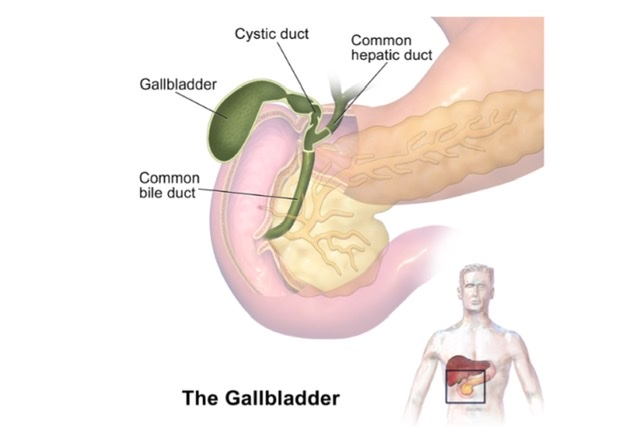
Gallbladder & Extra-Hepatic Biliary Pathway
EXTRA-HEPATIC BILIARY APPARATUS
Q.1 What are the structures forming the extra-hepatic biliary apparatus?
It is formed by:
- Right and left hepatic duct,
- Common hepatic duct,
- Cystic duct and
- Bile duct.
Q.2 What are the parts of the gallbladder?
Gallbladder is divided into three parts:
- Fundus,
- Body and
- Neck, it becomes continuous with cystic duct.
Q.3 What is a Hartmann’s pouch?
It is the dilated posteromedial wall of the neck of the gallbladder. It is directed downwards and backward. Some regard it as a pathological feature.
Q.4 What is the clinical importance of Hartmann’s pouch?
The gallstones may become impacted in the pouch and cause obstruction.
Q.5 What is the capacity fo gallbladder?
30 to 50 c.c., but is capable of 50 fold distention.
Q.6 What is a common hepatic duct?
It is a duct formed by the left and right hepatic duct. It is joined by a cystic duct at an acute angle and then forms the common bile duct.
Q.7 What are accessory hepatic ducts and their clinical importance?
These are present in 15% subjects and arise usually from the right lobe of the liver. These terminate into gallbladder or common hepatic duct or bile duct. If undetected, they are responsible for oozing of bile from the wound after cholecystectomy i.e., removal of the gallbladder.
Q.8 What is the ‘spiral valve of Heister’?
The spiral valve has 5-10 crescentic folds of mucous membranes in the cystic duct which are arranged spirally to form a valve-like structure.
Q.9 What are the relations of the bile duct?
The bile duct is about 7 cm long.
It lies from above downward in:
- Right margin of the lesser omentum. It lies to the right of the hepatic artery and in front of the portal vein.
- Behind the first part of duodenum. The gastroduodenal artery lies to the left of the bile duct.
- Behind the head of the pancreas and it lies in front of the inferior vena cava.
Q.10 What are the structures supplied by the cystic artery?
The cystic artery (usually a branch of the right hepatic artery) supplies blood to the gallbladder, cystic duct, hepatic ducts and upper part of the bile duct.
Q.11 What is the venous drainage of the gallbladder?
The superior surface of the gallbladder drains into hepatic veins through gallbladder fossa. Rest of the gallbladder is drained by cystic veins.
Q.12 What are ‘Crypts of Luschka’?
The mucous membrane contains indentations of the mucosa that sink into the muscle coat, these are known as crypts of Luschka.
Q.13 What is caterpillar turn or ‘Moynihan’s hump’?
It is a dangerous anomaly when the hepatic artery takes a tortuous course and the cystic artery is short. This tortuosity is known as a caterpillar turn.
Q.14 What are the functions of the gallbladder?
- Storage of bile
- Concentration of bile
- Regulates pressure in the biliary system, to maintain normal choledochoduodenal mechanism.
- Secretion of mucin.
- Changing the reaction of bile: bile excreted by the liver has pH 8.2 and gallbladder changes the pH to 7.5-7.2.
Q.15 Why is referred pain felt over the right shoulder in acute cholecystitis?
The referred pain is felt at some other region having the same segmental innervation as the site of lesion (on right side). In acute cholecystitis, the undersurface of the diaphragm is also inflamed. The pain sensation from under the surface of the diaphragm is carried by the phrenic nerve via the C4 spinal segment and skin over the shoulder is also supplied by the C4 spinal segment.
Q.16 What is Courvoisier’s law?
According to the Courvoisier’s law, the dilatation of the gallbladder occurs only in extrinsic obstruction of bile duct e.g., by carcinoma of head of pancreas. Intrinsic obstruction (e.g., by stones) do not cause any dilatation because of associated fibrosis.
Q.17 What is the role of gallbladder in typhoid fever?
The typhoid bacilli persist in the gallbladder and a carrier state develops and typhoid bacilli are disseminated to the population via the feces.
Q.18 What is Charcot’s triad of cholecystitis?
Stone in bile duct causes:
- Intermittent biliary colic
- Intermittent jaundice following each colic and
- Intermittent fever
Q.19 What are the characteristic histological features of gallbladder?
Gallbladder is composed of:
- Mucosa: Lined by tall columnar cells.
- Fibromuscular coat:
Formed of interlacing bundles of smooth muscle fibers.
Connective tissue, with abundant elastic fibers, lies between muscle bundles. - No submucosa
- Serous coat with subserous areolar connective tissue.
Q.20 What is the developmental origin of the extrahepatic biliary apparatus?
- Bile duct is formed by the narrowing of the connection between hepatic diverticulum and foregut.
- Another ventral outgrowth from the common bile duct forms the cystic duct and gallbladder. Hepatic ducts are formed by the lower end of the hepatic diverticulum. The bile duct first opens into the ventral wall of the duodenum, later it migrates to the dorsal (right) surface of the duodenum to the mesenteric border. This migration occurs due to differing rates of growth of duodenal walls.
Q.21 How the hemorrhage during cholecystectomy is controlled?
By compressing the hepatic artery, which gives off a cystic branch, between finger and thumb where it lies in the anterior wall of the foramen of Winslow.
Q.22 Why the gangrene of gallbladder is uncommon in occlusion of the cystic artery?
Because of rich secondary blood supply coming from the liver bed.
Q.23 What are the developmental anomalies of the gallbladder?
- Absence of gallbladder.
- Gallbladder may be septate.
- Double gallbladder with a single or separate cystic ducts.
- Floating gallbladder
Q.24 What are the normal variations in bile ducts?
Normally:
Cystic duct joins the common hepatic duct on the right side to form a common bile duct near the upper border of the duodenum.
Variations:
- Common hepatic and cystic ducts lie parallel before forming one duct.
- Cystic and common hepatic ducts unite behind the pancreas.
- Cystic duct may join a common hepatic duct in front or back of the duodenum.
- Cystic duct may be absent, the common hepatic duct entering gallbladder and common bile duct leaving it.
- Accessory hepatic ducts present.

Comments (0)