Nerve Supply of Upper Limb (Viva)
MUSCULOCUTANEOUS NERVE
Q.1 What is the origin of the musculocutaneous nerve?
It is a branch of the lateral cord of the brachial plexus, arising at the lower border of pectoralis minor (C5,6,7).
Q.2 What are the branches of the musculocutaneous nerve?
Muscular: To
- Coracobrachialis
- Biceps and
- Brachialis Cutaneous: It continues as the lateral cutaneous nerve of the forearm and supplies the skin of the lateral side of the forearm.
Articular: To elbow joint Communicating: To radial nerve, posterior cutaneous nerve of forearm, and palmar cutaneous branch of the median nerve.
Q.3 What will be the effect of the lesion of the musculocutaneous nerve?
Motor loss:
There will be paralysis of the biceps, coracobrachialis, and the medial part of brachialis, the lateral part being supplied by the radial nerve.
Effects:
- Flexion of the elbow joint will be weak but is still possible,
– With the forearm supinated due to the action of the unaffected lateral part of the brachialis and superficial flexors and
– In the prone or mid prone position by the brachioradialis and extensor carpi radialis longus.
- There will be very weak supination with the elbow flexed at 90°.
- There will be loss of biceps jerk
- There will be muscle atrophy.
Sensory loss:
Will be present over the lateral half of the forearm but the area will be less due to the overlapping of the intact adjacent cutaneous nerves.
MEDIAN NERVE
Q.1 What is the origin of the median nerve?
Median nerve is formed by the union of a medial root (C8, T1) from the medial cord and lateral root (C5,6,7) from the lateral cord.
Q.2 Name the branches and structures supplied by the median nerve?
In arm:
- Muscular branch to pronator teres
- Vascular branches to brachial artery
In forearm:
- Muscular branches to flexor carpi radialis, palmaris longus, flexor digitorum superficialis.
- Anterior interosseous branch to flexor pollicis longus, lateral half of flexor digitorum profundus, pronator quadratus and to distal radioulnar and wrist joints.
- Palmar cutaneous branch, to skin over thenar eminence and middle of the palm.
- Articular branch to elbow and proximal radioulnar joints.
- Vascular branches to radial and ulnar arteries.
- Communicating branch to ulnar nerve.
In hand:
- Muscular branches to abductor pollicis brevis, flexor pollicis brevis, opponens pollicis and first and second lumbrical
- Cutaneous branches to skin of lateral 3½ digits (Palmar digital branches).
Q.3 What will be the effect of a lesion of the median nerve at the wrist?
- Motor loss:
There will be paralysis of the thenar muscles and the 1st and 2nd lumbricals.
Effect:
– There will be loss of opposition of the thumb due to paralysis of the opponens pollicis
– Abduction of the thumb will not be greatly affected due to intact abductor pollicis longus which is supplied by the radial nerve
– Paralysis and wasting of the thenar muscles and unopposed extension by extensor pollicis longus and adduction by adductor pollicis will be rise to ‘apethumb’ deformity.
- Sensory loss:
There will be loss of sensation over the thumb, adjacent 3½ fingers, and the radial two-thirds of the palm.
Effect:
The sensory loss will prevent the accurate and delicate adjustments which the hand makes in response to tactile stimuli.
Q.4 What is ‘carpal tunnel’ syndrome?
This is a neuropathy resulting from compression of the median nerve as it passes beneath the flexor retinaculum through the carpal tunnel.
It causes:
• Motor loss:
Progressive weakness and wasting of thenar muscle
• Sensory loss:
In lateral 3½ digits.
RADIAL NERVE
Q.1 What is origin of the radial nerve?
It is a branch of the posterior cord of brachial plexus with a root value of C5,6,7,8 T1.
Q.2 What are the branches and distribution of radial nerve?
- Muscular branches: To
– Triceps
– Anconeus
– Brachialis,
Only lateral part of
– Brachioradialis and
– Extensor carpi radialis longus
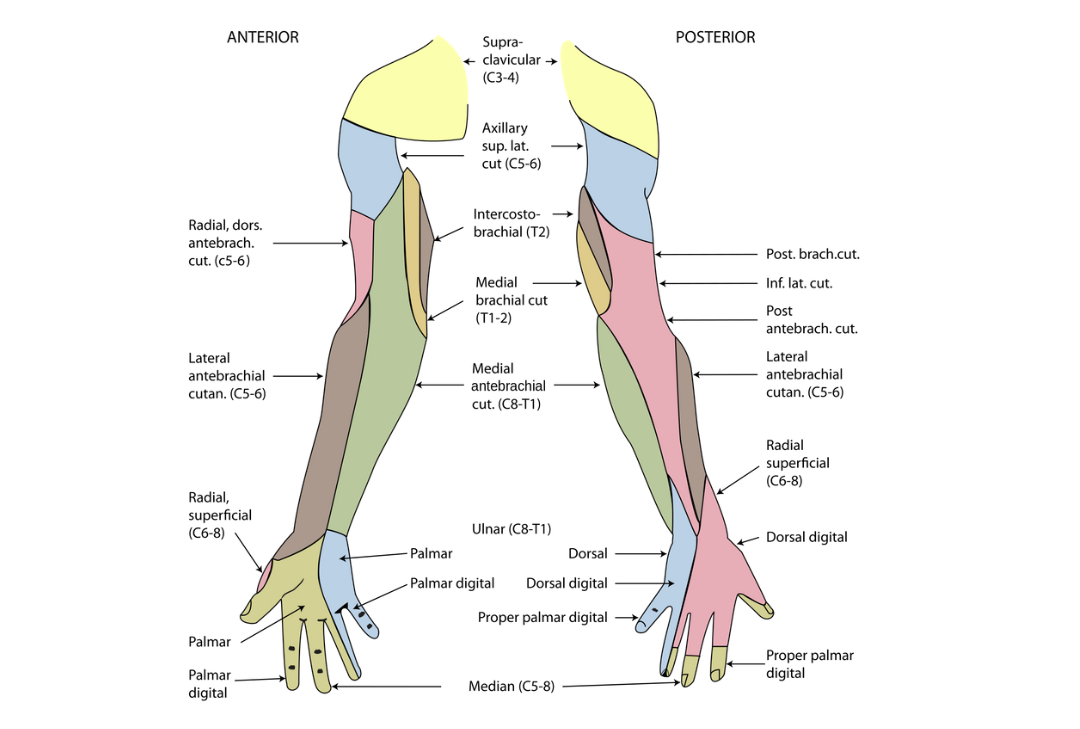
- Cutaneous branches:
– Lower lateral cutaneous nerve of arm
– Posterior cutaneous nerve of forearm
– Posterior cutaneous nerve of arm
– Dorsal digital branches from superficial terminal branch
- Articular branches: To elbow and wrist joint.
Q.3 What are the structures supplied by the posterior interosseous nerve?
Muscular branches:
- Extensor carpi radialis brevis
- Supinator
- Extensor digitorum
- Extensor digiti minimi
- Extensor carpi ulnaris
- Extensor pollicis longus
- Extensor indicis
- Abductor pollicis longus
- Extensor pollicis brevis
Q.4 What is the commonest site of radial nerve injury? What are the common causes of lesions?
In the region of radial (spiral) groove of the humerus.
The common causes of injury are:
- Fracture of shaft of humerus
- Intramuscular injections in arm
Q.5 What are the effects of the lesion of the radial nerve in the spiral groove?
- Triceps are not paralyzed since the branches supplying arise from the radial nerve more proximally.
- There is wrist drop, i.e. hand is flexed at the wrist and it lies flaccid due to the paralysis of the extensors of the wrist. The fingers are also flexed and when an attempt is made to extend them, the last two phalanges only will be extended, through the action of lumbricals and interossei.
- Supination is completely lost when the forearm is extended on the arm, but is possible to a certain extent if the forearm is flexed to allow effective action of the biceps.
Q.6 What will be the effect of cutting the radial nerve just below the elbow?
Sensory loss:
It is marked on the lateral part of the dorsum of the hand.
Motor loss:
- Wrist drop
- Loss of power of supination
- Extension of elbow is retained because of the intact triceps
- Flexion of elbow in normal position will also be retained because of intact biceps brachii and brachioradialis.
Q.7 What is the ‘high’ and ‘low’ radial nerve palsy?
When radial nerve is damaged above the origin of nerve to brachioradialis which arises above the elbow joint then it is called ‘high’ radial nerve palsy.
When radial nerve is damaged below the origin of nerve to brachioradialis then it is called ‘low’ radial nerve palsy. The brachioradialis is not paralyzed and causes flexion of the elbow joint in the mid prone position which when the elbow is flexed against resistance becomes prominent, can be felt superficially on the lateral aspect of the forearm.
ULNAR NERVE
Q.1 What is the origin of the ulnar nerve?
It arises from the medial cord of brachial plexus C8, T1.
Q.2 What are the branches of ulnar nerve?
In forearm:
- Muscular:
To flexor carpi ulnaris and medial half of flexor digitorum profundus. - Palmar and dorsal cutaneous branches:
In hand: - Muscular: –
By deep terminal branch: Abductor digiti minimi, flexor digiti minimi, opponens digiti minimi, medial two lumbricals, palmar and dorsal interossei and adductor pollicis
Palmaris brevis by palmar cutaneous or superficial terminal branch. - Articular: To elbow joint.
- Skin: Medial 1½ fingers by palmar digital branches.
Q.3 What will be the effect of a lesion of the ulnar nerve at the wrist?
- Motor loss:
There will be paralysis of all the intrinsic muscles of the hand (except those supplied by the median nerve), i.e. all interossei, 3rd and 4th lumbricals, hypothenar muscles, and adductor pollicis.
Effect:
- There will be ‘Mani-en-griff’ deformity or ‘clawing’ of the ring and little fingers. These fingers are hyperextended at the metacarpophalangeal joints (due to the unopposed action of the extensor digitorum as the 3rd and 4th lumbricals and all the interossei are paralyzed) and flexed at the interphalangeal joints (due to the unopposed action of the long flexors).
- Abduction of 2nd to 5th fingers will be weak due to paralysis of the dorsal interossei and abductor digiti minimi.
- There will be a loss of power of the adduction of the fingers due to paralysis of the palmar interossei.
- There will be a loss of power of the adduction of the thumb due to paralysis of the adductor pollicis.
- There will be wasting of the hypothenar eminence in long-standing injuries.
- There will be hollowing between the metacarpal bones, clearly apparent on the dorsum, due to atrophy of the interossei muscles in long-standing injuries.
- Sensory loss:
- There will be sensory loss on the medial side of the palm and the palmar surfaces of the little and the medial half of the ring fingers and on the dorsal aspect of the distal and middle phalanges of these fingers
- There will be no sensory loss over the dorsum of the hand as the dorsal cutaneous branch of the ulnar nerve will escape the injury. If the nerve is damaged proximal to the origin of this branch, then there will also be sensory loss over the dorsum of the hand.
Q.4 What will be the effect of a lesion of the ulnar nerve at the elbow?
- Motor loss:
- Same as when the nerve is damaged at the wrist.
- There will also be paralysis of the medial half of the flexor digitorum profundus supplying the little and ring fingers and of the flexor carpi ulnaris.
Effect:
- Same as when the nerve is damaged the wrist. ‘Clawing’ of the ring and little fingers will be less marked as their distal phalanges are not flexed due to paralysis of only the medial half of the flexor digitorum profundus.
- Loss of power in the flexor carpi ulnaris will result in weak flexion with radial deviation of the wrist.
- Sensory loss will be present over the ulnar 1½ fingers and the hand.
- Vasomotor and trophic changes will be present in the skin over the hypothenar eminence and little finger which will appear cold and dry and at times discolored. The nail of the little finger may be deformed.
Also read: Anatomy Question Collection
Also read: Anatomy Questions & Answers
Also read: Anatomy notes

Comments (0)