HPI Medical Abbreviation
HPI medical abbreviation is History of Present Illness, which is a detailed form of chief complaints describing the development & progress of the patient’s present illness. History of present illness (HPI) is the elaborated form of chief complaints describing a patient's present illness from initial signs or symptoms to present in chronological order.
History of present illness (HPI) is also sometimes called History of Presenting symptoms (HPS).
Key Components of History Taking
- Chief complaint (CC)
- History of present illness (HPI)
- Review of systems (ROS)
- Past, family, and/or social history (PFSH)
Types of History of Present Illness (HPI)
- Brief HPI
- Extended HPI
A Brief HPI contains about 1 to 3 components of HPI. For example, dull pain over the right arm for 10 days. Here, character, Location & Duration components of HPI have been covered.
An extended HPI contains 4 or more components of the HPI describing the patient's symptoms. For example, dull pain over the right arm for 10 days which relieves by taking ibuprofen & aggravated by even lifting light objects. The patient stated that the pain start after falling on the floor. Here, character, Location & Duration, modifying factors, and timing components of HPI have been covered.
Components of History of Present Illness (HPI)
There are basically 8 components of the History of the present illness according to which one can describe the principal symptoms of patients. They are:
- Location
- Quality
- Severity
- Duration
- Timing
- Context
- Modifying factors &
- Associated signs and symptoms.
Location:
Location denotes the location of the pain. For example, Central chest pain, Peripheral chest pain, Pain in the upper quadrant of the abdomen, Lower abdominal pain, cut injury in the right hand, pigmentation over the neck, etc.
Quality:
Quality describes the quality or characteristics of symptoms like quality of pain can be described as sharp pain, dull pain, burning pain, colicky pain, throbbing pain, stabbing pain, squeezing pain, etc.
Severity:
Severity indicates the degree of pain like asking the patients to describe their pain on a scale of 1 - 10.
Duration:
How long have you had your symptoms? Duration describes in terms of days, weeks, months, or years.
Timing:
It denotes the time-related elements. Describes when you have symptoms or the frequency of symptoms. For example Cough in the early morning, High-grade fever at night, Chest pain 3 times in a week, Pain starts after eating food, etc. Is the pain constant or intermittent?
Context:
What is the patient doing when the symptoms start?
Modifying Factors:
What makes the patient’s symptoms better or worse? For example, taking rest or medicine relieves the pain, Pain increase on exertion, etc.
Associated Signs and Symptoms:
Doctors make ask about other related symptoms based on clinical assessments like do you experience pain while exercising.
History of Present Illness (HPI) Examples
To clarify the elements/ components of the History of Present Illness (HPI), an example has been set below.
Location: Pain in the groin
Quality: Burning pain in the groin
Severity: Mild burning pain in the groin that has become more intense
Duration: Mild burning pain in the groin that has become more intense & frequent for the last 7 days
Timing: History of intermittent mild burning pain in the groin that has become more intense & frequent for the last 7 days.
Context: History of intermittent mild burning pain in the groin that has become more intense & frequent for the last 7 days since the patient had worked on the farm and continues to feel intense pain when bending.
Modifying factors: History of intermittent mild burning pain in the groin that has become more intense & frequent for the last 7 days since the patient had worked on the farm and continues to feel intense pain when bending. The patient is currently taking Mortin 500 mg for 3 days which relieves his symptoms to some extent.
Associated signs & symptoms:
History of intermittent mild burning pain in the groin that has become more intense & frequent for the last 7 days since the patient had worked on the farm and continues to feel intense pain when bending. The patient is currently taking Mortin 500 mg for 3 days which relieves his symptoms to some extent and he also complains about nausea for 3 days.
History of Present Illness (HPI) Example in case of COPD
According to the patient’s statement, he was reasonably well 2 years back. Since then, he has been suffering from frequent attacks of cough with productive sputum. Cough is present throughout the day & night, more marked in the morning and also on exposure to cold and dust. It is progressively increasing day by day. The sputum is whitish, mucoid, non-foul smelling & not blood-stained.
For the last 1 year, he also complained of gradual development of difficulty in breathing, more marked during moderate to severe exertion, relieved by taking rest. His breathlessness is also progressively increasing & more marked for the last 7 days.
There is no history of chest pain, hemoptysis, fever, swelling of the ankle, or weight loss. His bladder & bowel habits are normal.
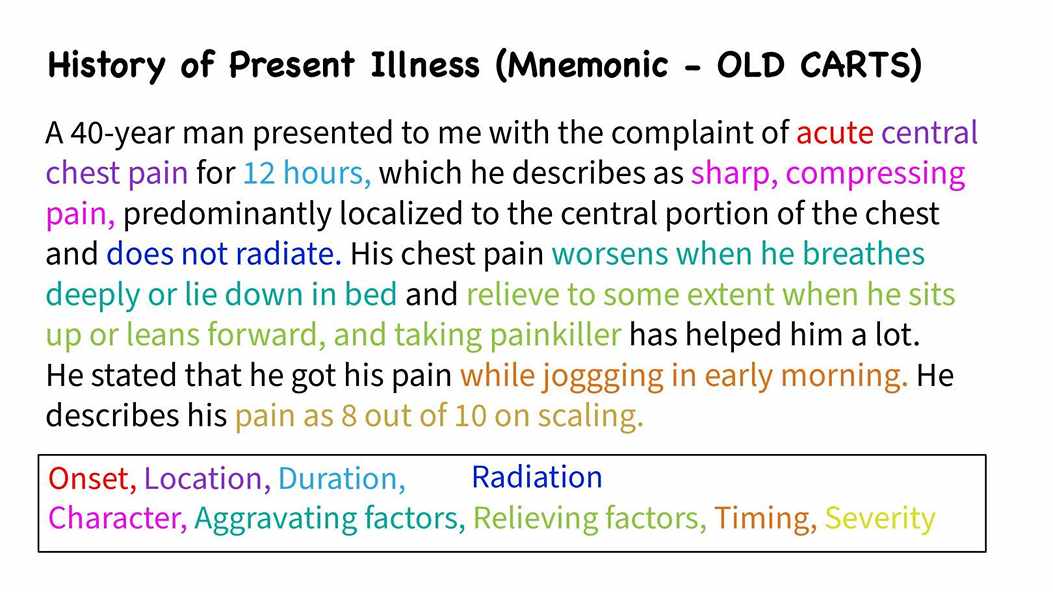
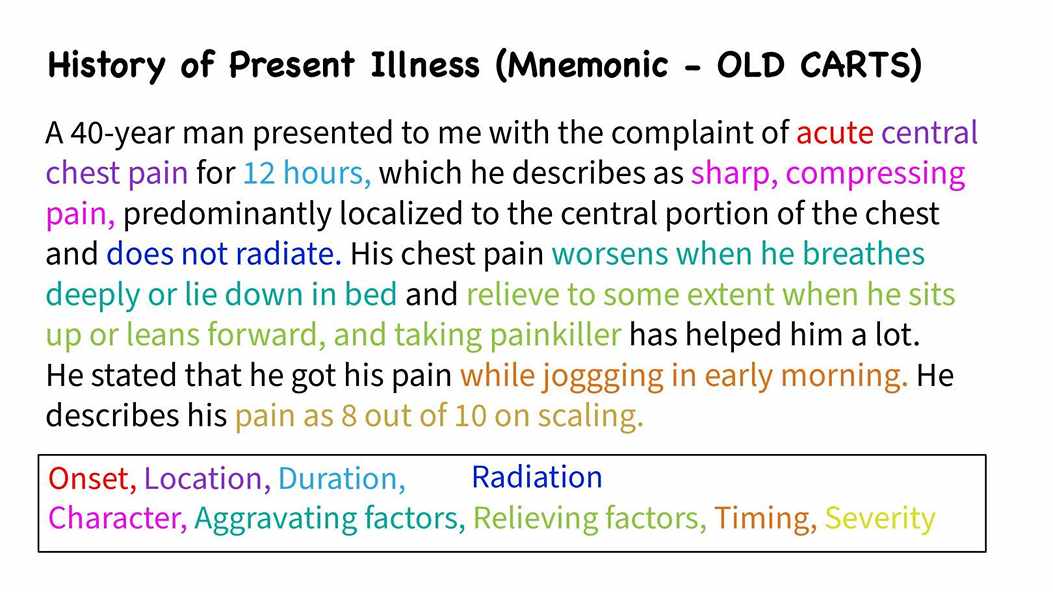
History of Present Ilnesss (HPI) Example for pain assessment (OLD CARTS Example)
A 40-year man presented to me with the complaint of acute central chest pain for 12 hours, which he describes as sharp, compressing pain, predominantly localized to the central portion of the chest and does not radiate. His chest pain worsens when he breathes deeply or lie down in bed and relieve to some extent when he sits up or leans forward, and taking painkiller has helped him a lot. He mentioned that the pain 1st initially started while jogging in the early morning. He describes his pain as 8 out of 10 on scaling.
This History of present illness (HPI) has been described in terms of OLD CARTS. Onset, Location, Duration, Character, Aggravating factor, Relieving factors, Timing, Severity
OLD CARTS Mnemonic
OLD CARTS can be used as mnemonics for history taking for describing the symptoms in the History of Present Illness (HPI). OLD CARTS stands for:
- O - Onset
- L - Location
- D - Duration
- C - Character
- A - Aggravating factors
- R - Relieving factors
- T - Timing
- S - Severity
OLD CARTS includes all the basic components of the History of Present Illness (HPI).
O in OLD CARTS indicates the onset of symptoms that is for days, weeks, months, or years. It can also describe in terms of acute or gradual or chronic onset. It corresponds to the Duration of HPI.
L in OLD CARTS indicates location, especially used to denote the location of pain i.e. central or peripheral chest pain, lower abdominal pain, weakness of the right leg, etc. It corresponds to the Location components of HPI.
D in OLD CARTS indicates the duration of symptoms like how often or how long the symptoms persist. For example pain last for a few minutes, hours, or days.
C in OLD CARTS indicates characteristics of symptoms. For example, the characteristics of pain can be described as sharp, dull, burning, colicky, throbbing, squeezing, and compressing pain.
A in OLD CARTS indicates Aggravating factors. Does the symptom worsen by activity or factors? Pain worsens on walking upstairs, eating food, etc. It corresponds to modifying factors of HPI.
R in OLD CARTS indicates radiation of pain & Relieving factors. For example, pain relieves by taking rest or medicine, throat irritation subsides after taking hot water, etc. It corresponds to modifying factors of HPI.
T in OLD CARTS indicates the timing. Describes when you have symptoms or the frequency of symptoms. For example Cough in the early morning, High-grade fever at night, Chest pain 3 times in a week, Pain starts after eating food, etc. Is the pain constant or intermittent?
S in OLD CATES indicates Severity i.e. the degree of pain like asking the patients to describe their pain on a scale of 1 - 10.
By describing the symptoms in terms of OLD CATES, one can write a better history of present illness (HPI).
Difference between Onset, Duration & Timing in OLD CARTS while describing History of Present Illness (HPI)
Acute Chest pain for 3 days, which lasts for 5 - 10 minutes on exertion. Here, Acute denotes onset & 3 days denote the duration of chest pain and 5 - 10 min denotes timing/frequency.
Another example:
Acute Cough for 1 week, more in the early morning. Here 1 week denotes duration and early morning indicates timing.
Socrates pain assessment
For the assessment of pain, while describing the pain in the History of Present Illness (HPI), we can use SOCRATES mnemonics which almost cover all basic components of the History of Present Illness (HPI).
SOCRATES stands for Site, Onset, Character, Radiation, Association, Time, Exacerbating/Relieving factors, and Severity.
Site: Where is the pain?
Onset: When did the pain start? Was it sudden or gradual?
Character: What is the pain like? Is it like stabbing, compressing, sharp, dull, ache, throbbing, squeezing pain?
Radiation: Does the pain radiate anywhere else in the body?
Association: Are any other signs or symptoms associated with pain?
Time: (Duration, Course, Pattern): How long the pain has been there? Does the pain follow any pattern?
Exacerbating/Relieving factors: Does anything change the pain?
Severity: How bad is the pain? Can you scale in 1 - 10?
Objective of History of Present Illness (HPI)
- Provide a detailed overview of the development & progress of the patient’s symptoms in chronological order.
- Helps to determine which system should be examined or focused on in the Review of systems (ROS) & physical examination.

Comments (0)