Clinical Indicators Prompting Secondary Surgical Intervention in Spinal Care
A patient walks into your clinic months after spinal surgery; still hurting, still limited, still searching for answers. Not every post-op ache is routine.
Ongoing pain, lingering numbness, or new neurological symptoms aren’t just inconvenient; they’re red flags. Understanding when these signs point to deeper structural problems can change outcomes.
It’s time to dig into the clinical indicators that reveal when a second surgery isn’t optional; it’s essential.
Persistent or Recurrent Pain: A Signal Worth Investigating
Pain that lingers (or reemerges) long after the expected healing window is often the first and loudest clinical alarm. While discomfort is common in the immediate post-op phase, pain that stretches beyond 12 weeks, intensifies with movement, or spreads to new areas often signals deeper structural or neurological issues.
Patients may report:
- Unrelenting nerve pain not responsive to medications or physical therapy
- Pain patterns that were not present before surgery
- A sudden return of radiculopathy or spinal claudication
- Mechanical back pain that worsens with specific postures or activity levels
In these scenarios, pain is not just a symptom but a guidepost toward reassessment.
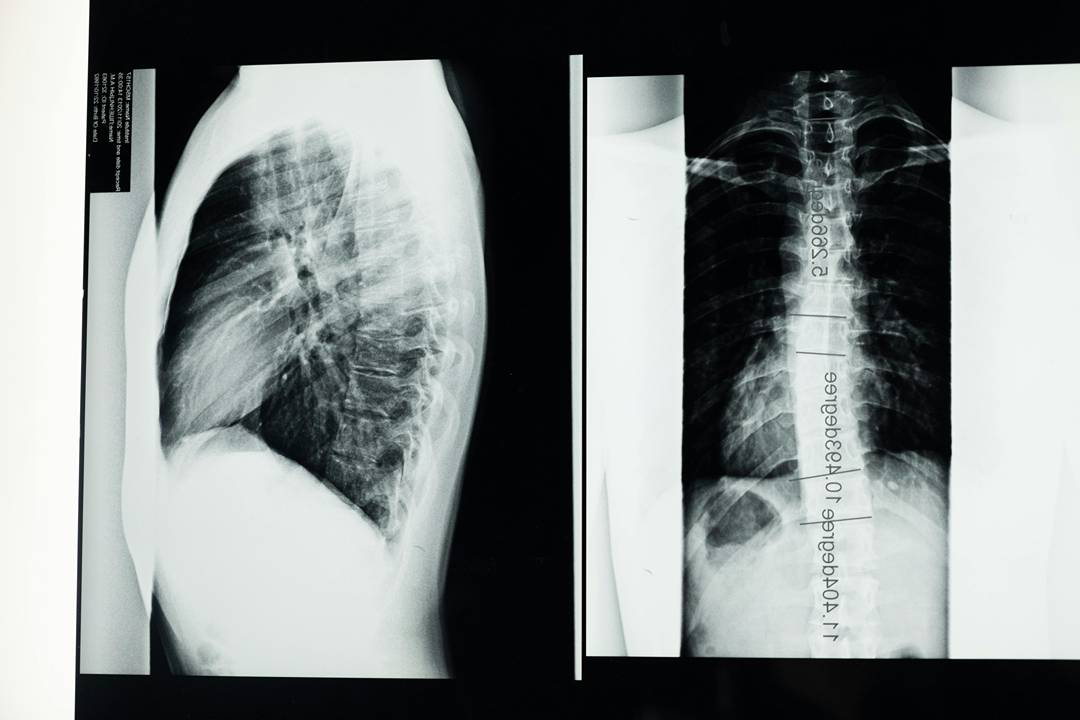
Mechanical Instability or Hardware Complications
Even when surgical techniques are sound, the spine is a dynamic structure. Over time, implants may loosen, hardware may shift, or fusion segments may fail to consolidate. Mechanical instability can manifest subtly at first, through minor functional deficits or sensations of “giving way.” Left unchecked, it progresses to clear imaging findings and significant clinical consequences.
Secondary imaging often reveals:
- Hardware loosening or breakage
- Pseudarthrosis or failed fusion
- Adjacent segment degeneration at accelerated rates
- Implant migration with potential neural impingement
In such cases, revision spine surgery becomes necessary to reestablish mechanical integrity and preserve neurological function.
Progressive Neurological Decline
Loss of motor strength, worsening gait, new-onset numbness, or signs of myelopathy aren’t symptoms that should ever be delayed. They often indicate compression or compromised blood flow to critical neural structures. These may result from postoperative scarring, recurrent disc herniation, or misalignment that was either missed initially or developed post-surgery.
Surgical reevaluation is often triggered when patients experience:
- Diminished hand coordination or foot drop
- Incontinence or saddle anesthesia
- Spinal cord signal changes on MRI
- Positive findings during electromyography or nerve conduction studies
Infections and Inflammatory Complications
Although rare, postoperative infections present a direct threat to spinal stability and systemic health. Whether superficial or deep, they can compromise fusion, erode hardware, or trigger widespread inflammatory responses. Revision surgery becomes essential if debridement or long-term antibiotics fail, or if infection infiltrates the bone or dura.
Clinical indicators include:
- Persistent wound drainage or erythema
- Elevated inflammatory markers despite antibiotics
- Imaging showing abscess formation or osteomyelitis
- New onset of fever and systemic symptoms
Failure of Prior Surgical Goals
Sometimes, the initial surgery may technically succeed, but the patient’s functionality doesn’t reflect it. Pain remains debilitating, posture is compromised, or the original spinal alignment was not fully restored. Here, the concern is not always a discrete failure but a misalignment between surgical outcome and patient goals.
Indicators for revision in these gray areas include:
- Incomplete decompression confirmed by imaging
- Under-corrected spinal curvature or sagittal imbalance
- Persistent disability despite completed physical rehabilitation
- Inability to return to baseline function in daily activities
Why Revision Surgery Isn’t Just a “Do-Over”
Second-line surgical intervention isn’t a matter of retracing steps; it’s a reengineering of strategy. These are often more complex cases involving altered anatomy, increased scar tissue, and higher stakes. Patients benefit most from spine surgeons who specialize in difficult cases and have access to advanced imaging, intraoperative navigation, and multidisciplinary rehabilitation teams.
Bridging the Gap Between Surgery and Stability
Each surgical decision is a pivot point. In spinal care, where anatomy meets mobility, that pivot often requires revisiting the surgical plan when outcomes stall or decline. Whether the issue is hardware fatigue, scar-induced compression, or progressing degeneration, timely secondary intervention can realign a patient’s trajectory toward meaningful recovery.
Clinicians who can translate imaging and symptoms into precise surgical strategies offer patients more than just pain relief. They offer renewed possibility. And that’s the measure of success that really matters.

Comments (0)