UTERUS
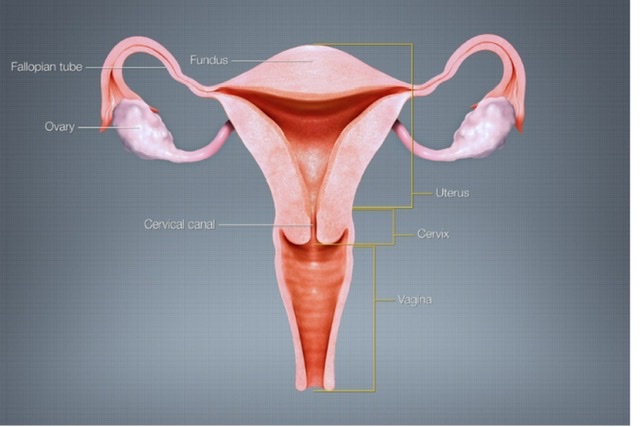
Q.1 What are the parts of the uterus?
- Fundus
- Body
- Cervix: lower 1/3.
The upper 1/3 of cervix forms ‘isthmus’.
Q.2 What are the parts of the cervix?
- Vaginal: Projects into the vagina.
- Supravaginal. The cervical canal (cavity of the cervix) extends from the internal os above to the external os below, where it opens into the vagina.
Q.3 What are ‘arbor vitae’?
The mucous membrane of the cervical canal is thrown into the fold and oblique furrows which pass away from anterior and posterior vertical ridges.
Q.4 What are the angulations of the uterus?
- Angle of anteversion:
Forward angulation between cervix and vagina. About 90 degrees. - Angle of anteflexion:
Forward angulation between body and cervix. About 120 to 125 degrees.
Q.5 Name the structures attached to the lateral border of the body of the uterus.
- Broad ligament.
- Uterine tube at the upper end.
- Round ligament of the uterus: Anteroinferior to the tube.
- Ligament of the ovary: Posteroinferior to the tube.
Q.6 What are the supports of the uterus?
The uterus is prevented from sagging down by a number of factors. They are classified into :
- Primary Supports:
– Muscular:
Pelvic diaphragm including levator ani muscles and pelvic fascia lining them
Perineal body
Urogenital diaphragm.
– Fibromuscular:
Uterine axis
Pubocervical ligaments
Transverse cervical ligament (Mackenrodt or cardinal ligament)
Uterosacral ligament
Round ligament of uterus.
- Secondary supports (of doubtful value):
Broad ligaments
Uterovesical fold
Rectovaginal fold.
Q.7 How uterine axis support the uterus in maintaining its position?
The anteversion prevents the uterus from sagging through the vagina. Any rise in intraabdominal pressure tends to push uterus against bladder, which further accentuates anteversion. The angle of anteversion is maintained by uterosacral and round ligaments.
Q.8 What is the canal of Nuck?
The round ligament of the uterus in the inguinal canal, in fetal life, is accompanied by a process of the peritoneum, which if persists, after birth is known as the canal of Nuck.
Q.9 What are the parts of the broad ligament of the uterus?
- Mesosalphinx: Between tube and ovarian ligament.
- Mesometrium: Below ovarian ligament.
- Suspensory ligament of ovary
- Mesovarium.
Q.10 What are the contents of the broad ligament of the uterus?
- Tube: Uterine tube.
- Ligaments: Round ligament of uterus Ligament of the ovary
- Vessels: Uterine vessels and Ovarian vessels.
- Nerves: Uterovaginal plexus Ovarian plexus.
- Embryological remnants: Epoophoron Duct of epoophoron (Gartner’s duct). Paroophoron.
- Lymphatics and lymph nodes.
- Fibroareolar tissue (Parametrium).
Q.11 What is the arterial supply of the uterus?
- Uterine arteries, mainly
- Ovarian arteries.
Q.12 Name the structures supplied by the uterine artery.
- Uterus
- Vagina
- Medial 2/3 of the uterine tube
- Ovary
- Ureter and
- Contents of the broad ligament.
Q.13 What is the histological structure of the uterus?
The wall of the uterus is made up of 3 layers:
- Outer: Perimetrium (derived from peritoneum)
- Middle: Myometrium (Muscular) consists of 3 layers:
External: Longitudinal fibers
Middle: Muscle fibers interlace
Inner: Circular fibers.
- Inner: Endometrium, consisting of surface epithelium, glands, and stroma.
In the cervix submucosa is absent, so epithelium and glands come in direct contact with myometrium.
Q.14 What is the histological difference between the two parts of the cervix?
The vaginal portion is covered by squamous epithelium which becomes continuous with columnar cells of the cervical canal at external os.
Q.15 Describe the course of the uterine artery and its distribution to the uterus.
The uterine artery is a branch of the anterior trunk of the internal iliac artery.
It runs downwards and forward and when reaches the parametrium, it turns medially towards the uterus. It reaches the uterus at the level of the internal os, where it turns upwards at right angles and runs a spiral course along the lateral border of the uterus to the uterine cornu.
During the vertical part, it gives branches, which run transversely into the myometrium (Arcuate arteries). From these arise radial arteries at right angles and they reach basal layers of the endometrium (Basal arteries). Basal arteries give rise to terminal spiral and straight arterioles of the endometrium.
Q.16 What is the lymphatic drainage of the uterus?
Lymphatics of the uterus form three intercommunicating plexuses, which drain into:
- Upper lymphatics from fundus and upper part of the body: Aortic and superficial inguinal nodes.
- Middle lymphatics from the lower part of the body: External iliac nodes.
- Lower lymphatics from cervix: External and internal iliac and sacral nodes.
Q.17 What are the changes in uterus with age?
| In fetal life: The cervix is larger than the body of the uterus. |
| At puberty: Uterus enlarges. The body grows more than the cervix so it acquires its pyriform shape. |
| During menstruation: Uterus slightly enlarged and more vascular. |
| During pregnancy: Uterus enormously enlarged. |
| After pregnancy: Regresses to normal size but the thickness of the wall and size of the cavity remains larger. |
| In older age: The uterus is smaller and denser in texture. |
Q.18 How is the uterus divided into upper and lower segments during pregnancy?
The uterus is divided into the upper uterine segment consisting of the fundus and the greater part of the body and the lower segment consisting of the lower part of the body and cervix. The upper one-third of the cervix is known as the isthmus.
Q.19 What is the developmental origin of the uterus?
The epithelium of the uterus develops from fused paramesonephric ducts. Myometrium from surrounding mesoderm. The unfused part of the paramesonephric duct embedded in the myometrium forms the fundus.
Q.20 What are the common anomalies of the uterus?
- The uterus may be duplicated or absent.
- The Lumen of the uterus may be divided by a septum.
- One-half of the uterus may be absent (unicornuate uterus).
- The uterus may remain rudimentary.
Q.21 What are the advantages and disadvantages of a midline incision made in the uterus?
The midline part of the uterus is the least vascular part, so there is less bleeding during surgery but the wound also heals poorly due to poor vascularity.
Q.22 What precaution should be taken in relation to the ureter while removing the uterus (hysterectomy)?
At the supravaginal cervix, the ureter lies just above the level of the lateral fornix and below uterine vessels as these pass within the broad ligament. In hysterectomy, the ureter may be accidentally divided when clamping the uterine vessels, especially when pelvic anatomy is distorted.
Q.23 What is the fate of mesonephric ducts and tubules in females?
They form a number of vestigial structures.
- Epoophoron: Represent cranial mesonephric tubules.
- Paroophoron: Represent caudal mesonephric tubules.
- The duct of Epoophoron: Represents the mesonephric duct.
Q.24 How vesicular appendix is developed?
From the cranial part of the paramesonephric duct

Comments (0)