous arteries.
Q.6 What is the lymphatic drainage of the vagina?
- Upper 1/3: External iliac nodes.
- Middle 1/3: Internal iliac nodes.
- Lower 1/3: Medial group of superficial inguinal nodes.
Q.7 What is the nerve supply of the vagina?
- Upper 2/3:
Pain insensitive
Supplied by sympathetic (L1,2) and parasympathetic (S2,3) nerves. - Lower 1/3:
Pain sensitive.
Supplied by inferior rectal and posterior labial branches of the pudendal nerve.
Q.8 What is the characteristic feature of the lining epithelium of the vagina?
The vagina is lined by stratified squamous epithelium and has no glands. It is lubricated partly by cervical mucus and partly by desquamated vaginal epithelial cells.
Q.9 What important information can be obtained by per vaginal (PV) examination?
The condition of:
• Vagina:
Abnormalities of entrance or walls.
• Urethra:
Can be rolled against symphysis in the anterior wall.
• Rectum:
If it contains a tumor, foreign body, or feces.
• Cervix and external os
• Vaginal fornices
• Rectovaginal pouch:
By finger in the posterior fornix. If it contains uterus, prolapsed ovaries, tumors, or abdominal collection of fluid.
• Ureter:
If thickened or has a stone, can be rolled against the pelvic bone just before it enters the bladder.
• To determine the diagonal conjugate of the pelvis, to assess whether the pelvis is large enough to transmit fetal head.
Q.10 What is a hymen?
A fold of mucous membrane at the lower end of the vagina which partially closes it.
Q.11 What is the developmental origin of the vagina?
The vagina is formed by the development of the lumen within the vaginal plate, which is formed by:
- Endodermal cells of the urogenital sinus which proliferate to form sinovaginal bulbs and
- The proliferation of mesodermal cells at the lower end of the uterovaginal canal.
Q.12 What are the abnormalities of the vagina?
- The vagina may be duplicated.
- The Lumen of the vagina may be subdivided by the septum.
- The vagina may be absent.
- The vagina may have abnormal communications with the rectum and urinary bladder

Comments (0)