Inguinal Canal (Viva)
INGUINAL CANAL
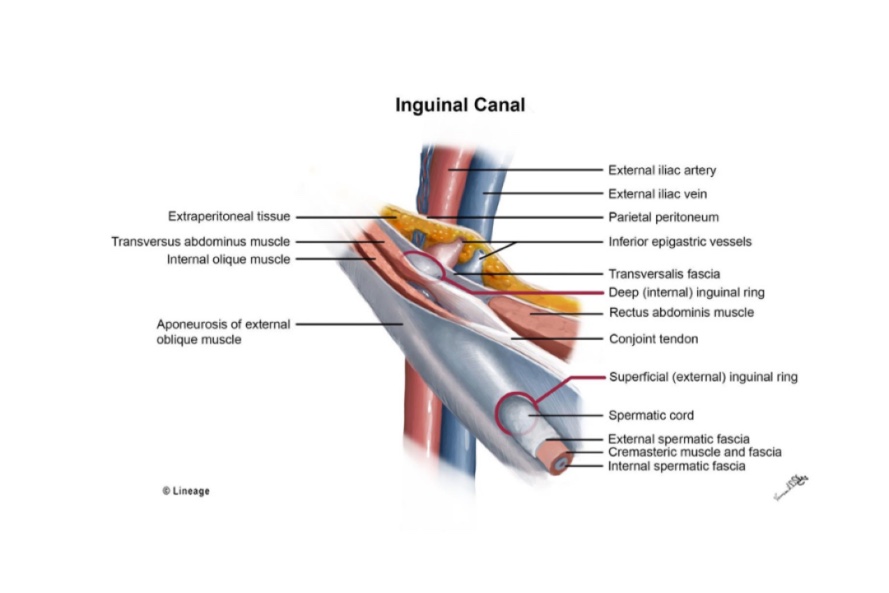
Q.1 What is the position of the inguinal canal?
In the lower part of the anterior abdominal wall, just above the medial half of inguinal ligament. It extends from deep to superficial inguinal ring, downwards and medially.
Q.2 What is the surface marking of the deep inguinal ring?
- Situated half an inch above the mid-point between the anterior superior iliac spine and the pubic symphysis (Mid-inguinal point).
- Oval opening in fascia transversalis.
- Larger in males.
Q.3 What is the surface marking of superficial inguinal ring?
- Just above and lateral to pubic crest.
- Triangular gap in external oblique aponeurosis.
- Medial to ring lie inferior epigastric vessels.
Q.4 What are the boundaries of the inguinal canal?
Anterior
- Skin
- Superficial fascia
- External oblique aponeurosis, over the entire length of the canal.
- Fibers of internal oblique in lateral 1/3 of canal.
Posterior
- Fascia transversalis
- Extraperitoneal connective tissue
- Parietal peritoneum
- Conjoint tendon in medial 2/3
- Reflected part of the inguinal ligament at medial end
Roof
- Arched fibers of the internal oblique and transversus abdominis.
Floor
- Union of inguinal ligament with fascia transversalis.
- Lacunar ligament at medial end.
Q.5 Name the structures passing through the inguinal canal.
- Spermatic cord in males.
- Round ligament of the uterus in females.
- Ilioinguinal nerve in both sexes.
Q.6 Name the structures passing through the deep inguinal ring.
Same as above except ilioinguinal nerve, which enters between external and internal oblique muscles and passes out through superficial inguinal ring.
Q.7 What are the boundaries of Hasselbach’s triangle?
Laterally: Inferior epigastric artery.
Medially: Lateral border of rectus abdominis.
Inferiorly: Medial half of inguinal ligament.
It is divided into two unequal portions by the obliterated umbilical artery.
Q.8 What is a hernia?
It is the protrusion of the contents of the abdomen (usually gut) through an opening or weak area in the wall of the body, e.g. femoral canal, inguinal canal, epiploic foramen.
Q.9 What are the factors which prevent the herniation through the inguinal canal?
- The inguinal canal lies obliquely in the abdominal wall, so deep and superficial ring do not lie opposite each other.
- Weakened posterior wall of the canal due to deep ring is compensated by thickening of the anterior wall by internal oblique muscle.
- Weakened anterior wall of the canal due to superficial ring is compensated by the presence of conjoint tendon and reflected part of an inguinal ligament in the posterior wall.
- With increased intra-abdominal pressure, anterior and posterior walls of the canal get pressed together closing the canal.
- Contraction of internal oblique obliterates the canal, which it reinforces from above, front and behind.
- Contraction of external oblique closes the superficial ring.
- Contraction of cremaster pulls the spermatic cord upwards, making it thicker and closing the superficial ring.
Q.10 What are the different types of inguinal hernia?
- Indirect (oblique) inguinal hernia:
Herniation occurs through the deep inguinal ring, lateral to the inferior epigastric artery. - Direct inguinal hernia:
This occurs through the Hasselbach’s triangle by pushing through the posterior wall of canal.
Two types:
– Medial direct hernia: Medial to obliterated umbilical artery.
– Lateral direct hernia: Lateral to obliterated umbilical artery.
Q.11 What is incomplete and complete inguinal hernia?
Inguinal hernia is incomplete when it does not pass beyond the superficial inguinal ring. In complete hernia, the herniated gut descends in front of testis into tunica vaginalis.
Q.12 What are the main differences, between direct and indirect inguinal hernia?
| Direct inguinal hernia | Indirect inguinal hernia |
| Less frequent | More frequent |
| Placed over the body of the pubic bone. | Placed in the course of the inguinal canal. |
| Neck of the sac: Medial to the inferior epigastric artery |
Neck of the sac: Lateral to the inferior epigastric artery |
| Spermatic cord: Lies on its posterior |
Spermatic cord: Lies behind it and lateral sides. |
| Usually acquired. | Usually congenital. |
Q.13 How will you clinically distinguish an inguinal hernia from a femoral hernia?
An inguinal hernia lies above and medial to the medial end of the inguinal ligament at its attachment to the pubic tubercle. Femoral hernia lies below and lateral to the pubic tubercle.
Q.14 In which sex:
• Inguinal hernia common.
- In males because of the greater diameter of the deep inguinal ring.
• Femoral hernia common and why?
- In females because of larger femoral ring due to broader pelvis and changes in tissues produced by the pregnancy.
Q.15 What can be the contents of a hernial sac?
- Omentum
- Intestine
- Portion of circumference of intestine
- Portion of bladder
- Fluid
Q.16.1 What is Littre’s hernia?
When the Meckel’s diverticulum present in the hernial sac.
Q.16.2 What is a ‘strangulated hernia’?
When the blood supply to hernial contents becomes impaired thus leading to the death of the tissue.
Q.17 How will you clinically distinguish a direct from an indirect inguinal hernia?
By deep ring occlusion test in cases of reducible hernia. The hernia is first reduced and deep (internal) inguinal ring is occluded with a fingertip and the patient is asked to cough while standing.
If it is an indirect hernia, as the deep ring is occluded, it prevents hernial contents from descending into scrotum. But a direct hernia will protrude as contents herniate through the posterior wall of the inguinal canal.
Q.18 What are the coverings of inguinal hernia?
Indirect hernia: From without inwards:
- Skin.
- Fascia of Camper.
- Fascia of Scarpa.
- External spermatic fascia.
- Cremasteric fascia.
- Internal spermatic fascia.
- Extraperitoneal areolar tissue.
- Parietal peritoneum.
Direct hernia:
- Lateral: 1,2,3,4 same as above.
- Fascia transversalis.
- Extraperitoneal tissue.
- Parietal peritoneum.
- Medial: 1, 2, 3, 4 the same as above.
- Conjoint tendon.
- Fascia transversalis.
- Extraperitoneal tissue.
- Parietal peritoneum.
Q.19 What is the developmental origin of the Inguinal canal?
It represents the passage of gubernaculum through the abdominal wall. It extends from the caudal end of developing gonad to labioscrotal swelling.

Comments (0)