Partograph
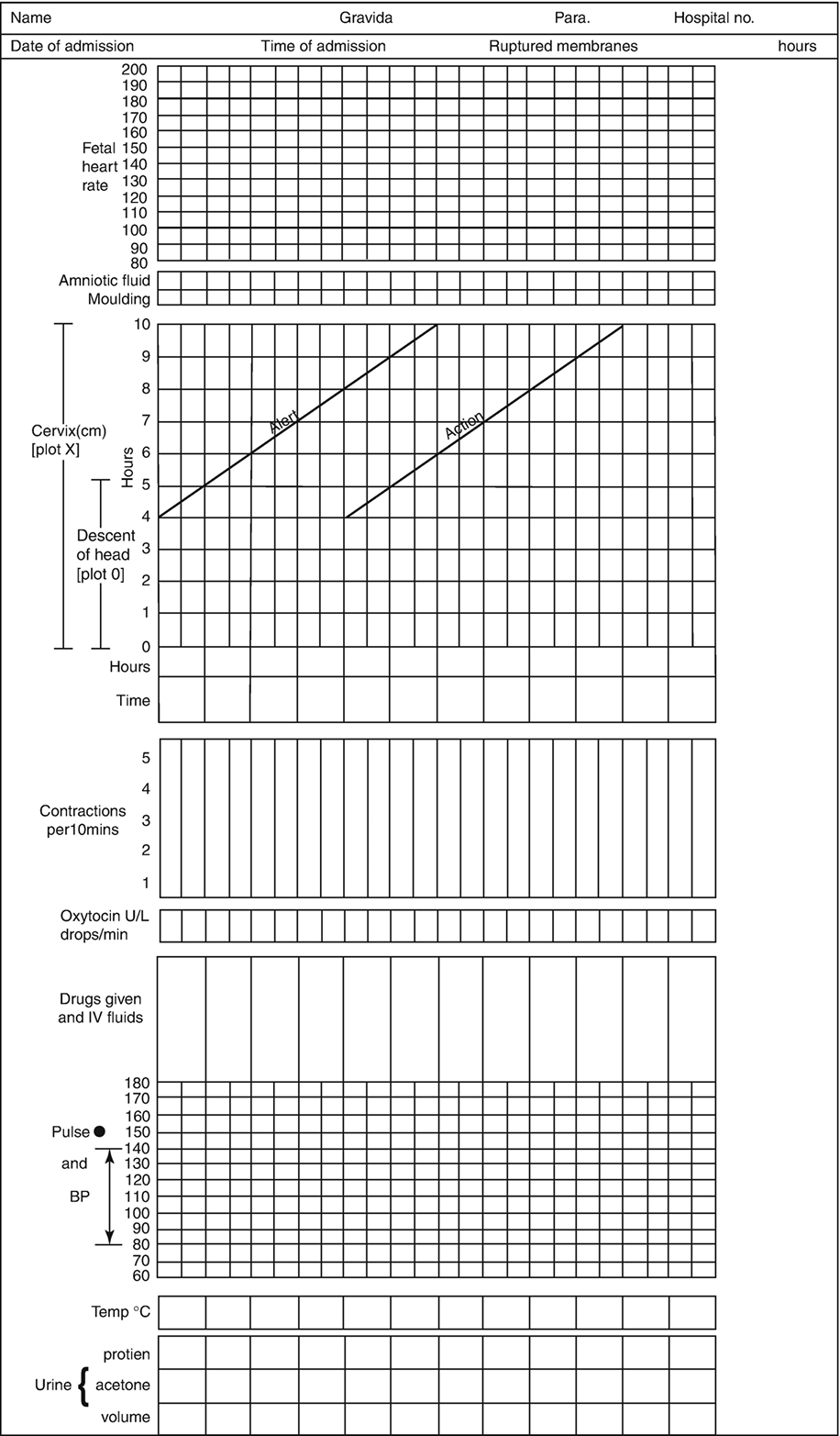
The partograph is the graphic representation of the events of labor plotted against time on a single sheet of paper. In other words, a partograph can be defined as a graphical tool used in obstetrics to monitor the progress of labor and maternal & baby well-being.
History of Partograph
In 1954, Friedman introduced the graphical labor curve on the basis of his observation of the progress of labor i.e. cervical dilation & fetal station against time in hours from the onset of labor. Further in 1972 Philpott and Castle modified the Labor curve version of Friedman. The concept of Alter line & Action line has been introduced.
In 1987 WHO introduced its own Partograph as an adaption of the Philpoot & Castle Partograph which includes the Latent phase of 8 hours & active phase which started from a 3 cm dilation of the cervix. Later in 2000, the WHO introduced the 2nd version of the Partograph to make it easier & simpler, Latent phase of cervical dilation has been excluded and the Active phase started from 4 cm of cervical dilation which is known as the Modified WHO Partograph.
In February 2018, WHO published a set of recommendations on 'Intrapartum care for a positive childbirth experience' which includes the new duration of the 1st and 2nd stages of labor and provides guidance on the timing and use of labor interventions to improve the mother & the baby's well-being. Based on these recommendations, the new Next Generation Partograph has been introduced as the WHO Labour Care Guide.
Here, we will discuss the basic concept of the Partograph based on the modified WHO Partograph.
Components of Partograph
There are 4 basic components/elements of a Partograph. They are:
- Patient Information
- Record of the progress of labor
- Fetal record
- Maternal record
Patient Information Part
In Patient information, Partograph consists of
- Name
- Garvida
- Para
- Rupture membrane
- Date of admission
- Time of admission
- Hospital number
Record of the progress of labor
The progress of labor is noted by
- Cervical dilation
- Descent of fetal head
- Uterine contractions
Fetal record
The fetal part of the Partograph consists of:
- Fetal heart rate
- Amniotic fluid
- Molding
Maternal record
The maternal part of the Partograph contains
- Pulse
- Blood pressure
- Temperature
- Urine volume, protein & acetone level
- Drugs given & I/V fluids
- Oxytocin given U/L (drops/min)
Importance/ Advantages of Partograph
1. A single sheet of Partograph provides all necessary information about the progress of labor, and maternal & fetal well-being.
2. Partograph helps in the early detection of abnormal progress of labor so that appropriate steps could be taken in time.
3. Partograph helps in the prevention of prolonged labor, obstructed labor & cesarean section rate. There is improvement in maternal morbidity, perinatal morbidity & mortality.
4. Early detection of cephalopelvic disproportion is possible through a Partograph study.
5. One can detect the timing of augmentation & termination of labor if needed, through the study of graph plots on Partograph.
Fetal heart rate (FHR):
The fetal heart is recorded every half hour for 1 minute. It is indicated by a dot in partograph and later all dots are joined. Normal Fetal Heart Rate range is from 110 - 160 beats/min. If below 110 beats/min, it is bradycardia. If above 160 beats/min, it is tachycardia
Amniotic fluid:
Membrane status is checked at every vaginal examination which is done every 4 hours. If the membrane is ruptured the color of amniotic fluid is recorded. According to the status of the membrane & amniotic fluid, the following alphabets (I, A, B, C, M) are written on the box of the partograph.
- I for membrane intact
- A for absent amniotic fluid
- B for Blood-stained fluid
- C for clear fluid
- M for meconium-stained fluid
Molding:
Molding is recorded in vaginal examination which is done every 4 hours. Sutures & bones are felt on the fetal head and based on that (0, +, ++, +++) are written on the partograph box.
When separated bones & sutures are felt easily, we write '0'. When bones are just touching each other i.e. Suture opposed, then we write 1 Plus (+). When bones are overlapping i.e. Suture overlapped but reducible, then we write 2 Plus (++). When bones are overlapping i.e. Suture overlapped and not reducible, then we write 3 Plus (+++).
Molding is an important parameter, which shows how adequately the pelvis can accommodate the fetal head. Increasing molding with slow descent of the fetal head indicates cephalopelvic disproportion.
Descent of fetal head:
Descent of the fetal head is assessed & measured by abdominal examination using the rule of fifth to assess the engagement of the fetal head. It refers to the part of the fetal head palpable above the pubis symphysis which is recorded as a circle (O) in partograph before doing every vaginal examination i.e. 4 hourly. Rule of fifth refers to the portion of the fetal head palpable above the symphysis pubis in finger breath which is assessed by placing the hand above the symphysis pubis (5-finger breadth of the hand above symphysis pubis).
- The head is 5/5 palpable above the pubis symphysis means the head is mobile, not engaged. It means the head accommodates the full width of five fingers above the symphysis pubic.
- The head is 2/5 above the symphysis pubis means the head accommodates two fingers width above the symphysis pubis. When the head is 2/5 palpable or less above the symphysis pubis by abdominal examination, that means the fetal head is engaged.
The fetal head, which is mobile above the symphysis pubis, will accommodate the full width of the 5 fingers of the hand. As the fetal head descends downward, the portion of the head remaining above the symphysis pubis will be represented by fewer fingers (4/5th, 3/5th etc). It is said that the head is engaged when 2 finger width or less represents the proportion of the fetal head above the symphysis pubis.
For labor to progress well, dilatation of the cervix should be accompanied by descent of the head. However, descent may not take place until the cervix has reached about 7 cm dilatation.
Cervical dilatation:
Cervical dilation is assessed by two fingers at every vaginal examination i.e. every 4 hours. On average, 1 finger is equal to 1.6 cm & 2 fingers are equal to 3 cm.
Cervical dilation is marked with a cross (X) & 1st plotting of cervical dilation is always marked along the alert line of the partograph.
There are two phases of cervical dilation in the progress of labor.
1. Latent phase: Latent phase of cervical dilation is up to 4 cm of cervical dilation from the onset of true labor pain. It is the slow period of cervical dilatation. Usually latent phase lasts for 8 hours. If longer than 8 hours, it needs reassessment. The patient should be transferred to the hospital if she is in a peripheral center. Nowadays latent phase is not included in the partograph.
2. Active phase: Active phase of cervical dilation starts from 4 cm to 10 cm. In the active phase (faster period of cervical dilatation) the cervix dilates at a rate of 1 cm/hour in primigravida & 1.5 cm/hour in multigravida. And fetal head starts to descend from 7 cm dilation.
According to the modified WHO Partograph (2000), the active phase of cervical dilation starts from 4 cm to 10 cm. From the active phase only, Partograph graph plotting is started. The latent phase of cervical dilation is not needed to be plotted & not included in the partograph.
But according to the WHO Labour Care Guide, the active phase of cervical dilation starts from 5 cm to 10 cm. So, from 5 cm of cervical dilation only, graph plotting on the WHO Labour Care Guide Partograph started.
Alert line:
In the modified WHO partograph (2000), the Alert line starts from 4 cm of cervical dilatation to the point of expected full dilatation at the rate of 1 cm per hour. Always start 1st plotting of cervical dilation along the alert line.
Action line:
The action line is present 4 hours to the right of the alert line & parallel to the alert line.
|
Always remember plotting should be started from cervical dilation on the Alert line, then only other parameters are plotted.
Plotting on the Partograph always should be started 1st from cervical dilation when it is 4 cm dilated, which should be always drawn along the alert line.
|
If cervical dilation has not progressed to 4 cm, then any plotting of the Partograph is not done.
When the patient presented with cervical dilation of more than 4 cm, for example, 5 cm, then plotting should be started with 5 cm on the alert line.
If the patient presented with 6 cm, then plotting should be started from 6 cm on the alert line.
If the graph plot of cervical dilation, lies along the alert line or left of the alert line of the partograph, it indicates that there is satisfactory cervical dilation. In normal cases with normal cervical dilatation plotting of cervical dilatation will be on the alert line or to the left of the alert line.
If cervical dilatation crosses the alert line and lies between the alert line & action line zone, it indicates slow dilatation of the cervix and therefore delay in labor. So reassessment is indicated. Reassessment should be done about 3 main things.
- Passenger (Fetus)
- Passage Canal
- Power of uterine contraction
The action line is drawn 4 hours to the right of the alert line. If the cervical dilatation graph plot crosses the action line, then it indicates a delay in the progress of labor. So critical assessment of the cause of the delay is needed. The appropriate decision should be taken regarding appropriate management to overcome this delay of labor progress. There are 2 options regarding the management of this delay of labor progress.
- Termination of labor
- Augmentation of labor
Uterine contraction
There must be good uterine contractions in order for labor to progress well. In normal labor, they usually become more frequent and longer. Observations of Uterine contractions are made hourly in the latent phase and half-hourly in the active phase for 10 minutes. Two observations were made on uterine contractions, the frequency, and the duration.
The frequency of contractions is the number of contractions, which occur in a 10 minutes period. The length of the contractions is counted from the time the contraction is first felt abdominally to the time when the contraction passes off & is measured in seconds.
On Partograph there are 5 blank squares & each square represents one contraction. Regarding the uterine contraction frequency on the partograph, if two contractions are felt in 10 minutes, two squares will be shaded. The length of the contraction is counted in seconds and there are three possible ways to fill the squares according to how long the contractions last.
- If the contraction last for less than 20 seconds (Mild contraction), squares are filled with dot-dot.
- If the contraction last for 20 to 40 seconds (Moderate contraction), squares are filled with inclined parallel lines.
- If the contraction lasts more than 40 seconds (Severe contraction), squares are shaded black.
Contraction of more than 3 & less than 5 in number in 10 minutes in which each contraction lasts for more than 40 seconds & less than 1 minute is considered to be good uterine contraction.
At a glance
How frequently components of the partograph are recorded?
| Components of Partograph | Time interval |
| Fetal heart rate | 30 min |
| Uterine contraction | 30 min |
| Pulse | 30 min |
| Blood pressure | 2 hourly |
| Temperature | 2 hourly |
| Cervical dilation | 4 hourly |
| Descent of fetal head | 4 hourly |
| Urine volume, Protein, and Acetone | 4 hourly |
Vaginal examination is done every 4 hours. In the case of Induction or augmentation of labor, it is done 2 hourly. In the case of multigravida, it can be done more frequently i.e. less than 4 hours interval. In the latent phase of labor, Fetal Heart Rate & Uterine contraction are measured at hourly intervals.
What action you will take if the action line is crossed & fetal head is 5/5?
Action is to be taken when the action line is crossed & fetal head is 5/5. The fetal head 5/5 means the head is floating above the brim and not engaged. Usually, the head becomes engaged in normal labor but in this case, cervical dilatation crosses the action line, and the head is not engaged which indicates a delay in the progress of labor. In this condition:
1. A critical assessment of the cause of the delay is needed.
2. Termination can be done either by augmentation of labor or cesarean section if indicated. Augmentation of labor is done by ARM and/or oxytocin. If liquor is meconium stained, a cesarean section should be done.

Comments (0)