CARTILAGE
Cartilages are the specialized type of connective tissue composed of cells & extracellular matrix (fibers & ground substances).
• It is devoid of blood vessels, & nerve supply.
Thus, the healing of cartilage is quite slow.
Components:
1) Cells
• Chondroblasts (immature)
• Chondrocytes (mature) |
| * Chondroblasts → responsible for synthesis of extracellular matrix. |
2) Extracellular matrix
• Ground substance
Mainly composed of
- Glycosaminoglycans (GAG)
- Water & electrolyte |
• Fibers (collagen & elastic fiber)
Fibrocartilage & Hyaline
→ Type-II collagen fibers
|
Elastic cartilage
→Elastic fibers |
Peculiarities of cartilage• Devoid of nerve supply• Avascular, get nutrition from blood vessels of adjacent tissues by diffusion.• Matrix is not calcified like in bone.
Functions of cartilage
• Supports the soft tissues of the body
• Shock absorber
• Sliding area for joints & facilitates bone movements.
• Growth & developments of long bones before & after birth.
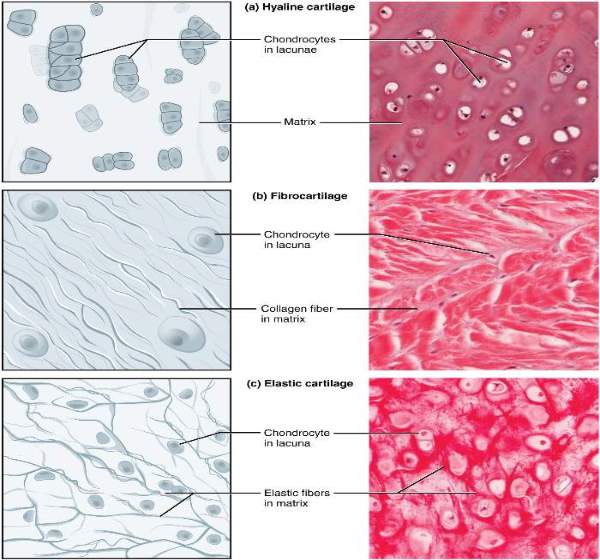
Types of cartilage:
- Hyaline cartilage
- Fibrocartilage
- Elastic cartilage
Distribution of cartilage:
Hyaline cartilage
| • Articular cartilage (cartilage around articular surface of bone) |
| • Costal cartilage of ribs which articulate with the sternum |
| • Thyroid & cricoid cartilage of larynx |
| • Epiphyseal plate of Growing long bone |
| • In the walls respiratory tract i.e nose, larynx, trachea, bronchi |
Fibrocartilage
| • Annulus fibrosis of intervertebral disc |
| • Symphysis pubis |
| • Menisci (present in knee joint) |
| • Glenoid labrum (of shoulder joint socket) |
| • Acetabular labrum of the hip joint socket |
| • Articular discs of temporomandibular joint & wrist joint |
Elastic cartilage
| • Auricles or pinna of external ear |
| • Cartilaginous part of external auditory canal |
| • Auditory tube (Eustachian tube) |
| • Epiglottis, cuneiform & corniculate cartilage of larynx |
Articular disc
It is the fibrocartilagenous structure, intervening between the articular surfaces in synovial joints.
Present in
• Temporo-mandibular joint (TMJ)
• Wrist Joint (Radio-carpel joint)
• Sternoclavicular joint
| * Articular discs present in the wrist joint (radio-carpel joint) prevent ulna for making wrist joint. |
| * Articular discs of the Temporomandibular joint divide the joint cavity into two compartments. |
Articular cartilage:
It is a special type of hyaline cartilage that covers the articular surfaces of the bones of most synovial joints.
• In some cases, where the bone is ossified in membrane, the cartilage is fibrocartilage
• Absence of perichondrium in articular cartilage
• Acts as shock absorbers & ensures gliding movement
Intervertebral disc:
The two adjacent vertebral bodies are united to each other by a special type of connective tissue called an intervertebral disc.
Two parts
• Annulus fibrosus (outer layer of fibrocartilage)
• Nucleus pulposus (inner mass of gelatinous materials, rich in hyaluronic acid)
Function
1. Allow certain movements between the vertebrae.
2. Acts as a shock absorber.
3. Protect the friction of the corresponding vertebrae.
| • Annulus fibrosus, a type of fibrocartilage developed from mesenchyme. |
|
• Nucleus pulposus developed from notochord.
Nucleus pulposus represents notochord.
|
Disc prolapse:
Dislocation or herniation of intervertebral disc from its position between the vertebrae.
• Due to a reduction in proteoglycan size within the nucleus pulposus diminishes its viscoelasticity leading to focal damage.
• Most common at L 4 & L 5 due to increased mechanical forces across this area.
Just to know:
Mode of nutrition of cartilage:
• Cartilage is devoid of blood vessels
• Hyaline cartilage cells metabolize glucose mainly by anaerobic glycolysis to produce lactic acid.
• Hyaline & elastic cartilage → From vessels of perichondrium
• Fibrocartilage → From blood vessels of surrounding connective tissue
• Articular cartilage → From synovial fluid
Histology of Elastic cartilage: -
• Yellowish in appearance due to the presence of elastic fibers.
• Composed of-
1. Cells
• Chondrocytes &
• Chondroblasts |
2. Extracellular matrix
• Fibers- Elastic fiber
• Ground substance |
• Chondrocytes are present in the space called lacunae.• Perichondrium present• Elastic fibers form branching & anastomosing network• It's composition is similar to hyaline cartilage except that it contains elastic fibers instead of collagen type-II fibers.
Histology of fibrocartilage:
• Fibrocartilage is a tissue intermediate between dense connective tissue & hyaline cartilage.
• Cells lies in rows between collagen fiber bundles
• Long, parallel, wavy bundle of collagen fibers present
• No distinct perichondrium
Histology of Hyaline Cartilage
• Weakest cartilage of all
• Matrix around the cells → deeply stained called as territorial matrix.
• Inter-territorial matrix (lightly stained) → present between two groups of cells
• Chondrocytes lie in space called lacunae forming groups of cells called isogenous aggregates.
• Composed of-
| Cells → Chondrocytes & Chondroblast |
| Fibers → Type-II collagen fibers |
| Ground substances |
• Perichondrium present• Chondrocytes appear in the space called lacunae.
Tips:
|
A lacunae contains either single cells or multiple cells.
Collection of lacunae group of cells called isogenous aggregates.
|
| • Chondrocytes synthesize collagens & the other matrix molecules. |
| * Hyaline & Fibrocartilage contain Type-II type of collagen fibers but elastic cartilage contains elastic fibers. |
| * Perichondrium is absent in articular cartilage & Fibrocartilage. |
Perichondrium:
• Its a sheath of dense connective tissue that surrounds the cartilage.
• Not found in articular cartilage & fibrocartilage
Two layers present
| Outer fibrous layer (Vascular) |
| Inner chondrogenic layer (Cellular) |
Composed of Type-I collagen fibers, fibroblasts & chondrocytes in inner layers.
Functions
• It harbors the vascular supply for avascular cartilage.
• Cells around the Perichondrium has the capacity to regenerate to some extent in case of cartilage damage.
• It contains nerves & lymphatic vessels.
Cartilage Formation/ Chondrogenesis:
| • All cartilage derived from the embryonic mesenchyme. |
| • The mitotic proliferation of mesenchymal cells occurs which later differentiate into chondroblasts |
| • Chondroblasts secrete the components of extracellular matrix & form lacunae and become chondrocytes. |
| • Chondrocytes divide one or two times within lacunae to form isogenic groups. |
| • Each chondrocytes secrete their own matrix causing it to form its own lacunae and separate apart. |
| • The superficial mesenchyme develops into the Perichondrium. |
• Synthesis of matrix contributes greatly to the growth of the cartilage.
Comments (0)