Peritoneum (Viva)
PERITONEUM
Q.1 What is peritoneum?
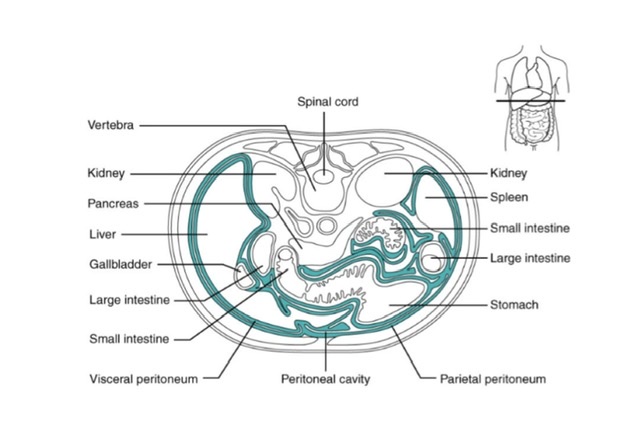
Peritoneum is a large serous membrane (sac) lining the abdominal cavity.
Q.2 What are the different parts of peritoneum?
The peritoneum is divided into:
- Outer layer, the parietal peritoneum.
- Inner layer, the visceral peritoneum.
- Folds of peritoneum, which suspend the viscera.
- Peritoneal cavity
Q.2.1 What are the differences between parietal and visceral peritoneum?
| Features | Parietal peritoneum | Visceral peritoneum |
| Position | Lines the inner surface of abdominal pelvic walls (parieties) and the lower surface of the diaphragm. | Lines the outer and surface of viscera. |
| Attachment | Loosely attached by extraperitoneal connective tissue. | Firmly adherent |
| Blood and nerve supply | Same as overlying parieties | Same as underlying viscera. |
| Pain sensitivity | Sensitive because of somatic innervation. | Insensitive because of autonomic innervation. |
| Development | Derived from somato-pleural layer of lateral plate mesoderm | Derived from splanchno-pleural plate mesoderm layer of lateral plate mesoderm |
Q.3 What are the functions of folds of peritoneum?
- These suspend the organs in the abdominal cavity.
- Provide a degree of mobility to the organs.
- Provide media for the passage of vessels, nerves and lymphatics of the suspended organs
Q.4 What are the different types of peritoneal folds?
The peritoneal folds are divided into 3 types:
- Omenta: Folds suspending the stomach.
- Mesentery: Folds suspending parts of the small and large intestine.
- Ligaments (False Ligament)
Q.5 What is the peritoneal cavity?
It is a potential space lying between the parietal and visceral peritoneum.
Q.6 What are the different parts of the peritoneal cavity?
The peritoneal cavity is divided into two parts:
- Greater sac: Larger
- Lesser sac:
Smaller, situated behind lesser omentum, stomach, and liver.
It also extends into an interval between anterior and posterior parts of the greater omentum.
The two sacs communicate with each other through the epiploic foramen (Foramen of Winslow).
Q.7 What are the retroperitoneal structures related to the lesser sac.
- Anterior surface of head, neck and body of pancreas (Not a Tail)
- Left kidney
- Left suprarenal gland
- Abdominal aorta, upper part
- Diaphragm
- Coeliac trunk and its branches
Q.8 What are peritoneal fossae (Recesses)?
These are small pockets of peritoneal cavity enclosed by small, inconstant of folds of peritoneum. More frequent in newborn babies and most of them become obliterated after birth. The largest of these is a lesser sac. Smaller recesses are found in relation to the duodenum, ileocecal region, and sigmoid mesocolon.
Q.9 What is the ‘Policeman of Abdomen’?
It is greater omentum hanging down from the greater curvature of stomach and covering the loops of intestine. It is called a policeman of abdomen because it limits the spread of infection by moving to the site of infection and sealing it off from the surrounding areas.
Q.10 What are the contents of lesser omentum?
The right free margin of lesser omentum contains:
- Hepatic artery
- Portal vein
- Bile duct
- Hepatic plexus of nerves
- Lymph nodes and lymphatics.
Along the lesser curvature of the stomach and upper border of duodenum, it contains:
- Right and left gastric vessels
- Gastric lymph nodes and lymphatics
- Branches of gastric nerves.
Q.11 What are peritoneal ligaments?
These are the double layers of peritoneum connecting the viscera to each other or to the diaphragm or the abdominal wall or pelvic wall.
Example:
- Falciform ligament
- Right and left triangular ligaments
- Superior and inferior layers of coronary ligaments
- Gastrophrenic ligament
- Gastrosplenic ligament
- Lienorenal ligament
- Hepatogastric ligament
- Hepatoduodenal ligament
- Ligaments of the uterus and urinary bladder.
Q.12 What are the relations of the root of mesentery?
It extends from duodenojejunal flexure on the left side of L2 vertebra to upper part of right sacroiliac joint and is about 15 cm long.
It crosses:
- Third part of duodenum
- Abdominal aorta
- Inferior vena cava
- Right ureter
- Right psoas major
- Right testicular (ovarian) vessels
Q.13 What are the contents of mesentery?
- Jejunal and ileal branches of superior mesenteric artery and veins
- Autonomic nerve plexus
- Lymphatics
- Lymph nodes
- Fat
Q.14 What is Falciform ligament?
It is a sickle-shaped fold of peritoneum which connects the anterosuperior surface of the liver to anterior abdominal wall and undersurface of diaphragm.
Q.15 What is the clinical importance of Epiploic foramen?
Internal hernia can occur into lesser sac through the foramen. If the hernia becomes strangulated then it cannot be reduced by enlarging the foramen because of structures around it. So the gut is first aspirated and then reduced back through the epiploic foramen.
Q.16 At what level epiploic foramen lies?
It is situated at the level of T12 vertebra, behind the right free margin of the lesser omentum.
Q.17 What are the boundaries of epiploic foramen?
Anteriorly: Right free margins of lesser omentum with structures in it.
Posteriorly: Inferior vena cava Right suprarenal gland T12 vertebra
Superiorly: Caudate process of liver
Interiorly: First part of duodenum and Horizontal part of hepatic artery.
Q.18 What are subphrenic spaces?
These are the potential spaces below the diaphragm and are formed by reflections of peritoneum around the liver, they are:
- Intraperitoneal spaces:
– Left subphrenic space
– Left subhepatic space (Lesser sac)
– Right subphrenic space
– Right posterior (subhepatic) space
- Extraperitoneal spaces:
– Right extraperitoneal space (bare area of liver)
– Left extraperitoneal space around the left suprarenal and upper pole of the left kidney.
Q.19 Which part of the liver is related to the superior recess of left subhepatic space?
Caudate lobe of liver
Q.20 What is Morison’s pouch? What is its clinical importance?
Right subhepatic space is known as Morison’s pouch or Hepatorenal pouch.
Clinical importance:
This is the most dependent part of the peritoneal cavity of the abdomen proper in the supine position. This is the commonest site of subphrenic abscess and also fluid effusions tend to accumulate here.
Q.21 What is the rectouterine pouch (pouch of Douglas)?
This is the most dependent part of the peritoneal cavity in the sitting or standing position and of the pelvic cavity in the supine position. The floor of the pouch is only 5.5 cm from the anus.
Q.22 What are the boundaries of the Rectouterine pouch?
Anteriorly: Uterus and posterior fornix of the vagina.
Posteriorly: Rectum
Floor: Rectovaginal fold of peritoneum.
Q.23 What is the clinical importance of rectouterine pouch?
This being the most dependent part of the peritoneal cavity, so the pus tends to collect here and form the pelvic abscess.
Q.24 What is the clinical importance of peritoneal fossae?
Some of these may persist and maybe the site of an internal hernia and strangulation.
Q.25 What is zygosis?
Some of the abdominal organs possess mesentery during the embryonic life, e.g. duodenum, ascending and descending colon, rectum. But due to the fusion of their mesentery with the peritoneum of the posterior abdominal wall (zygosis), these become retroperitoneal.
Q.26 What are the different peritoneal fossae found?
- Lesser sac
- Duodenal fossae
- Superior duodenal fossa: Present in 50%
- Inferior duodenal fossa
- Para duodenal fossa: Present in 20%
- Duodenojejunal fossa: Present in 20%
- Retroduodenal fossa
- Mesentricoparietal fossa of Waldeyer
- Caecal fossae
- Superior ileocaecal fossa
- Inferior ileocaecal fossa
- Retrocaecal fossa
- Intersigmoid fossa
Q.27 What are the different retroperitoneal organs?
- Duodenum
- Ascending colon
- Descending colon
- Kidneys
- Rectum
Q.28 What is the developmental origin of peritoneum?
Parietal layer: From somatopleural layer of lateral plate mesoderm.
Visceral layer: From splanchnopleural layer of lateral plate mesoderm.
Q.29 What is the composition of peritoneal fluid?
- Water electrolytes and solutes derived from interstitial fluid of neighboring tissue and from plasma of adjacent blood vessels.
- Proteins.
- Desquamated mesothelial cells, macrophages, fibroblasts, lymphocytes.
Q.30 Why the irritation of peritoneum produces rigidity of abdominal muscles in that region?
The parietal peritoneum is supplied by somatic spinal nerves which also supply muscle and the skin of the parieties, so, when parietal peritoneum is irritated the abdominal muscles are reflexly contracted, thus producing rigidity of abdominal wall in that region.
Q.31 What is ascites?
Collection of free fluid in peritoneal cavity.
Q.32 What is ‘paracentesis abdominis’ and from which site it is done?
It is the tapping of ascitic fluid. It is done with a trocar and cannula by puncturing the abdomen either in the median plane midway between the umbilicus and pubic symphysis or at a point just above the anterior superior iliac spine.
Q.33 Why the herniation into paraduodenal fossa is associated with hemorrhoids (piles)?
The inferior mesenteric vein formed by superior rectal vein (which drains internal rectal venous plexus) runs in the anterior wall of paraduodenal fossa, is compressed by the pressure of herniated gut.
Q.34 What are the functions of peritoneum?
- Movement of viscera: Peritoneum provides a slippery surface for free movement of abdominal viscera.
- Protection of viscera: Phagocytic cells of peritoneum guard against infections.
- Absorption: Fluid and solutes by mesothelium, which acts as a semipermeable membrane.
- Healing and adhesions: By transformation of mesothelium into fibroblasts.
- Storage of fats: Especially in peritoneal folds.
Q.35 What are the differences between male and female peritoneum?
In male:
- Peritoneum is a closed sac lined by mesothelium.
In female:
- Peritoneal cavity communicates with the exterior through uterine tubes.
- Peritoneum covering ovaries is lined by cubical epithelium.
- Peritoneum covering fimbria is lined by columnar ciliated epithelium.

Comments (0)