Anterior Abdominal Wall (Viva)
Anterior Abdominal Wall
Q.1 What is the position of umbilicus?
- In young adults at the anterior median line at the level of the junction between L3 and L4 vertebra.
- It is lower in infants and in those with a pendulous abdomen.
Q.2 What are different abdominal regions?
The abdomen can be divided into the following nine regions: In the midline from above downwards the regions are epigastrium (EPG); the umbilical region (UHB); and the hypogastrium (HVG), also known as the pubic region. Lateral to the epigastrium, there is the right hypochondrium (RH) and left hypochondrium (LH). Lateral to the umbilical region, there is the right lumbar region (RL) and the left lumbar region (LL). Lateral to the hypogastrium, there is the right inguinal region (I), also called the right iliac fossa and the left inguinal region (LI), also called as the left iliac fossa.
Q.3 What is the developmental origin of umbilicus?
It is scar formed by the remnants of the root of the umbilical cord.
Q.4 What happens if urachus remains patent?
Urinary fistula is formed so that urine may pass through the umbilicus.
Q.5 What is exomphalos?
It is the persistence of the physiological hernia of the midgut loop outside the abdominal cavity.
Q.6 What is the importance of umbilicus?
Anatomical:
- It marks the watershed of the body. The lymph and venous blood do not cross the umbilical plane.
- Supplied by the T10 segment of the spinal cord.
- Site of portacaval anastomosis.
Embryological:
Site of attachment of umbilical cord.
Clinical:
Vitellointestinal duct may persist.
Q.7 What are the remnants of the umbilical cord?
- Median umbilical ligament: Remnant of urachus.
- Lateral umbilical ligament: Formed by obliterated umbilical arteries.
- Ligamentum teres of the liver: Remnant of the left umbilical vein.
Q.8 What are the features of the superficial fascia of the abdominal wall?
Below the umbilicus, superficial fascia is divided into:
- Superficial fatty layer (Fascia of Camper).
- Deep membranous layer (Fascia of Scarpa)
Q.9 What are the attachments of fascia of Scarpa?
- It is continuous below with membranous layer of the superficial fascia of the perineum (Colles’ fascia).
- The line of attachment passes over:
– Along Holden’s line (Lateral to pubic tubercle and extends for about 8 cm).
– Pubic tubercle.
– Body of pubis.
– Deep fascia of adductor and gracilis.
– Margins of pubic arch
– Posterior border of perineal membrane.
– Above umbilicus, it merges with the fatty layer.
Q.10 What are the contents of the superficial fascia of abdominal wall?
- Fat
– Cutaneous nerves.
– Cutaneous vessels.
– Superficial lymphatics
Q.11 Is there any deep fascia in the anterior abdominal wall?
No. This absence of deep fascia allows expansion of the abdominal wall.
Q.12 What is the cutaneous nerve supply of the anterior abdominal wall?
- Anterior cutaneous nerves
– 5 intercostal nerves (T7-11)
– Subcostal nerve (T12)
– Iliohypogastric (L1)
- Lateral cutaneous nerves
2 intercostal nerves (T10-T11)
Q.13 What is the nerve supply of muscles of the anterior abdominal wall?
- Lower six intercostal nerves (T6-11) and subcostal nerve: Branches to external and internal oblique, transversus abdominis, and rectus abdominis.
- Subcostal nerve (T12): Also to pyramidalis
- Iliohypogastric nerve (L1): Internal oblique and transversus abdominis muscle
- Ilioinguinal nerve (L1): Internal oblique.
Q.14 What is the arterial supply of anterior abdominal wall?
- Branches of lower (10th and 11th) intercostal arteries: Branches of descending thoracic aorta.
- Branches of internal thoracic artery: – Superior epigastric – Musculophrenic.
- Branches of external iliac artery: – Inferior epigastric – Deep circumflex iliac
- Branches of subcostal artery: Branch of descending thoracic aorta.
- Branches of the lumbar artery.
- Superficial branches of upper femoral artery: Superficial epigastric, superficial circumflex iliac and superficial external pudendal.
Q.15 What is the lymphatic drainage of the anterior abdominal wall?
- Lymphatic drainage of skin – Above the umbilicus: Axillary nodes. – Below the umbilicus: Superficial inguinal lymph nodes.
- Lymphatic drainage of deeper tissues: External iliac nodes.
Q.16 Where the urine will collect in the rupture of urethral bulb in perineum?
It will be collected in scrotum, perineum, and penis and then lower abdomen deep to fibrous fascial plane. It does not extravasate into lower limb, because of attachment of membranous layer to the deep fascia of the upper thigh along Holden’s line.
Q.17 What is the drainage of cutaneous veins of the anterior abdominal wall?
- Below umbilicus:
Great saphenous vein into the femoral vein which drains into inferior vena cava. - Above umbilicus:
Lateral thoracic vein to axillary vein which drains into superior vena cava. - Few paraumbilical veins:
Into left branch of portal vein along ligamentum teres in falciform ligament. All these veins anastomose with each other.
Q.18 What is caput medusae and its clinical importance?
In portal vein obstruction, the superficial abdominal (cutaneous) veins are dilated for collateral circulation around the umbilicus in a radiating pattern. In caput-medusae, the blood flows upwards above the umbilicus and downwards below the umbilicus.
Q.19 What is the clinical importance of the thoracoepigastric vein?
It is a subcutaneous vein connecting the great saphenous vein with an axillary vein. It becomes dilated and tortuous in vena caval obstructions to provide alternate channel for blood flow. It connects tributaries of lateral thoracic vein draining into an axillary vein and superficial epigastric vein draining into the great saphenous vein which in turn drains into the femoral vein. Clinical importance: In superior caval obstruction, blood in thoracoepigastric vein flows downwards and in inferior caval obstruction, blood flows upwards.
Q.20 Name the muscles of the anterior abdominal wall.
- External oblique
- Internal oblique
- Transversus abdominis
- Rectus abdominis
- Cremaster
- Pyramidalis.
Q.21 What are the functions of the muscles of the anterior abdominal wall?
- Support for abdominal viscera
- Expulsive acts: Helps in micturition, defecation, parturition, etc. by increasing the intra-abdominal pressure.
- Forceful expiratory acts: In coughing, sneezing, blowing.
- Movements of trunks:
– Flexion of trunk: Recuts abdominis.
– Lateral flexion: Oblique muscles.
– Rotation of trunk: External oblique with internal oblique of the opposite side.
- Pyramidalis tenses linea alba.
- Cremaster helps to suspend testis and can elevate it.
Q.22 What is the origin, insertion, and nerve supply of pyramidalis muscle?
Pyramidalis is a small triangular muscle placed in front of rectus abdominis within its sheath.
Origin: Front of pubis and pubic symphysis
Nerve supply: Subcostal nerve.
Q.23 What is a cremasteric reflex? What is its clinical importance?
On stroking the skin of the upper part of the medial side of thigh there is elevation of the testis, due to reflex contraction of the cremaster muscle. Reflex is more brisk in children.
Clinical importance:
In upper motor neuron lesions above the L1 segment, the reflex is lost.
Q.24 What is the Ligament of Poupart?
Inguinal ligament.
Q.25 How inguinal ligament is formed?
Extension of lower border of external oblique aponeurosis, which is thickened and folded backward. It extends from anterior superior iliac spine to pubic tubercle.
Q.26 What are the attachments to inguinal ligament?
Upper border:
- Lateral 2/3: Origin of Internal oblique.
- Medial 1/3: Origin of Transversus abdominis.
Lower border: Fascia lata.
Q.27 Name the extensions of inguinal ligament.
- Pectineal part of inguinal ligament.
- Pectineal ligament (Ligament of Cooper)
- Reflected part of the inguinal ligament.
Q.28 How is conjoint tendon formed ?
Formed by fusion of lower aponeurotic fibers of the internal oblique and transversus abdominis. It is attached to the pubic crest and medial part of pecten pubis.
Q.29 What is the function of conjoint tendon?
It guards the weak point of the superficial inguinal ring.
Q.30 What are the boundaries of the lumbar triangle of Petit and what is its clinical importance?
Floor: Internal oblique muscle.
Below: Crest of ilium.
Laterally: External oblique.
Medially: Latissimus dorsi.
It is the site of the primary lumbar hernia
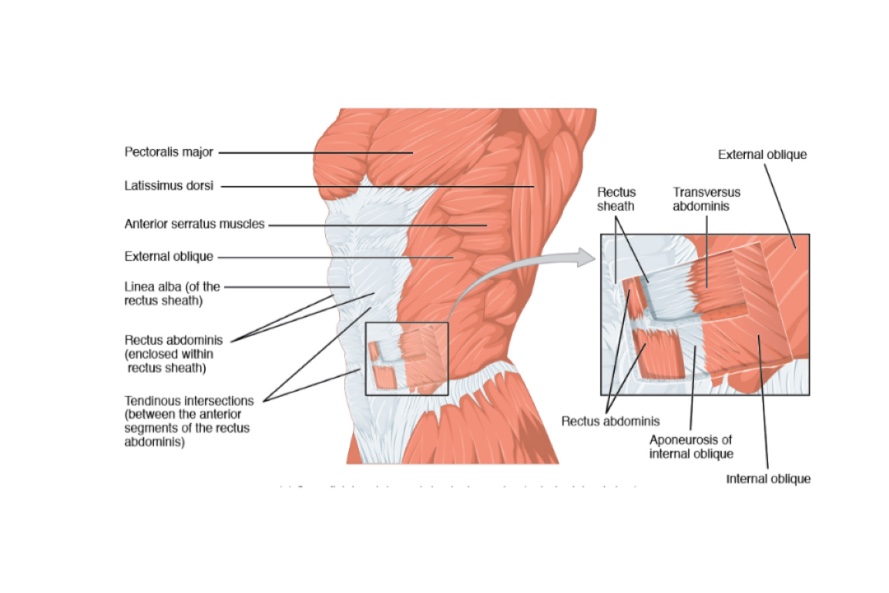
RECTUS SHEATH
Q.1 What is the Rectus sheath?
It is an aponeurotic sheath covering rectus abdominis and pyramidalis muscle with their associated vessels and nerves.
Q.2 How is the Rectus sheath formed?
- Above costal margin:
Anterior wall:
External oblique apo-neurosis.
Posterior wall:
Deficient; Rectus lies directly on costal cartilages.
- Between costal margin and arcuate line:
Anterior wall:
External oblique aponeurosis,
Anterior lamina of internal oblique.
Posterior wall:
Posterior lamina of internaloblique,
Aponeurosis of transversus abdominis
- Below arcuate line:
Anterior wall:
Aponeurosis of all three muscles of the abdomen.
Posterior wall:
Deficient; Rectus muscle rests on fascia transversalis.
Arcuate line (fold or Douglas) represents a lower free margin of posterior wall of the rectus sheath, at the level midway between the umbilicus and pubic symphysis.
Q.3 What are the ‘tendinous intersections’ of Rectus abdominis?
- These are transverse fibrous bands that divide the muscle into smaller parts.
- Three in number: Present
– Opposite umbilicus.
– Opposite lower border of xiphoid.
– In between 1 and 2.
Sometimes intersections may be present below the umbilicus.
- Traverse only the anterior half of the muscle and are adherent to the anterior wall of the rectus sheath.
Q.4 What is the importance of tendinous intersections of Rectus abdominis?
- They represent the segmental origin of the muscle.
- Functionally, they make the muscle more powerful by increasing the number of muscle fibers.
Q.5 Where is the ‘neurovascular plane’ of abdomen is situated?
It lies between the internal oblique and transversus muscle. Various abdominal nerves and vessels run in this plane.
Q.6 What are the functions of the rectus sheath?
- Support the abdominal viscera.
- Increases efficiency of rectus muscle by checking bowing during its contraction.
Q.7 What are the contents of the rectus sheath?
- Muscles: Rectus abdominis, Pyramidalis
- Arteries: Superior epigastric artery, Inferior epigastric artery.
- Veins: Superior epigastric vein, Inferior epigastric vein.
- Nerves: Lower 5-intercostal nerves Subcostal nerve.
Q.8 What is linea alba?
- It is a raphe formed by interlacing fibers of aponeuroses of three muscles forming rectus sheath.
– It extends from the xiphoid process to pubic symphysis.
– Wider above and narrow below the umbilicus.
– It separates the two rectus abdominis muscles from each other.
Q.9 What is the divarication of recti?
- Seen in weak children and multipara women.
- There is a weakness of linea alba, so the fingers can be insinuated between the two recti.
Q.10 Why supraumbilical median incision is given for surgery?
The incision through linea alba is given, because it is made of fibrous tissue only, so there is minimal blood loss. It also does not cause damage to the nerves.
Q.11 In the paramedian incision of the rectus sheath, the rectus muscle is retracted laterally. Explain why?
- To avoid injury to nerves as they enter the rectus through its lateral border.
- On closing the incision, the rectus slips back into its place.
Q.12 Why the trans-rectus incisions are not preferred during surgery?
Because the rectus receives its nerve supply laterally and muscle medial to incision is deprived of its innervation and hence undergoes atrophy.
Q.13 What is fascia transversalis?
Part of abdominopelvic fascia lining inner surface of transversus abdominis muscle and is separated from peritoneum by extraperitoneal tissue which is rich in fat.
Q.14 What are the prolongations of fascia transversalis?
- Over femoral vessels as anterior wall of femoral sheath.
- At the deep inguinal ring, over the spermatic cord as internal spermatic fascia.
Q.15 Why the cutting of one or two nerves supplying rectus produces clinical ill effects but not that of lateral abdominal muscles?
Because lateral abdominal muscles are supplied by a richly communicating network but the segmental nerve supply of rectus has little cross communications.
REGIONS OF ABDOMEN
Q.1 How is the abdomen divided into various regions?
Abdomen is divided into nine regions by:
- Two vertical planes:
Right and left lateral planes.
Passing from mid inguinal point and crossing the tip of ninth costal cartilage and passing up to midpoint between medial and lateral ends of the clavicle (midclavicular lines). - Two horizontal planes:
– Transpyloric plane:
Passes through the tip of 9th costal cartilage and lower border of L1.
It lies between the upper border of manubrium sterni (suprasternal notch) and the upper border of the symphysis pubis.
– Transtubercular plane:
Passes through tubercle of iliac crest and body of L5 vertebra near the upper border. - Two additional transverse planes have been described:
– Subcostal plane:
Can be used in place of a transpyloric plane. Passes through the lower border of 10th costal cartilage, i.e. lowest part of the costal margin and upper part of the body of L3.
– Supracristal plane:
Lies at the level of the highest point of iliac crests and it passes posteriorly through the spine of L4 vertebra.
Q.2 What is ‘linea semilunaris’?
It is a curved line from the pubic tubercle to the tip of 9th costal cartilage, present on the lateral edge of the rectus abdominis muscle.
Q.3 Name the structures lying at the level of L1 vertebra.
- Transpyloric plane
- Pylorus
- Duodenojejunal flexure
- Pancreas
- Hilum of kidneys.
Q.4 Name the structures lying at the level of L5 vertebra.
- Inter (trans) tubercular plane
- Common iliac veins end
- Inferior vena cava begins.
Q.5 Name the structures lying at the level of L2 vertebra.
- Spinal cord ends
- Thoracic duct begins
- Azygous vein begins.

Comments (0)