Emergency drugs
Emergency drugs are those drugs used in medical emergencies i.e. acute life-threatening conditions that need immediate action with the aim to save the life of the patients. Emergency drugs are also called Life Saving Drugs.
Emergency drugs are commonly found in the Emergency ward, ICU (intensive Care Unit), CCU (Critical Care Unit), and Operation theatre. Emergency drugs are the backbone of life support in the emergency department.
Emergency drugs can be divided into two categories.
- The 1st category of emergency drugs is those drugs that are essential & most used and should be present in every department of emergency drug kit.
- The 2nd category of emergency drugs is those drugs that are useful but are optional depending upon the practitioners. Thus, the emergency drugs list may vary from hospital to hospital.
Medical emergencies are critical situations in which acute, sudden changes occur in the medical status of patients which endangers the patient’s life and needs immediate action & intervention. For this emergency drugs come into play.
Common medical emergencies are
- Vasovagal syncope
- Seizure
- Stroke
- Cardiac arrest
- Cardiac arrhythmia
- Angina
- Myocardial infarction (Heart Attack)
- Airway obstruction
- Asthma exacerbation
- Anaphylactic reaction
- Hypoglycemia
- Poisoning
- Shock
- Sepsis
- Trauma
Characteristics of emergency drugs
The main objective of emergency drugs is to save the life of a patient from life-threatening medical conditions. The characteristics of emergency drugs are:
- Rapid onset of action
- Short half-life & less side effects
- Parenteral Route of administration to ensure rapid absorption & distribution for rapid action
- Highly potent & effective
- Wide therapeutic wide (i.e. high safety margin)
- Stabilizing properties of vital signs
- Specific & clear dosing
One of the essential characteristics of emergency drugs is rapid onset of action & highly potent. Other characteristics of emergency drugs are discussed below.
1. Rapid onset of action
Emergency drugs are used in life-threatening conditions where every second counts, and thus need immediate action. So, emergency drugs must have a rapid onset of action i.e. should start its action within seconds to minutes.
2. Short half-life & less side effects
Short-acting drugs are preferred over long-acting drugs as emergency drugs because long-acting drugs may give long-term side effects. So, the patient’s condition may further deteriorate & patient also may die due to the side effects of drugs.
3. Parenteral Route of Administration
Most emergency drugs are available in injectable form. The intravenous route (IV route) is mostly used in emergency conditions for rapid onset of action without any delay as the bioavailability of the IV route is 100%. But other parenteral routes are also used in some special emergency conditions like the intramuscular route (IM route), Sublingual route, etc.
4. Highly Potent drug
Emergency drugs should be highly effective & specific in emergency conditions.
List of emergency drugs
The list & availability of emergency drugs may slightly vary from hospital to hospital & different health departments. The list of most commonly used essential emergency drugs are
- Epinephrine/Adrenaline
- Noradrenaline
- Dopamine
- Lidocaine
- Nitroglycerin (GTN)
- Amiodarone
- Adenosine
- Propranolol
- Metoprolol
- Digoxin
- Salbutamol
- Hydrocortisone
- Dexamethasone
- Calcium gluconate
- Dextrose
- Aspirin
- Atropine
- Naloxone
- Morphine
- Magnesium sulfate
- Furosemide
- Mannitol
- Lorazepam
- Diazepam
- Flumazenil
- Midazolam
- Sodium nitroprusside
- Diphenhydramine
- Aminophylline
- Potassium chloride
- Heparin
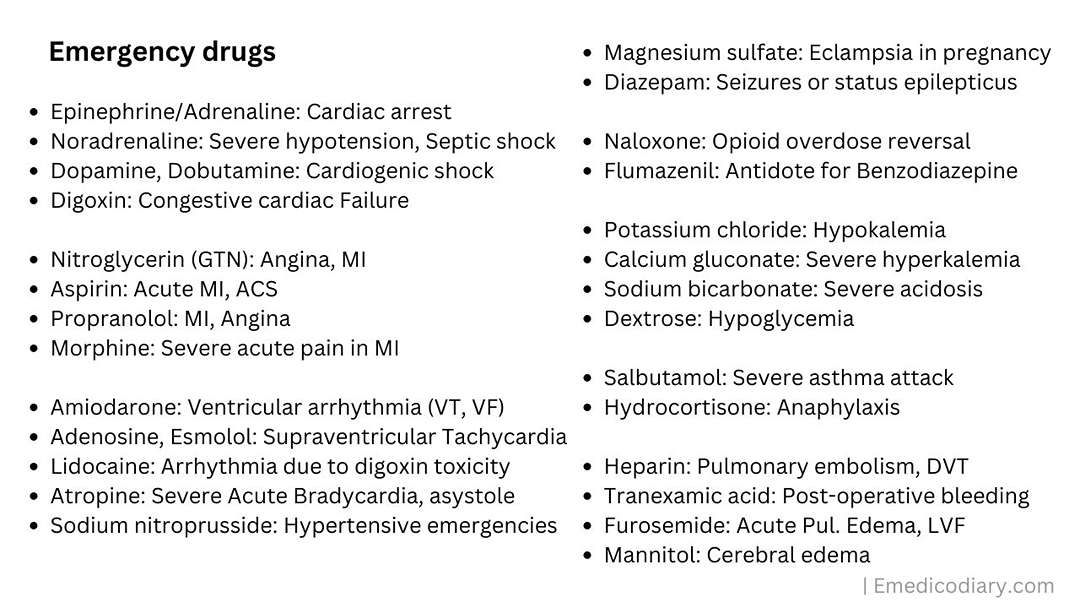
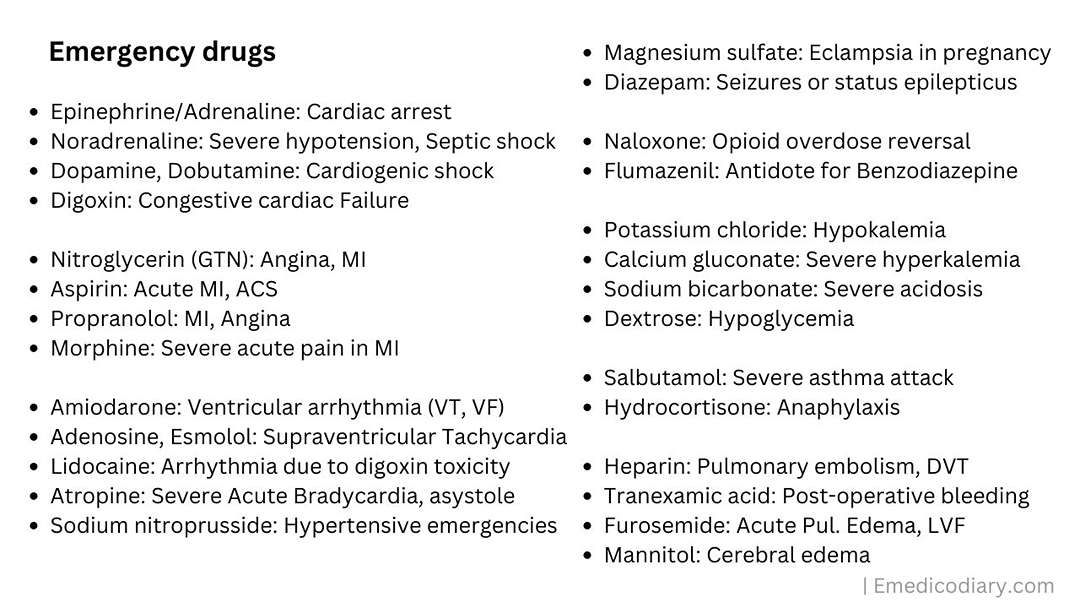
Summary Overview of Indication of emergency drugs
The one-line indication of emergency drugs is presented in the systemic form. The list of emergency drugs and their uses are
- Epinephrine/Adrenaline: Used in Cardiac arrest
- Noradrenaline: Used in Severe hypotension, Septic shock
- Dopamine, Dobutamine: Used in Cardiogenic shock
- Digoxin: Used in Congestive cardiac Failure
- Nitroglycerin (GTN): Used in Angina, MI
- Aspirin: Used in Acute MI, Acute Coronary Syndrome (ACS)
- Propranolol: Used in MI, Angina
- Morphine: Used in Severe acute pain in MI
- Amiodarone: Used in Ventricular arrhythmia (VT, VF)
- Adenosine, Esmolol: Used in Supraventricular Tachycardia
- Lidocaine: Used in Arrhythmia due to digoxin toxicity
- Atropine: Used in Severe Acute Bradycardia, asystole
- Sodium nitroprusside: Used in Hypertensive emergencies
- Magnesium sulfate: Used in Eclampsia in pregnancy
- Diazepam: Used in Seizures or status epilepticus
- Naloxone: Used for Opioid overdose reversal
- Flumazenil: Used as Antidote for Benzodiazepine
- Potassium chloride: Used in Hypokalemia
- Calcium gluconate: Used in Severe hyperkalemia
- Sodium bicarbonate: Used in Severe acidosis
- Dextrose: Used in Hypoglycemia
- Salbutamol: Used in Severe asthma attacks
- Hydrocortisone: Used during Anaphylaxis
- Heparin: Used for Pulmonary embolism, Deep Vein Thrombosis (DVT)
- Tranexamic acid: Used for Post-operative bleeding
- Furosemide: Used in Acute Pulmonary Edema, Acute Left Ventricular Failure (LVF)
- Mannitol: Used in Cerebral edema
For more detail about the classification of drugs, and to know under which category drugs belong, you can download the drugs book pdf. In this Pharmacological Drugs book pdf, most of the drugs have been covered.
A short overview and brief description of important commonly used emergency drugs are given below.
1. Epinephrine (Adrenaline): Adrenaline has a potent cardiac inotropic effect. It is used in cardiac arrest, severe allergies (anaphylaxis), and asthma unresponsive to salbutamol.
2. Norepinephrine (Noradrenaline): An important vasoconstrictor used to increase blood pressure in patients with severe hypotension or shock.
3. Dopamine: A vasopressor as well as a cardiac inotrope, used to support blood pressure and cardiac output in critically ill patients i.e. cardiogenic shock.
4. Dobutamine: A positive inotrope used to increase heart contractility and cardiac output in certain cases of heart failure or low cardiac output states i.e. cardiogenic shock.
5. Nitroglycerin (GTN): A vasodilator, used for the relief of angina (chest pain) like stable angina or unstable angina and in emergencies related to heart conditions. It venodilate & decreases cardiac workload reducing O2 demand. And increase O2 supply by coronary artery dilation.
6. Aspirin: An antiplatelet drug, used in emergencies involving chest pain or suspected heart attacks (acute myocardial infarction), as it can help reduce blood clot formation and prevent further blockage of coronary arteries.
7. Morphine: A potent analgesic used to relieve severe pain, such as in heart attacks (MI). It can also help reduce anxiety and stress.
8. Naloxone: An opioid antagonist used to rapidly reverse the effects of opioid overdose, helping to restore normal breathing and prevent death.
9. Atropine: An anti-muscarinic drug, used to treat severe acute bradycardia and work as an antidote for OPC poisoning.
10. Amiodarone: A Class III antiarrhythmic drug, potassium channel blocker, used to treat life-threatening cardiac arrhythmias by prolonging repolarization i.e. prolonged Phase 3.
11. Adenosine: Used in supraventricular tachycardia.
12. Lidocaine: A Class I antiarrhythmic, a sodium channel blocker, used for ventricular arrhythmias and as a local anesthesia during medical procedures.
13. Albuterol (Salbutamol): A bronchodilator used to treat acute asthma attacks and other breathing difficulties.
14. Hydrocortisone: Used for severe allergic reactions (anaphylaxis).
15. Oxygen: Administered when there are signs of respiratory distress or low oxygen levels in the blood.
16. Insulin: Used for tight glucose control in diabetic patients or those with hyperglycemia in the ICU.
17. Glucose: Administered to individuals experiencing hypoglycemia (low blood sugar) or altered mental status due to diabetes.
18. Sodium Bicarbonate: Given in emergencies to correct severe acidosis/metabolic imbalance or some drug overdoses i.e. antidote of TCA.
19. Diazepam or Lorazepam: Benzodiazepines are used for the treatment of seizures or status epilepticus & alcohol withdrawal. It can be given for sedation to calm the patient and reduce anxiety if it is contributing to the chest pain.
20. Magnesium Sulfate: Used for eclampsia and severe pre-eclampsia during pregnancy.
21. Oxytocin: Used to control postpartum hemorrhage.
22. Heparin or Low Molecular Weight Heparin (LMWH): Used as anticoagulation to prevent or treat deep vein thrombosis (DVT) and pulmonary embolism in immobilized or critically ill patients.
Emergency drugs list used for Cardiovascular condition
Emergency drugs are needed to save the life of patients from life-threatening conditions like acute myocardial infarction (Heart attack), cardiac arrest, severe cardiac arrhythmia, and other critical cardiovascular conditions, The list of most commonly used emergency drugs for cardiovascular conditions are
- Aspirin
- Nitroglycerin (GTN)
- Epinephrine (Adrenaline)
- Norepinephrine (Noradrenaline)
- Dopamine
- Dobutamine
- Amiodarone
- Adenosine
- Atropine
- Furosemide
- Heparin
- Streptokinase
- Esmolol
- Lidocaine
Emergency drugs list used for critical Respiratory conditions
Emergency drugs are used to treat acute, severe & life-threatening respiratory conditions like acute respiratory distress, severe asthma attacks, massive pulmonary embolism, etc. The list of emergency drugs used for critical respiratory conditions are
- Short-acting beta-agonists (SABAs) like albuterol or salbutamol.
- Anticholinergics like ipratropium bromide
- Corticosteroids (Dexamethasone, Hydrocortisone)
- Epinephrine (Adrenaline)
- Magnesium sulfate
- Naloxone
- Aminophylline
- Sodium bicarbonate
- Oxygen
Emergency drugs list for management of electrolytes imbalance
Sometimes, electrolyte imbalance can lead patients to emergency life-threatening conditions like hyperkalemia. Some of the commonly used emergency drugs for the management of electrolytes imbalance are
- Intravenous (IV) fluids
- Sodium bicarbonate
- Glucose & Insulin
- Calcium gluconate
- Magnesium sulfate
- Potassium chloride
- Furosemide
- Desmopressin
Emergency drugs list used as a vasodilator
In emergency conditions, like a hypertensive crisis, or heart failure where rapid dilation is needed for the improvement of blood flow, a rapidly acting vasodilator can be used. Some of the lists of emergency drugs commonly used as vasodilators are
- Nitroglycerin
- Nitroprusside
- Hydralazine
- Labetalol
Antidotes as emergency drugs
In an emergency department, an appropriate antidote should be administered to countereffects the effects of overdoses of drugs, and poisoning cases for saving the life of the patients. Here is the list of commonly used antidotes in emergency medicine.
- Naloxone: Antidote for opioid overdose
- Flumazenil: Antidote for benzodiazepine overdose
- Vitamin K: Antidote for warfarin
- Protamine sulfate: Antidote for heparin
- Atropine: Antidote for organophosphorus (OPC) poisoning
- Digoxin immune Fab: Antidote for digoxin toxicity
- Calcium gluconate: Antidote for severe hyperkalemia
- Sodium bicarbonate: Antidote for Tricyclic antidepressant (TCA) overdose
- Deferoxamine: Antidote for iron overload
- Dimercaprol (BAL): Antidote for heavy metal poisoning i.e. lead, arsenic, mercury, etc.
- N - acetylcysteine: Antidote for acetaminophen (paracetamol) poisoning
Emergency drugs list & uses in detail
1. Adrenaline/Epinephrine
Adrenaline is the non-selective α & β agonist adrenergic drug. It is a sympathomimetic drug also known as Epinephrine. Adrenaline is one of the most important essential emergency drugs.
Mechanism of action of Adrenaline
Adrenaline acts on all α & β receptors i.e. α1 is present in blood vessels, β1 present in the heat & β2 present in the lungs. But Adrenaline has a more affinity over the β1 receptor, so it has a potent inotropic effect.
Adrenaline is an alpha-adrenergic vasoconstrictor, that binds with alpha 1 receptor and can reduce bleeding & causes mydriasis.
Adrenaline is the drug of choice in cardiac arrest. It binds with the beta 1 receptor of the heart it stimulates the cardiac muscle to contract effectively.
Adrenaline is the drug of choice in anaphylactic reactions. It binds with the alpha 1 receptor and produces vasoconstriction to increase blood pressure. Similarly, adrenaline binds to the beta 2 receptor of the bronchus (lungs) and causes bronchodilation as histamine causes bronchoconstriction & vasodilation in anaphylactic conditions.
Indication of Adrenaline/Epinephrine
The indication of adrenaline are
- Cardiac arrest
- Anaphylaxis
- Superficial bleeding (Adrenaline shocked gauze)
- Asthma unresponsive to salbutamol (albuterol)
Dose of Adrenaline/Epinephrine
In cardiac arrest, the dose of adrenaline is 0.1 mg/ml IV (1:1000). The half-life of adrenaline is a very short duration i.e. 2 to 3 minutes, so adrenaline injection is given every 3 -5 minutes in case of cardiac arrest. In anaphylaxis, the dose of adrenaline is 0.3 to 0.5 mg/ml IM.
The available doses of Adrenaline are 0.1mg/mL (1mg/10mL or 1:10,000), 1mg/ml (1: 1000), 0.3 mg/ml auto-injector (EpiPen), 0.15 mg/ml (EpiPen Jr).
|
How to prepare the adrenaline dose of 0.1 mg/ml?
Adrenaline 1:1000 means 1gm per 1000ml or 1mg per 1ml (1mg in 1ml). Adrenaline 1:10000 means 1 gm per 10000ml or 1 mg per 10 ml (0.1 mg in 1 ml). |
Route of Administration of Adrenaline
The route of administration of adrenaline injection in emergency conditions is Intravenous (IV) in case of cardiac arrest and intramuscular (IM) in case of anaphylaxis.
Side effects of adrenaline
The side effects of adrenaline are hypertension & arrhythmia. Hypertension is due to alpha 1 receptor stimulation & arrhythmia is due to beta 1 receptor stimulation.
Thus, it is essential to monitor heart rate, blood pressure, pulse, and ECG at regular intervals during adrenaline therapy in the emergency ward. Hypertension due to adrenaline therapy can be controlled by phentolamine injection & arrhythmia by esmolol.
2. Noradrenaline
Noradrenaline is an adrenergic drug. It exerts both vasoconstrictor & inotropic effects, but noradrenaline is the potent vasoconstrictor (acts on alpha 1 receptor). Thus, help to increase blood pressure, heart rate & cardiac output.
Indication of noradrenaline
- Septic Shock (Vasodilatory shock)
- Acute hypotension
Dose of Noradrenaline
The dose of Noradrenaline is 0.01 - 0.3 mcg/kg/min IV infusion. The intramuscular route & subcutaneous route are contraindicated in Noradrenaline because of the high chance of necrosis.
3. Dopamine & Dobutamine
Dopamine & Dobutamine are two important emergency drugs of the catecholamine class. Dopamine acts on both alpha 1 & beta 1 receptors. And Dobutamine acts only on the beta-1 receptor.
On low doses, dopamine only stimulates the heart (β1) increasing cardiac output. In high doses, dopamine stimulates the heart (β1) as well as acts on blood vessels (α1) causing vasoconstriction & increase blood pressure too.
Dobutamine increases cardiac contractility and increases cardiac output increasing the heart rate.
Indication of Dopamine & Dobutamine
Dopamine & dobutamine are effective in Cardiogenic Shock & Acute Heart Failure. The indication of Dopamine & Dobutamine are
- Cardiogenic Shock
- Acute Heart Failure
Adrenaline & Nor adrenaline are not used in cardiogenic shock because it causes vasoconstriction & does not help in the improvement of vital organ perfusion.
Dose of Dopamine & Dobutamine
The dose of Dopamine & Dobutamine is 5 - 20 mcg/kg/min IV.
4. Atropine
Atropine is an anticholinergic i.e. antimuscarinic drug. Atropine is the drug of choice for severe acute bradycardia & antidote to OPC poisoning.
Mechanism of action of Atropine:
Atropine increases cardiac output & heart rate by blocking the vagal stimulation of the heart. Atropine blocks the muscarinic receptor & causes vasoconstrictors & increases blood pressure. It also has an anti-spasmodic effect.
Indication of atropine
- Severe acute bradycardia
- OPC poisoning
Dose of Atropine
The dose of atropine in severe acute bradycardia is 0.5 - 1 mg IV every 3 -5 min. The antidote dose of atropine in OPC poisoning is 1 - 6 mg IV.
5. Amiodarone
Amiodarone is a potassium channel blocker, belonging to class III antiarrhythmic drug. Amiodarone is a drug of choice in case of unstable ventricular tachycardia and ventricular fibrillation and is only anti-arrhythmic and considered to reduce sudden cardiac death.
Mechanism of action of Amiodarone
Amiodarone is an anti-arrhythmic drug that works on the cardiac cell membrane and blocks the potassium channel & prolonged the repolarization phase (Phase 3).
Indication of Amiodarone
- Unstable ventricular tachycardia
- Ventricular fibrillation
- Atrial fibrillation
Dose of Amiodarone
The dose of amiodarone in case of unstable ventricular tachycardia and ventricular fibrillation is 300mg IV followed by 150mg IV.
6. Adenosine
Adenosine is considered a Class V anti-arrhythmic drug. It decreases the rate of conduction of cardiac impulses blocking the AV node. Adenosine is the drug of choice for Paroxysmal supraventricular tachycardia (PVST). Abnormality of rate & rhythm arising from the atrium i.e. above the ventricle is called supraventricular tachycardia (SVT). Supraventricular tachycardia includes Atrial Fibrillation, Atrial flutter, Paroxysmal supraventricular tachycardia (PSVT), Wolff Parkinson White syndrome, etc.
Mechanism of action of Adenosine
Adenosine is an anti-arrhythmic drug that slows down the conduction time of cardiac impulses through the AV node. It can interrupt the reentry pathways through the AV node & can restore normal sinus rhythm in patients with Paroxysmal supraventricular tachycardia (PSVT).
Dose of Adenosine
The dose of adenosine is 6 mg IV. The half-life of adenosine is very short i.e. less than 10 seconds. So, it must be administered rapid IV push otherwise it does not work. The maximum dose of 12 mg can be administered if a 6 mg rapid IV push does not work.
7. Lidocaine
Lidocaine, also known as Lignocaine, is a local anesthetic drug. But it also works as a class I anti-arrhythmic drug by blocking sodium channels in the cardiac cell membrane.
Indication of Lidocaine
- Ventricular tachycardia due to digitalis toxicity (Digoxin Toxicity)
- Ventricular arrhythmia
- Acute MI
- Cardiac catheterization
In ventricular tachycardia and ventricular fibrillation, Lidocaine can be used if amiodarone is not available at the moment or is contraindicated.
Dose of Lidocaine
The dose of Lidocaine is 25 - 50 mg/min.
8. Nitroglycerin/ Glyceryl Trinitrate (GTN)
Nitroglycerin, also known as Glyceryl Trinitrate (GTN), is an anti-anginal drug, a vasodilator. Nitroglycerine (GTN) is short-acting organic nitrate and has a rapid onset of action.
Mechanism of action of Nitroglycerine (GTN)
Nitroglycerine is a vasodilatory drug primarily used to treat anginal pain. Angina is a cardiovascular disease characterized by severe strangling chest pain due to an imbalance between O2 supply & O2 demand.
It causes relaxation of smooth muscles i.e. vasodilation & coronary artery dilation. Through vasodilation, it decreases the venous return & decreases the cardiac workload reducing the myocardial O2 demand. Similarly, it increases the myocardial O2 supply through coronary vasodilation.
Indication of Nitroglycerine (GTN)
- Unstable Anginal pectoris
- Coronary artery spasm
- Myocardial infarction
- Per operative hypertension
Dose of Nitroglycerine (GTN)
The dose of Nitroglycerine (GTN) is 0.5 - 2 mg/min. In emergency conditions, it is given sublingually, and its action is onset within 2 - 3 min.
9. Furosemide
Furosemide is a powerful loop diuretic that blocks the Na-K-2Cl symporter in the thick ascending limb of the loop of Henle. It prevents the reabsorption of sodium, potassium, and chloride & causes forceful diuresis.
Indication of Furosemide
It is used in emergency conditions like
- Acute Left ventricular failure
- Acute Pulmonary edema
- Edema due to Nephrotic syndrome, CCF
- Cerebral edema
- Severe hypertension
- Hyperkalemia
Dose of Furosemide
The initial dose of furosemide is 20 - 80 mg IV. The maximum dose that can be given is 600 - 800 mg. The onset of action of furosemide is within 10 - 15 minutes.
10. Calcium gluconate
Calcium gluconate is the calcium salt of gluconic acid used as an emergency drug in conditions like dysrhythmia and cardiotoxicity due to hyperkalemia or hypermagnesemia. It is also used in the prevention & treatment of severe hypocalcemia causing tetany, laryngospasm & seizure. For magnesium sulfate toxicity, calcium gluconate is the antidote.
Indication of Calcium gluconate
- Dysrhythmia and cardiotoxicity due to hyperkalemia or hypermagnesemia
- Prevention & treatments of hypocalcemia, tetany.
- Magnesium sulfate toxicity
Mechanism of action of Calcium gluconate
Calcium is needed for the maintenance of proper functioning of the nervous, muscular including cardiac and skeletal systems. It is important for nerve impulse conduction, muscle contraction, blood coagulation, and cell membrane permeability.
In the case of Hyperkalemia & Hypermagnesemia, calcium gluconate binds with the excess potassium & magnesium ions.
Dose of calcium gluconate
The dose of calcium gluconate is 1 - 3 gm IV push over 3 - 5 min. The available dose of calcium gluconate is 1000 mg per 10 ml i.e. 100 mg/ml.
11. Magnesium sulfate
Magnesium sulfate is an anti-convulsant drug used in the management of life-threatening seizures/convulsions. This drug should be available in every emergency department, especially in Obstetric wards. It is used in the management of eclampsia in pregnancy, a triad of hypertension, proteinuria & seizure/convulsion.
Magnesium sulfate is a drug of choice in the case of Torsade de points, a type of ventricular arrhythmia. In Torsade de Pointes, there is a prolonged QT interval which may be due to hypokalemia or hypomagnesemia.
Mechanism of action of Magnesium sulfate:
Magnesium sulfate reduces acetylcholine release at the neuromuscular junction & blocks the peripheral nerve impulse conduction. It acts as a membrane stabilizer and neuroprotector. It also inhibits calcium influx & decreases muscle contraction. It also blocks the calcium channel & helps to increase potassium and magnesium levels.
Indications of Magnesium sulfate:
- Life-threatening seizures /convulsions
- Pre-eclampsia and eclampsia during pregnancy.
- Severe acute asthma attack
Dose of Magnesium sulfate
The dose of Magnesium sulfate in Eclampsia is 4 - 6 gm over 15 - 20 minutes followed by 10 gm IM (4 gm loading dose with 10 g IM). The dose of Magnesium sulfate in severe acute asthma is 2 gm IV over 15 - 30 minutes. In the case of Torsade de points, its dose is 1 - 2 gm IV slow push.
12. Dexamethasone
Dexamethasone is a corticosteroid, anti-inflammatory immunosuppressant drug. It decreases inflammation by suppression of polymorphonuclear leukocytes.
Indication of Dexamethasone
- Any inflammation
- Allergies, Anaphylaxis
- Cerebral edema
- Septic shock
Dose of Dexamethasone
The initial dose of dexamethasone is 0.5 - 20 mg.
Steroids are increasingly popular among sportsmen and fitness enthusiasts who want to achieve their physical goals and improve their performance due to online platforms, changing accessibility despite traditional legal challenges and limited availability. Steroids Canada provides a diverse selection of premium pharmaceutical brands, dosages, and forms of steroids to cater to individual preferences and demand.
Conclusion
Emergency drugs should be only used for highly qualified, trained healthcare professionals who are knowledgeable & skill in their proper administration & monitoring. Incorrect dosing or administration of Emergency drugs can deteriorate the patient's condition leading to serious consequences, including adverse side effects, complications, or even life-threatening situations. If you are facing a medical emergency or require information about specific drug doses, please contact a medical professional, visit the nearest healthcare facility, or call emergency services immediately.
It is important to recognize that the administration of emergency drugs should only be performed by qualified and trained medical professionals to ensure the correct dosage, appropriate indications, and the best possible patient outcomes. These medications are powerful tools that, when used judiciously and skillfully, can save lives and improve the chances of recovery in critical situations.

Comments (0)