Small & Large Intestine (Viva)
INTESTINES
Q.1 What are the different parts of the small intestine?
Small intestine about 6 m long, is divided into:
- Upper fixed part: Duodenum 25 cm in length.
- Lower mobile part: Upper 2/5 forms jejunum and lower 3/5 forms ileum.
Q.2 What are ‘valves of Kerckring’?
These are circular folds of mucous membrane which begin in the second part of the duodenum and extend up to proximal half of ileum.
These increase the absorptive surface area and also retard the passage of food.
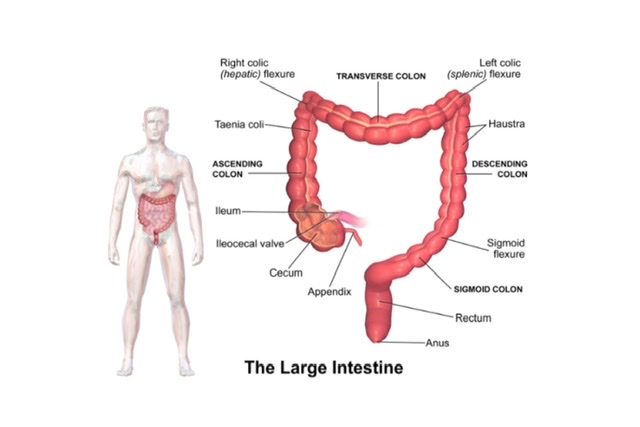
Q.3 What are the different parts of the large intestine?
The large intestine 1.5 m. long, is divided into:
- Appendix: 9 cms long
- Caecum: 6 cms long
- Transverse colon: 50 cm long
- Ascending colon: 15 cm long
- Descending colon: 25 cm long
- Sigmoid colon: 40 cm long
- Rectum: 12 cm long
- Anal canal: 3.8 cm long
Q.4 What are the differences between small and large intestine?
| Small intestine | Large intestine | |
| Calibre | Smaller | Wider |
| Sacculations | Absent | Present |
| Taenia coli | Absent | Present |
| Appendices epiploicae | Absent | Present |
| Fixity | Greater part is freely mobile | Greater part is fixed |
| Transverse mucosal folds | Permanent | Obliterated when longitudinal muscle coat relaxes |
| Villi | Present | Absent |
| Peyer’s patches | Present in ileum | Absent |
Q.5 What are the differences between Jejunum and Ileum?
| Features | Jejunum | Ileum |
| Location | Occupies upper and left part of the intestinal area | Occupies lower and right part of intestinal area |
| Lumen | Larger | Narrow |
| Mesentery | • Windows present • Fat less • Arterial arcades 1 to 3 • Vasa recta longer and |
• Windows absent • Fat abundant • Arterial arcades: 5 to 6 • Vas recta shorter and more fewer |
| Circular | Larger and more mucosal folds | Smaller and sparse. closely set |
| Villi | Large, thick, more | Shorter, thinner and fewer |
| Peyer’s patches | Absent | Present |
| Solitary lymphatic follicles | Fewer | More numerous |
Q.6 What is ‘taenia coli?
These are ribbon-like bands formed by longitudinal muscle coat, present only in large intestine till terminal part of the sigmoid colon.
COLON
Q.1 What are the functions of the colon?
The functions of the colon are:
- Lubrication of feces, by mucus.
- Absorption of salt, water, and other solutes.
- Bacterial flora of colon synthesizes vitamin B.
- Mucoid secretion of colon has IgA antibodies which protect it from invasion by micro-organisms.
- The microvilli of some columnar cells serve a sensory function.
Q.2 What is phrenico-colic ligament?
It is a horizontal fold of peritoneum, attaching left colic flexure to the 11th rib. It supports the spleen and forms the partial upper limit of left paracolic gutter.
Q.3 What are the posterior relations of ascending colon?
- Right iliacus
- Iliac crest
- Right quadratus lumborum
- Right transversus abdominis
- Lateral cutaneous nerve of thigh
- Iliac branch of iliolumbar artery
- Right kidney
- Iliohypogastric nerve
- Ilioinguinal nerve
Q.4 What is attachment of transverse mesocolon?
It is attached to the anterior aspect of the head of the pancreas and anterior border of the body of the pancreas.
Q.5 What are the posterior relations of the descending colon?
- Left kidney
- Left transversus abdominis
- Left quadratus lumborum
- Left iliacus
- Left psoas major
- Iliohypogastric nerve
- Ilioinguinal nerve
- Lateral cutaneous nerve of thigh
- Iliac branch of iliolumbar artery Just above, inguinal ligament it lies over
- External iliac artery
- Femoral nerve
- Genitofemoral nerve
- Testicular vessels
Q.6 What are the structures related to the apex of sigmoid mesocolon?
- Bifurcation of left common iliac artery
- Left ureter
Q.7 What is the features of sigmoid mesocolon.
The sigmoid mesocolon is shaped like an inverted ‘V’ and is attached to the posterior abdominal and pelvic walls.
Q.8 What is the parasympathetic innervation of the gut?
Parasympathetic nerve supply from the pharynx to right two-thirds of the transverse colon is through the vagus. The left one-third of transverse colon, descending sigmoid colon, rectum, and upper part anal canal are supplied through sacral part (S2-4) of the parasympathetic system by pelvic splanchnic branch. Postganglionic parasympathetic neurons are located in myenteric and submucosal plexuses.
Q.9 What is the function of parasympathetic nerves in the gut?
- Stimulate the intestinal movement.
- Inhibit the intestinal sphincters
- Secretomotor to the glands in mucosa.
Q.10 What are the fibers which carry the pain sensation from the gut?
Pain from most of the gut is carried by sympathetic nerves. Pain from pharynx and esophagus is carried by the vagus and from the rectum and lower part of pelvic colon by parasympathetic pelvic splanchnic nerve.
Q.11 What is the blood supply to the colon?
The colon is mainly supplied by a superior mesenteric artery, inferior mesenteric artery, and branches of the internal iliac artery. The superior mesenteric artery gives rise to middle colic, right colic and ileocolic arteries which supply the right colon and the right half of transverse colon. The branches of the inferior mesenteric artery are: left colic, sigmoid, and superior rectal (hemorrhoidal) arteries. These vessels supply the left half of the transverse colon to the proximal rectum. The distal rectum is supplied by inferior and middle rectal (hemorrhoidal) arteries, which are the branches of the internal iliac artery.
Q.12 What is the characteristic feature of the arterial supply of transverse colon?
The right 2/3 of transverse colon develops from the midgut, so it is supplied by the superior mesenteric artery. The left 1/3 is formed from hindgut, so it is supplied by the inferior mesenteric artery.
Q.13 What is the lymphatic drainage of the colon?
- Ascending and transverse colon drain into the superior mesenteric group of preaortic nodes.
- Descending and sigmoid colon drain into the inferior mesenteric group of preaortic nodes.
CAECUM
Q.1 What is the position of caecum?
It is situated in the right iliac fossa above the lateral half of the inguinal ligament.
Q.2 What are communications to the caecum?
Caecum communicates :
- Superiorly with ascending colon
- Medially with ileum
- Posteromedially with appendix.
Q.3 What are the relations of caecum?
Anteriorly: Anterior abdominal wall
Posteriorly: Iliacus, Posas major, Lateral cutaneous nerve of thigh
Q.4 What are the different shapes of caecum?
There are three types of caecum:
- Conical type
- Ampullary type, commonest
- Intermediate type.
APPENDIX
Q.1 What are the dimensions of the appendix?
The length of the appendix varies form 2-20 cm, average about 9 cm. It is longer in children.
Q.2 What are the different positions of the appendix?
The base of the appendix is fixed but its tip can point in any direction. Depending on it following positions of the appendix are described
- Retrocecal, commonest (60%)
- Pelvic (30%)
- Subcaecal
- Preileal
- Postileal
Q.3 What is ‘valve of Gerlach’?
It is an indistinct semilunar fold of mucous membrane guarding the appendicular orifice.
Q.4 What are the peritoneal relations of the appendix?
The appendix is suspended by a small, triangular fold of peritoneum called mesoappendix. Unlike other mesenteries, the mesoappendix is not attached to the posterior abdominal walls but to the mesentery of the terminal part of the ileum.
Q.5 What is the characteristic feature of the blood supply of the appendix?
The appendix is supplied only by an appendicular artery, a branch of ileo-colic artery. It runs first in the free edge of the appendicular mesentery and then distally along the wall of the appendix.
Q.6 What is McBurney’s point?
It is the point of maximum tenderness in acute appendicitis. It lies at the junction of medial 2/3 and lateral 1/3 of a line joining umbilicus to anterior superior iliac spine.
Q.7 What is Murphy’s triad?
Appendicitis first causes pain around umbilicus. Then followed by vomiting and fever. The sequence of symptoms is known as Murphy’s triad.
Q.8 Why the gangrene of the appendix is common in acute infections?
Because the appendicular artery supplying the appendix gets thrombosed and it has no collateral circulation.
MECKEL’S DIVERTICULUM
Q.1 What is Meckel’s diverticulum?
It is a persistent proximal part of the vitellointestinal duct, which normally disappears, during the 6th week of intrauterine life.
Q.2 What is the position of persistent Meckel’s diverticulum?
It is situated 2 feet proximal to the ileocaecal valve, attached to the antimesenteric border of the ileum.
Q.3 What is the clinical importance of Meckel's diverticulum?
- It may cause intestinal obstruction.
- Acute inflammation of diverticulum may resemble appendicitis.
- It is often the site of heterotrophic gastric mucosa with oxyntic cells.
Q.4 What is the effect of patent Meckel’s diverticulum?
Small intestine contents being discharged at the umbilicus.
Q.5 Why the infections of Meckel’s diverticulum are dangerous?
Because
- Its walls are thinner so, it perforates more easily.
- It lies in the middle of the peritoneal cavity, so more chances of widespread peritonitis.
Q.6 What is Enterotomata?
The vitellointestinal duct is closed at both ends, i.e. umbilical and intestinal end, but remains patent in middle. This may cause cysts behind naval called enterotomata.
Q.7 What will happen if the vitellointestinal duct persists as a fibrous band?
- This fibrous band passes from umbilicus to some part of the mesentery or small gut.
- This band may cause compression of the loop of gut under it.
- If attached to the branch of the mesenteric artery, which may be torn during abdominal operations.

Comments (0)