Prostate & Vas Deferens (Viva)
PROSTATE
Q.1 What is the position of the prostate?
It lies in lesser pelvis, below the neck of the urinary bladder, behind the lower part of the pubic symphysis and upper part of the pubic arch and in front of the ampulla of the rectum.
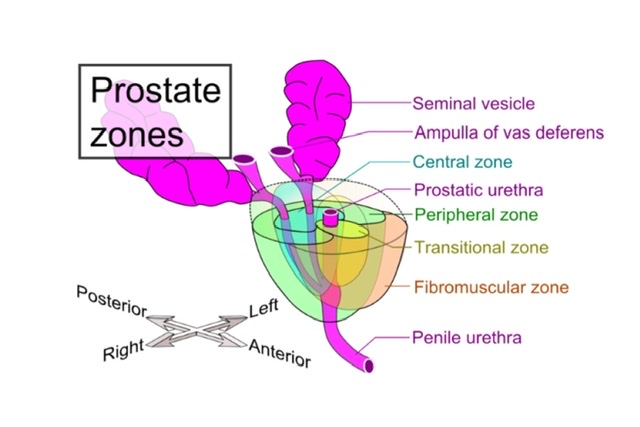
Q.2 What are the lobes of the prostate?
Five lobes :
- Anterior lobe
- Posterior lobe
- Median (Middle or prespermatic) lobe
- Right and left lateral lobes
Q.3 Name the structures lying within the prostate?
- Prostatic urethra.
- Prostatic utricle.
- Ejaculatory ducts.
Q.4 How the capsules of the prostate are formed?
- False capsule:
Outer and is derived from the pelvic fascia. - True capsule:
Inner to false capsule and is formed by condensation of fibromuscular peripheral part of the gland.
Q.5 What is venous drainage of the prostate?
- Veins form a plexus deep to false capsule, around sides and base of the gland. The plexus communicates with vesical plexus, vertebral plexus, and internal pudendal vein.
- Drains into vesical and internal iliac veins.
Q.6 What is the lymphatic drainage of the prostate?
Prostatic lymphatics drain into internal and external iliac nodes.
Q.7 What is ‘cave of Retzius’?
This is a potential retropubic space separating the pubic symphysis and anterior surface of the prostate. This is filled with fat.
Q.8 What is the ‘pathological capsule of prostate’?
In benign tumors of the prostate, the normal peripheral part of the gland becomes compressed into a capsule around the tumor mass.
Q.9 What are ‘valveless vertebral veins of Bateson’? What is their clinical importance?
Some veins of prostatic plexus communicate with plexus of veins lying in front of vertebral bodies and neural canal. These veins are valveless.
Clinical importance:
Because of these valveless veins, there is a retrograde spread of carcinoma of the prostate to pelvis and vertebrae.
Q.10 Which part of the prostate is enlarged in benign hypertrophy?
Benign hypertrophy most commonly affects the median lobe of the prostate. This lobe enlarges upwards and forwards to produce projection on the interior of urinary bladder just behind internal urethral orifice, thus obstructing it.
Q.11 Which part of the prostate is affected by the carcinoma?
Outer glandular zone
Q.12 Why rectal involvement is uncommon in carcinoma of the prostate?
Because fascia of Denonvilliers is rarely penetrated by carcinoma of the prostate.
Q.13 What is the histology of the prostate?
Prostate is composed of glands present in smooth muscle stroma. Part of the gland in front of the urethra has dense muscular tissue and very little glandular tissue. The glands are made up of follicles, lined by columnar cells.
Q.14 How prostate is developed?
It develops from buds arising from prostatic urethra.
From epithelium: Secretory part.
From mesoderm: Inner glandular zone.
From endoderm: Outer glandular zone.
From mesenchyme: Muscle and connective tissue.
Q.15 What are the homologous of the prostate in females?
Urethral glands and paraurethral glands of Skene.
Q.16 What do you understand by the enucleation of the adenoma of the prostate?
In enucleation, plane between adenomatous mass and pathological capsule is cleaved, the tumor is removed and peripheral condensed prostatic tissue is left behind. The prostatic venous plexus, lying between true and false capsule, is not disturbed.
DUCTUS DEFERENS (VAS DEFERENS)
Q.1 What is the ampulla of vas?
- The dilated and tortuous part of vas behind the base of the bladder.
- It has no lumen.
Q.2 How ejaculatory duct is formed?
By the union of lower end of seminal vesicle and ductus deferens, at the base of the prostate.
Q.3 What are the constituents of the secretion of seminal vesicle?
- Fructose
- Vesiculase enzyme
- Albumin
Secretion is slightly alkaline.
Q.4 Where do you palpate the vas deferens?
It is felt as a firm structure between thumb and finger as it lies within the spermatic cord at the scrotal neck. As it is traced upwards it passes medial to the pubic tubercle and then through external inguinal ring, which can be felt by invaginating scrotal skin with the fingertip.
Q.5 What is the position of seminal vesicle?
The left and right seminal vesicles lie posterior to base of the urinary bladder, between it and rectum.

Comments (0)