Rectal Prolapse vs Hemorrhoids
Hemorrhoids
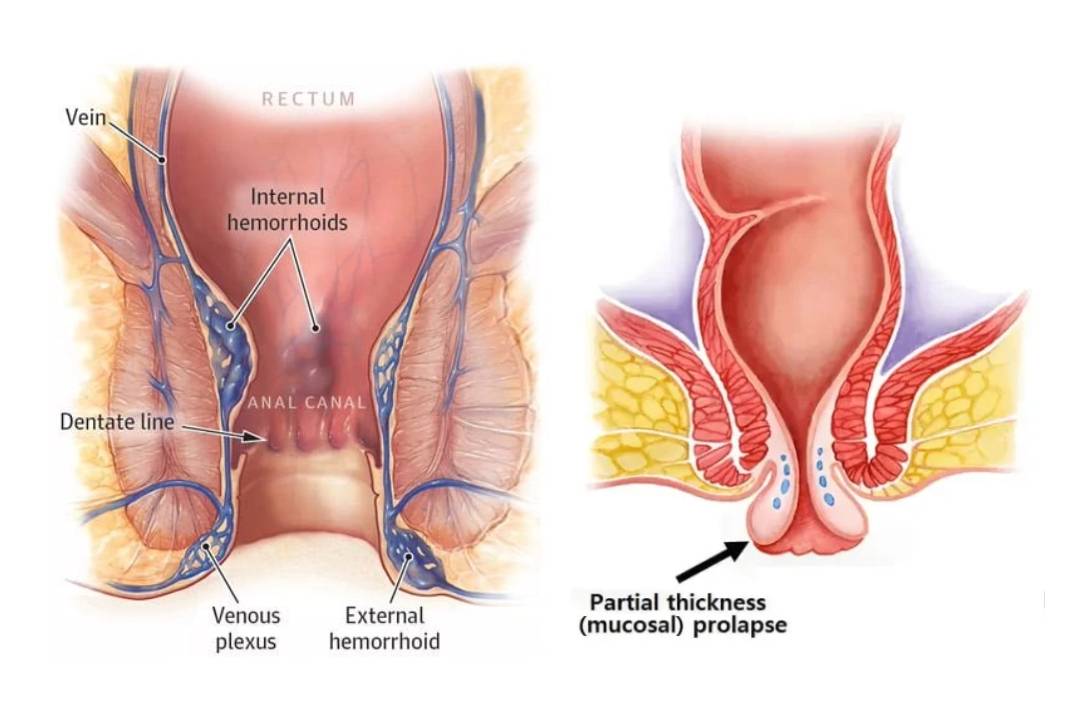
Hemorrhoids, also known as piles refer to symptomatic engorgement of veins in the lower part of the anal canal. Hemorrhoids can cause discomfort, pain, itching, and bleeding, although not all cases exhibit symptoms. Anal cushions position: 3 o'clock position, 7 o'clock position, and 11 o'clock position.
Types of Hemorrhoids:
There are two main types of hemorrhoids based on their location:
- Internal Hemorrhoids
- External Hemorrhoids
1. Internal Hemorrhoids: These lie above the dentate line, covered with mucus membrane, and are usually painless. They may cause bleeding during bowel movements, leading to bright red blood in the stool.
2. External Hemorrhoids: These lies below the dentate line covered with skin around the anus and can be painful. They may cause itching and discomfort, and sometimes, they can thrombose (develop blood clots).
3. Internal-external Hemorrhoids
Causes of Hemorrhoids:
Hemorrhoids occur due to increased pressure in the veins of the rectum or anus. The common causes of Hemorrhoids include:
- Straining due to constipation.
- Prolonged sitting or standing: Especially on the toilet for extended periods.
- Chronic diarrhea: Frequent bowel movements can put a strain on the rectal area.
- Pregnancy: Increased pressure on the pelvic area can lead to hemorrhoids during pregnancy.
- Obesity: Excess weight can increase pressure on the rectal veins.
- Low-fiber diet: Insufficient fiber intake can lead to constipation, exacerbating hemorrhoids.
Internal hemorrhoids:
Internal Hemorrhoids are above the pectinate line i.e. in the endodermal part with columnar epithelium so they are painless. Usually, the engorged and cushions prolapse and bleeding is the earliest symptom. So uncomplicated cases present with per rectal bleeding bright red. There can be mucus discharge & prolonged bleeding may lead to anemia. With prolonged time, itching can develop due to difficulty in maintaining hygiene. In complicated cases, there can be ulceration, thrombosis, gangrene, or fibrosis.
Grades of internal hemorrhoids
First degree: In 1st degree of Internal hemorrhoids, there can be prolapse of engorged anal cushions but only internally and does not come out of the anal verge. So there is only bleeding.
Second degree: In 2nd degree of Internal hemorrhoids, piles prolapse during defecation but return spontaneously.
Third degree: In 3rd degree of Internal hemorrhoids, piles prolapse during defecation and can be replaced back only by manual manipulation and does not reduce spontaneously.
Fourth degree: In 4th degree of Internal hemorrhoids, piles are completely prolapsed that cannot be reduced. It may even be strangulated with other complications.
External hemorrhoids
In external hemorrhoids, veins are engorged circumferentially. The external hemorrhoids lie below the pectinate line, i.e. ectodermal part with squamous epithelium. so they are painful due to pudendal nerve innervation. When they get eroded or they try to erode the skin then leads to bleeding. When chronic skin tags are produced then during defecation, the fecal matter may get trapped between them and leads to hygiene problem including itching. Usually, it resolves in 5-7 days.
Symptoms of hemorrhoids:
The symptoms of hemorrhoids may include:
- Bleeding: Bright red blood in the stool or on toilet paper after bowel movements.
- Pain or discomfort: Especially during bowel movements in the case of external hemorrhoids.
- Itching and irritation: Around the anus.
- Swelling and lump: In the anal area, particularly with external hemorrhoids.
- Leakage of feces: In more severe cases.
Diagnosis of Hemorrhoid:
To diagnose hemorrhoids, a medical professional will typically perform a visual inspection and digital rectal examination. For visual inspection and digital rectal examination, the position the patient in the left lateral decubitus position. External hemorrhoids are easily seen through visual inspection. In the case of internal hemorrhoids, prolapsed parts may be seen. Internal hemorrhoids are often not palpable on digital rectal examination if not palpable we cannot rule them out and thus they are best diagnosed with anoscopy or proctoscopy. In some cases, additional procedures may be used, such as anoscopy, sigmoidoscopy, or colonoscopy, to rule out other potential causes of rectal bleeding such as bulging, blue veins are seen.
Treatment of Hemorrhoids/Piles:
Treatment for hemorrhoids varies based on their severity. Common treatment options include:
• Lifestyle changes: Increasing dietary fiber or fiber alternatives like spagula husk, sterculia, methylcellulose, drinking plenty of water, and avoiding prolonged sitting or straining during bowel movements.
• Topical treatments: Over-the-counter creams, ointments, or suppositories may help relieve symptoms.
• Sitz baths: Soaking the buttocks area in warm water can provide relief.
• Para surgical procedures like doppler-guided hemorrhoidal artery ligation, sclerotherapy, infrared coagulation, barrons banding, cryosurgery, and laser therapy.
• Surgical procedures: oen hemorrhoidectomy, closed hemorrhoidectomy, stapled hemorrhoidopexy, anal stretching- lords, racemes.
Prevention of Hemorrhoids:
Medical professionals should advise patients on preventive measures to reduce the risk of developing hemorrhoids, including:
• Maintaining a high-fiber diet to prevent constipation.
• Drink plenty of water
• Avoid prolonged sitting or standing.
• Engaging in regular physical activity to improve bowel movement regularity.
Rectal prolapse
Rectal prolapse involves the protrusion or telescoping of the mucous membrane and submucosa of the rectum (the lower end of the large intestine) outside the anus approx 1-4 cm. On palpation of prolapsed mucosa between finger and thumb, it is evident that it is composed of no more than a double layer of mucous membrane. this helps to distinguish mucosal prolapse from full-thickness prolapse.
Types of Rectal Prolapse:
1. Full-Thickness Rectal Prolapse:
The entire thickness of the rectal wall protrudes through the anus. This type is the most severe.
2. Mucosal Prolapse:
Only the inner lining (mucosa) of the rectum protrudes through the anus. Mucosal prolapse is less severe than full-thickness prolapse.
3. Partial Prolapse (Internal Rectal Intussusception):
The rectum collapses upon itself, but it does not protrude from the anus. This type is often not visible externally and may only be detected during diagnostic tests.
Causes of Rectal Prolapse:
Rectal prolapse is often associated with weakened pelvic floor muscles and supportive tissues, leading to an inability to maintain the normal position of the rectum. Several factors can contribute to this weakening, including:
• Chronic Constipation: Straining during bowel movements over time can stress the pelvic floor muscles and rectal tissues.
• Chronic Diarrhea: Frequent bowel movements can also contribute to rectal prolapse.
• Childbirth: In women, the process of childbirth can stretch and weaken the pelvic floor muscles.
• Aging: As people age, the supportive tissues in the pelvis may naturally weaken.
• Neurological Disorders: Conditions that affect the nerves controlling the pelvic muscles can increase the risk of rectal prolapse.
Symptoms of rectal Prolapse:
The symptoms of rectal prolapse may include:
• Protrusion from the anus: A visible mass or lump that protrudes through the anus, especially during bowel movements.
• Discomfort or pain: Pain or discomfort in the rectal area, often relieved when the prolapsed tissue is repositioned.
• Difficulty with bowel movements: Feeling of incomplete evacuation or straining during bowel movements.
• Bleeding or mucus discharge: Some individuals may experience rectal bleeding or mucus discharge from the prolapsed tissue.
Diagnosis of Rectal Prolapse:
Diagnosing rectal prolapse typically involves a combination of medical history, physical examination, and sometimes diagnostic tests, such as defecography, sigmoidoscopy, or colonoscopy. These tests help confirm the presence of prolapsed tissue and determine the type and severity of the prolapse.
Treatment of Rectal Prolapse:
Treatment for rectal prolapse depends on the type and severity of the prolapse. Mild cases may be managed with conservative measures, such as dietary changes, fiber supplements, and pelvic floor exercises. In more severe cases, surgical intervention may be necessary to repair the weakened tissues and support the rectum.
A. MUCOSAL PROLAPSE:
Digital Positioning and submucosal injection or banding are done in infants and young children. Local treatments such as the injection of phenol in almond oil or the application of a rubber band and excision of prolapsed parts are done in adults.
B. FULL-THICKNESS PROLAPSE:
In Full thickness prolapse, surgery is required which can be done by perineal or abdominal approach. Abdominal rectopexy can be done either laparoscopically or open. By Perineal approach, Thiersch operation, Delorme operation, and Altemeier operation can be done.
Difference between Rectal Prolapse vs Hemorrhoids:
The key differences between hemorrhoids and rectal prolapse are:
- Hemorrhoids are swollen veins in the rectum or anus, whereas rectal prolapse involves the protrusion of the rectum through the anus.
- Hemorrhoids are caused by increased pressure on the rectal veins, while rectal prolapse is often related to weakened pelvic floor muscles and supportive tissues.
- Hemorrhoids may cause bleeding, pain, and itching, while rectal prolapse may present as a visible protrusion from the anus and can cause discomfort and difficulty with bowel movements.
- Tissue folds in hemorrhoids are radial whereas in rectal prolapse they are circumferential.
- On palpation in hemorrhoids, the abnormality is present in hemorrhoidal plexuses while in rectal prolapse double rectal wall is palpated
- On resting and squeeze pressure, hemorrhoids are normal while rectal prolapse increases.
Rectal Prolapse vs Hemorrhoids
The differences between Rectal prolapse and Hemorrhoids are given below.
| Hemorrhoids | Rectal Prolapse |
| Hemorrhoids are the engorgement of veins in the lower part of the anal canal. | Rectal prolapse involves the protrusion of the rectum outside the anus. |
| Hemorrhoids occur due to increased pressure on the rectal veins. | Rectal prolapse occurs due to weak pelvic floor muscles and supportive tissues. |
| Hemorrhoids may cause bleeding, pain, and itching. | Rectal prolapse causes visible protrusion from the anus with discomfort and difficulty of bowel movements. |
| Tissue folds in hemorrhoids are radial. | In rectal prolapse, tissue folds are circumferential. |
| On palpation, the abnormality is present in hemorrhoidal plexuses in hemorrhoids. | In rectal prolapse, the double rectal wall is palpated. |
| On resting and squeeze pressure, hemorrhoids are normal while rectal prolapse increases. | On resting and squeeze pressure, rectal prolapse increases. |

Comments (0)