Bones
5 years ago 7409
| 1. Bone cells • Osteocytes • Osteoblast • Osteoclasts |
| 2. Extracellular matrix • Organic - Type-I collagen fibers - Protein - Glycosaminoglycans (Mucopolysaccharides) |
|
• Inorganic
- Abundant calcium & phosphorus |
| Membranous bone Ex: Most of the flat bone |
| Cartilaginous bone Ex: All the long bones |
| Compact bone Ex: Shaft of typical long bone |
| Spongy or cancellous bone Ex: Each end of a typical long bone |
| Axial skeleton Ex: Skull, ribs, sternum & vertebrae |
| Appendicular skeleton Ex: Bones of limbs |
| 1. Long bone →Typical long bone
Ex: Humerus, radius, ulna, femur, tibia, fibula
→Miniature long bone Ex: Metacarpals, metatarsals, Phalanges →Modified long bone
Ex: Clavicle
|
|
2. Short bone
Eg. Carpal & tarsal |
|
3. Flat bone
Eg. Scapula, sternum, ribs, parietal, frontal |
| 4. Irregular bones Eg. Vertebrae, hip bone |
| 5. Pneumatic bones Eg. Maxilla, sphenoid, ethmoid |
|
6. Sesamoid bone
Eg. Patella, pisiform
|
| • Regulate phosphate metabolism • Maintain homeostasis of blood calcium. Plays a role in the removal or deposition of calcium when required. |
|
• Maintains bone tissue
• Responsible for hormones controlling bone growth & development |
| • Outer fibrous layer: Consists of dense fibrous connective tissue with a network of blood vessels, lymphatics & nerves |
| • Middle vascular layer |
| • Inner osteogenic layer: Consists of more loosely arranged connective tissue, collagenous fibers with connective tissue cells (osteoprogenitor cells) |
| • It provides a media for the attachment of the muscles, tendons, ligaments, etc. |
| • Responsible for regeneration of bone (as osteoprogenitor cells present with enough blood supply) |
| • As it is more vascular, it forms a vascular bed from which it sends capillaries to supply the underlying bone |
| • Prevents overgrowth of bone • Helps in bone formation • Protection of bone |
| Role of periosteum in the growth of long bone: |
| • Periosteum consists of a dense fibrous outer layer of collagen bundles & fibroblasts. • The innermost cellular layer of the periosteum contains mesenchymal stem cells called osteoprogenitor cells, which divide by mitosis & differentiate into osteoblasts. • Osteoprogenitor cells play a prominent role in bone growth & repair. So, periosteum plays a role in new bone formation. |
| Elongated shaft (called as diaphysis) with two expanded ends on either side of the shaft (called as epiphysis). |
| One shaft & Two epiphysis |
| The medullary cavity is present in the shaft which contains bone marrow. |
| Only one primary ossification center |
| Two or more than two secondary ossification centre. |
| Eg. Humerus, radius, ulna, femur, tibia, fibula |
| Quite smaller in appearance than typical long bone |
| One shaft & only one epiphysis (only one expanded end/epiphysis) also called as head here. |
| Primary Ossification center lies on head/epiphysis/expanded end. |
| Only one secondary ossification center. |
| Eg. Metacarpals, Metatarsals, Phalanges |
| Devoid of medullary cavity |
| Mostly ossify in membrane |
| Two primary ossification centers |
| Two or more than two secondary ossification center |
| Eg. Clavicle, body of vertebrae |
| • Cuboidal in shape & presents six surfaces. |
| • Out of these four surfaces are articular & the remaining two surfaces give attachment to muscles, ligaments & are pierced by blood vessels. |
| • Eg. Carpal & tarsal bones |
| • Consists of two outer plates of compact bone with middle sponge bone containing marrow. |
|
• In term of skull called as
- Inner & outer tables of compact & - Middle layer of diploe
|
| • Intervening spongy tissue in the bones of the vault of the skull, is known as the diploe. |
| Eg: Most of the bones of the vault of the skull, sternum, ribs, sternum, scapula |
| Sphenoid bone | Sphenoid sinuses |
| Maxilla | Maxillary air sinuses |
| Ethmoid | Ethmoidal air sinuses |
| Frontal | Frontal air sinuses |
| • Develop in the tendon of muscles |
| • Ossify after birth |
| • Devoid of periosteum |
| • Absence of Haversian system |
| Metaphysis is present between the epiphysis & diaphysis that contain the Epiphyseal plate (growth plate) which is of hyaline cartilage in a growing bone. |
| When the bone stops growing, this growth plate/Epiphyseal plate is replaced by osseous tissue & the Epiphyseal plate is demarcated by Epiphyseal line. After the cessation of the growth plate, no further longitudinal growth of bone occurs. |
| • It is the cartilaginous end where the secondary center appears first & unites last with the diaphysis. |
| • Growing end of long bone is present in the area of epiphysis that appears 1st & fuses last. |
| • Relatable to law of ossification. |
| • It is situated against the direction of the nutrient foramen of that bone. |
| • Humerus - Down toward the elbow |
| • Radius & Ulna - Up toward the elbow |
| • For humerus - Upper end (toward the shoulder end) |
| • For radius & ulna - Lower end (toward the wrist end) |
| • Femur - Upward away from knee |
| • Tibia & Fibula - Downward away from the knee |
| • Knee ends of femur, tibia & fibula i.e |
|
(Lower end of femur) &
(Upper end of tibia & fibula) |
|
Even though Tibia doesn't follow the law of ossification,
but still, the upper end of the tibia is growing end. |
|
“To the elbow I go, from the knee I flee”
(Toward the elbow, away from knee)
|
| • The Epiphyseal center which appears first, unit last with the diaphysis & vice-versa. |
| • That means epiphysis that ossify first fuse with diaphysis last & the epiphysis that ossifies last fuses first with diaphysis except fibula. |
| • Secondary ossification center appears first in the lower end, |
| that means epiphysis of lower end of fibula ossify first but also fused with diaphysis first. |
| • As the upper epiphysis of fibula fused last, the upper end of the fibula is the growing end of the fibula as usual. |
| • There is no violation in determining the growing end. It's same for all long bones (opposite to the direction of nutrient foramen) |
| • Epiphysis develops from the secondary ossification center. |
| • Diaphysis (shaft) develop from the primary ossification center. |
| The primary ossification center is that from where, the bone starts ossified which appears before birth. |
| The primary ossification center is that from which, the main part of the bone is ossified & is appears before birth, usually during the 8th week of intrauterine life, which forms diaphysis (later called as the shaft of a long bone). |
| The secondary ossification center is that from which accessory part of a bone is ossified & is appears mostly after birth, which forms the epiphysis. |
|
• In typical long bones, the shaft (diaphysis) is chiefly compact bone surrounding a medullary cavity.
Medullary cavity present within diaphysis (shaft) contains yellow bone marrow - (contain fat store cells). |
|
• In typical long bones, the expanded end called epiphysis is composed of spongy bone.
Red Bone Marrow is present within the spaces of spongy bone. |
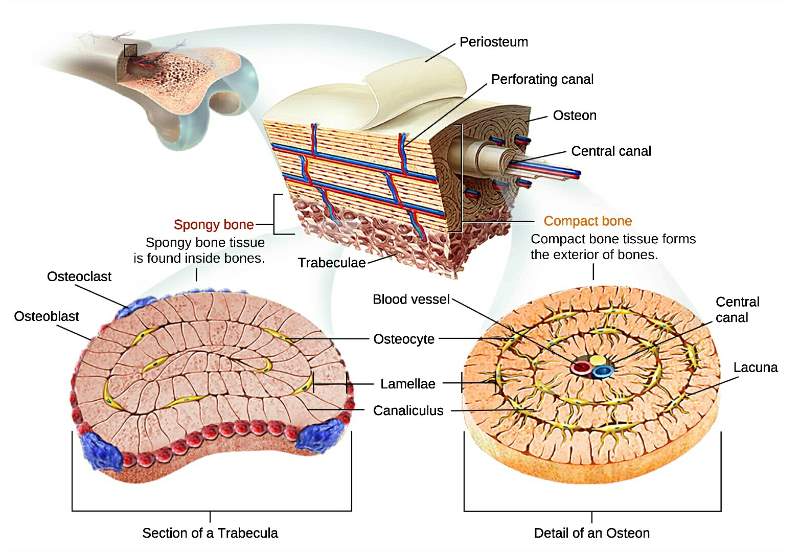
| Compact bone | Spongy bone |
| Compact bone has developed Haversian system. | Spongy bone has no developed Haversian system. |
| Shows dense area generally without any cavities | Shows areas with numerous interconnecting cavities. |
| Red Bone Marrow converted to Yellow Bone marrow present within the medullary cavity in adult age. | Red Bone marrow within the numerous marrow spaces persist throughout the life. |
| It is tortuous before entering the bone, so that it is not damaged during muscular contraction. |
| Enter the medullary cavity where it divides into ascending & descending branches. |
| Each branch anastomoses with the Epiphyseal, metaphyseal & periosteal arteries. |
| Long longitudinal central canal of Haversian system |
| Surrounded by 4-10 concentric lamellae |
| Contain blood vessels, nerves & loose connective tissue |
| Haversian canal is connected with the medullary cavity & with the outer surface of bone by numerous oblique channels known as Volkman's canal. |
| Contain small artery & nerves |
| Each Haversian canal is surrounded by 4-10 concentric lamellae. |
| Made up of bony matrix. |
| Composed of Type-I collagen fibers. |
| Small spaces between the lamellae |
| Contain only one osteocyte. |
| Fine radiating channels |
| Connect the lacunae with each others & Haversian canal |
| Contain branches of blood vessels & cytoplasmic process of osteocyte. |
| Periosteum | Endosteum |
| Cover the external surface of the bone except articular surface which is covered by hyaline cartilage | Cover the internal surface around the medullary cavity |
| Consists of outer fibrous & inner osteogenic layers | Consists of a single layer of flattened osteoprogenitor cells |
| Thicker than endosteum | Thinner than periosteum |
| Bone | Cartilage |
| The intercellular matrix is calcified, so it is hard. | The intercellular matrix is uncalcified, so it is soft. |
| Highly vascular | Avascular |
| Nerve supply present | No nerve supply |
| Bones are arranged in a definite pattern termed as the Haversian system. | No definite pattern of arrangements. |
| Outer covering called the periosteum. | Outer covering called Perichondrium. |
| • Found in fetal & young bones. • Active in the production of blood cells. |
| • With increasing age, it converts into yellow marrow. |
| • In newborns, the entire skeleton is occupied by the red bone marrow. |
| • By the age of 20, red marrow is found only in diploe (middle spongy layer) of skull bones, in the ribs, sternum, vertebrae, & in the spongy part at the expanded end of long bones. |
| • At the age of 20, all the marrow of long bones of the body becomes yellow except the proximal epiphysis of the femur & humerus. |
| • It consists mainly of adipose cells with an admixture of macrophages, undifferentiated mesenchymal cells & reticular cells. |
| • Production of blood cells |
| • Destruction of RBC (act as part of the reticuloendothelial system) |
| • Store iron in the form of ferritin & haemosiderin |
| • Play a role in the inactivation of toxins or other toxic substances of the body. |
| • Performs immunological functions. |
| Develop from mesoderm - undifferentiated mesenchymal cells |
|
It is composed of three elements of connective tissue
ie. Cells, Fibers & ground substances.
|
| Intercellular matrix (fibers & ground substances) are maximum & cellular substances are minimum. |
|
Fracture of a bone - destroy of bone matrix & bone cells adjoining the fractures
↓
Damaged blood vessels cause hemorrhage & form a blood clot. ↓
Blood clot, cells & damaged bone matrix are removed by macrophages. ↓
Proliferation of periosteum & endosteum, forming tissue around the fracture. ↓
Primary soft bone is formed by endochondral & membranous ossification. ↓
Further repair produces irregularly formed trabeculae of primary soft bone that temporarily unite the edges of the fractured bone, forming a hard bone callus. |
| • Decalcification of bone may be caused by excessive production of parathyroid hormone (hyperparathyroidism), which can cause increased osteoclastic activity, |
| • intense resorption of bone, elevation of blood calcium & phosphate levels |
| • & abnormal deposition of calcium in the arterial walls & kidneys (leading to kidney stone) |
Comments (0)