Connective Tissue
5 years ago 7449
| • Intercellular matrix is maximum & cellular component is minimum |
| • Composed of cells & matrix (i.e fibers & ground substances) |
| • Mesodermal in origin |
| • Cells are widely scattered within the intercellular matrix. |
| • Only so-called connective tissue proper is not only connective tissue proper. |
| • Even bone, cartilage, blood & lymph are connective tissue & possess all the above characteristics. |
| • Only difference in what form, intercellular matrix exists. |
| Connective Tissue | Intercellular matrix |
| Connective Tissue Proper | Jelly-like, soft, Viscous |
| Cartilage | More than semi-solid |
| Bone | Solid |
| Blood & Lymph | Fluid type |
| A) Embryonic connective tissue 1. Mesenchyme: Give rise to all other connective tissues |
| 2. Mucous C.T (Wharton's Jelly): Present in umbilical cord |
| B) Adult connective tissue Derived from mesenchyme |
| 1. Connective tissue proper • Loose connective tissue - Areolar C.T - Adipose C.T - Reticular C.T |
| • Dense connective tissue - Regular C.T - Irregular C.T - Elastic C.T |
| 2. Supporting Connective tissue • Bone - Compact - Spongy |
| • Cartilage - Hyaline - Fibrous - Elastic |
|
3. Fluid connective tissue
• Blood • Lymph |
| • Only difference is the matrix of other connective tissue is soft, viscous but, |
|
• Matrix of cartilage → Semi-solid
• Matrix of bone → Solid |
| 1. Cells |
| 2. Extracellular Matrix (Intercellular matrix) • Fibers • Ground substances |
| Fixed cells (Stationary cells) • Non-motile |
| 1. Fibroblasts 2. Chondroblasts 3. Osteoblasts 4. Adipose cell 5. Mast cell 6. Pigment cell 7. Reticular cell |
| Wandering cells (migratory cells) • Motile, move one place to another |
| 1. Neutrophils 2. Eosinophils 3. Basophils 4. Monocyte 5. Lymphocyte 6. Plasma cells 7. Macrophage |
|
Types of WBC (Leukocyte)
• Neutrophils • Eosinophils • Basophils • Monocyte • Lymphocyte |
| These cells are usually present in blood. Thus they migrate with the blood fluid. |
| B-Lymphocyte later differentiate into antigen producing cells called plasma cells. |
| • Fibroblast | Connective tissue proper |
| • Chondroblast | Cartilage |
| • Osteoblast | Bone |
| Hematopoietic stem cells | Blood cells |
| Immature (blast) | Mature (cyte) |
| Fibroblast | Fibrocyte |
| Chondroblast | Chondrocyte |
| Osteoblast | Osteocyte |
| Hematopoietic stem cells | RBC, WBC, Platelets |
| 1. Fibroblasts synthesize protein such as collagen & elastin which form collagen, reticular & elastic fibers. (Fibro-fibers synthesis) |
| 2. It also synthesizes glycosaminoglycans (GAGs), proteoglycans, and glycoproteins of ground substance. |
| 3. They help in the healing of wounds by continued proliferation and simultaneous conversion into fibrocytes and cause scar formation. |
| Macrophages derived from bone marrow precursor cells that divide, producing monocytes which circulate in the blood |
| & cross the wall of venules & capillaries to penetrate the connective tissue, where they mature & acquire the morphological features of macrophages. |
| • They digest particular organic molecules, foreign bodies, pathogens by phagocytosis process. • Thus, helps in removing cell debris & damaged extracellular components |
| • Production of cytokines, chemotactic factors, & several other molecules that participate in inflammation, antigen presentation. |
| • They contribute to the immunological reactions of body • Macrophages are the main antigen-presenting cells. |
|
1) Fixed/Resting macrophages:
• These macrophages remain in a particular tissue. Example: Alveolar macrophage
Splenic macrophage
|
|
2) Wandering macrophages:
• In tissue, macrophage gets a special name. • Monocyte during infection or inflammation get to different tissue & get a different name.
|
| Site | Name of macrophages |
| Skin | Langerhans's cell |
| Connective tissues | Histiocytes |
| Brain | Microglia |
| Lungs | Alveolar macrophage |
| Liver | Kuffer's cell |
| Spleen | Red pulp & splenic macrophages |
| Lymph node | Reticular cells |
| Bone | Osteoclast |
| • Phagocytic cells occupying the endothelial lining & reticular space of connective tissue & mobile macrophages are collectively called reticulo-endothelial system. |
| • The total combination of monocyte, mobile macrophage, fixed tissue macrophages & few endothelial cells in bone marrow, spleen & lymph nodes is called reticulo-endothelial system. |
| • Also known as mononuclear phagocyte system • Macrophage system |
| In connective tissue → Histocytes |
| In blood → monocytes (precursors of macrophages) |
| In sinusoids of liver → Kupffer's cell |
| In the lymphoid tissue & lymph nodes → Reticular cells |
| In spleen → splenic & red pulp macrophages |
| In lung alveoli → Alveolar macrophages |
| In brain & spinal cord → Microglia |
| In bone → osteoclast |
| Mononuclear phagocytic cells are derived from precursor cells in the bone marrow. These precursors develop into monocytes and dendritic cells, phagocytic cells that are released into the bloodstream. Some monocytes and dendritic cells remain in the general circulation, but most of them enter body tissues. In tissues, monocytes develop into much larger phagocytic cells known as macrophages. The great majority of macrophages remain as stationary cells within the tissue, where they filter out and destroy foreign particles. Some of them break away, however, and wander through the circulation and within the intercellular spaces. |
|
Cells of the mononuclear phagocyte system differ in appearance and name because of their various location.
For example,
Dendritic cells are found in many tissues, including the lungs, the skin, and the GIT, as well as throughout the lymphatic system.
Histiocytes are found in numerous subcutaneous tissues.
Kupffer cells line the sinusoids of the liver.
Microglia occur in nervous tissue, and alveolar macrophages are found in the air spaces of the lungs.
|
| The mononuclear phagocyte system plays an important role in the destruction of worn-out aging red blood cells and the recycling of iron. Specialized macrophages, primarily those residing in the bone marrow, liver, spleen, break down old red blood cells and metabolize the hemoglobin (oxygen-carrying protein), thereby freeing the iron compound heme for the production of new red blood cells. |
| Source: https://www.britannica.com/science/mononuclear-phagocyte-system |
|
Alveolar macrophage of lungs phagocytose the harmful product present in smoke.
That's why the smoker's lung seems to be black.
|
|
Macrophage beneath the skin → digest the color of the tattoo.
It is the reason your tattoo of body could fade out.
|
| • Liberate histamine and other chemical mediators during allergic and inflammation reaction & promote vasodilation and increased vascular permeability (swelling, inflammation). |
| • Heparin acts as an anticoagulant in function. |
| • Acts as storage of lipids chiefly triglyceride i.e esters of fatty acids & glycerol. • Acts as a cushion, shock absorber. |
| • Acts as an insulator, prevent excessive heat gain or loss through the skin. • Maintain the visceral position (e.g kidney) |
| • Fibroblast, chondroblast, osteoblast → Production of respective fibers & ground substances |
| - Fibroblast → for connective tissue proper - Chondro blast → for cartilage matrix - Osteoblast → for bone matrix formation |
| • Plasma cells → Production of antibodies |
| • Mast cell → secrete histamine for inflammatory response & heparin → for anticoagulation action |
| • Adipose cell → store of neutral fats (TAG), heat production |
| • Macrophage → phagocytosis of foreign harmful particles |
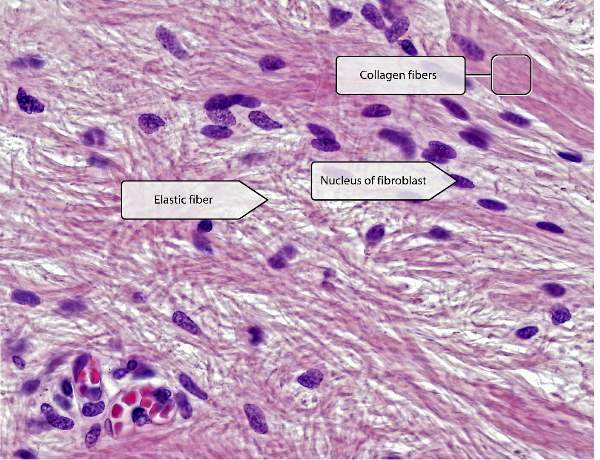
| • White protein fibers formed from collagen protein |
| • Produce from fibroblast |
| • Fibers are arranged in numerous straight or wavy bundles. • No branching present |
| • Non-elastic but has high tensile strength, to withstand strong tension. |
|
Type-I collagen fiber
About 90% of collagen fibers are of Type-I (chief constituents of organic part of bone) - Skin - Tendon - Ligament - Bone - Fascia - Scar tissue (that firm after wound healing) |
|
Type-II collagen fiber
- Fibrocartilage (i.e intervertebral disc) - Hyaline cartilage (i.e articular surface of joint, larynx, trachea)
|
| Type-III collagen fiber - Large blood vessels - Spleen - Liver - Kidney - Uterus - Smooth muscle |
| Type-V collagen fibers - Fetal tissue - Placenta |
| • Produced from a type of fibroblast called reticular cells. |
| • Composed of Type-III collagen fibers |
| • Fine short fibers which branch to form an extensive network for supporting soft tissues like liver, bone marrow and tissues of the lymphatic system |
| • Commonly known as the framework of lymphoid organs. |
| * Reticular cell, a type of fibroblast → that produces Type-III collagen fibers which are used to produce reticular fibers. So it seems Type-III collagen fibers & reticular fibers have common distribution. |
| • Yellow branching fibers composed of elastin protein, formed by fibroblast |
| • Highly elastic and give elasticity to the lungs, large blood vessels (i.e aorta) |
|
* For inspiration, diaphragm & external intercostal muscles act.
But for quite expiration, no muscles needed for active action.
|
|
• It occurs due to the elastic recoil tendency of the lung.
Elastic forces extended by the surface tension of the fluid lining of lung alveoli & elastic fibers of lungs.
|
| Type-I collagen fibers For tough structure • Bone • Tendon • Ligament |
| Type-II collagen fibers • Hyalin cartilage • Fibroelastic cartilage Elastic cartilage (has elastic fibers) |
| Reticular fibers • Lymphoid organs |
| Elastic fibers For those that need elasticity • Lungs • Large arteries for pumping action like heart. • Elastic cartilage |
| Epithelial tissue | Connective tissue |
| Defined as a collection of closely aggregated polyhedral cells with very little intercellular substance covering the external & internal surfaces of the body. | It is a group of tissues structurally composed of cells, fibers & amorphous ground substances derived from embryonic mesoderm & are responsible for providing & maintaining form in the body. |
| Derived from all germ layers | Derived from mesoderm (mesenchyme) |
| Generally devoid of blood vessels & get nutrition by diffusion from underlying blood vessels. | Present blood supply |
| Maximum cellular element & minimum intercellular substance | Maximum extracellular element & minimum cellular element |
| Functions: covering, absorption, secretion, sensory, lubrication |
Function: Mechanical, storage, defense, repair, transport & regeneration |
| • Ascorbic acid (vitamin C) is an important co-factor for proline hydroxylase (enzyme) for collagen synthesis • Vitamin C (ascorbic acid) is an essential cofactor during collagen biosynthesis. |
|
• The hydroxylation occurs during protein synthesis and requires ascorbic acid (vitamin C) as a cofactor.
• Deficiency of vitamin C leads to deficiency in proline hydroxylation leading to less stable collagen & causes the formation of defective collagen and leading to scurvy.
|
| • In scurvy, the collagen formed is unhydroxylated, relatively unstable, and subject to collagenolysis. |
| Collection of connective tissue which may appear as condensations on the surfaces of muscles. |
| Examples: • Clavipectoral fascia • iliotibial tract • Deep cervical fascia (fascia coil) |
| Closed connective tissue sac lined with a synovial membrane filled with lubricating fluid |
| Function: • Allows free movements • Helps in lubrication • Diminish friction |
Comments (0)