The Role of Single Cell Omics in Infectious Disease Research and Management
Advances in molecular biology have transformed our capacity to understand infectious diseases at unprecedented resolution. Traditional bulk analyses, which average signals across thousands or millions of cells, can obscure critical differences in how individual cells respond to pathogens. In contrast, single-cell omics allows researchers to dissect the heterogeneity inherent in infected tissues, revealing subpopulations of immune cells, identifying rare infected cells, and characterizing the dynamic interplay between host and pathogen.
By integrating genomics, transcriptomics, proteomics, and other high-dimensional data modalities at the single-cell level, scientists can chart the course of infection with exquisite detail—yielding insights that inform diagnostics, therapeutics, and public health strategies.
Principles of Single-Cell Omics
Single-cell omics encompasses a suite of technologies that profile one cell at a time rather than in bulk. The workflow typically begins with tissue dissociation or microfluidic isolation of individual cells, followed by amplification of nucleic acids or labeling of proteins with barcoded reagents.
For transcriptomic analyses, single-cell RNA sequencing (scRNA-seq) captures messenger RNA transcripts within each cell, yielding gene expression profiles that distinguish cell types, activation states, and differentiation trajectories. Emerging modalities such as single-cell ATAC-seq map chromatin accessibility to infer regulatory landscapes, while single-cell proteomics—leveraging mass cytometry or novel bioorthogonal labeling approaches—quantifies protein abundance and post-translational modifications. Together, these layers of information form a comprehensive picture of cellular function and state.
Applications in Pathogen Discovery and Surveillance
Discovering and surveilling novel pathogens demands sensitivity to detect rare infected cells amid complex host tissues. During an outbreak of an emerging virus, for example, only a small fraction of respiratory epithelial cells may harbor replicating virions at a given time point. Single-cell transcriptomics can identify cells actively expressing viral transcripts, illuminating the anatomical niches where a pathogen first establishes infection. In a study of influenza A virus infection, researchers used scRNA-seq to reveal that only a subset of alveolar epithelial cells expresses high levels of viral genes, while neighboring cells mount antiviral responses despite lacking viral RNA. This level of resolution is critical for refining diagnostics: if only 5 percent of cells in a nasal swab exhibit detectable viral RNA, bulk assays may underestimate viral load or yield false negatives. Similarly, single-cell profiling of blood samples during outbreaks—such as during Ebola virus surveillance—has enabled identification of circulating monocytes or dendritic cells that respond to infection before clinical symptoms manifest. By pairing these insights with multiplexed serological assays, public health teams can track asymptomatic carriers and anticipate transmission hotspots, enhancing epidemic preparedness.
Investigating Host-Pathogen Interactions
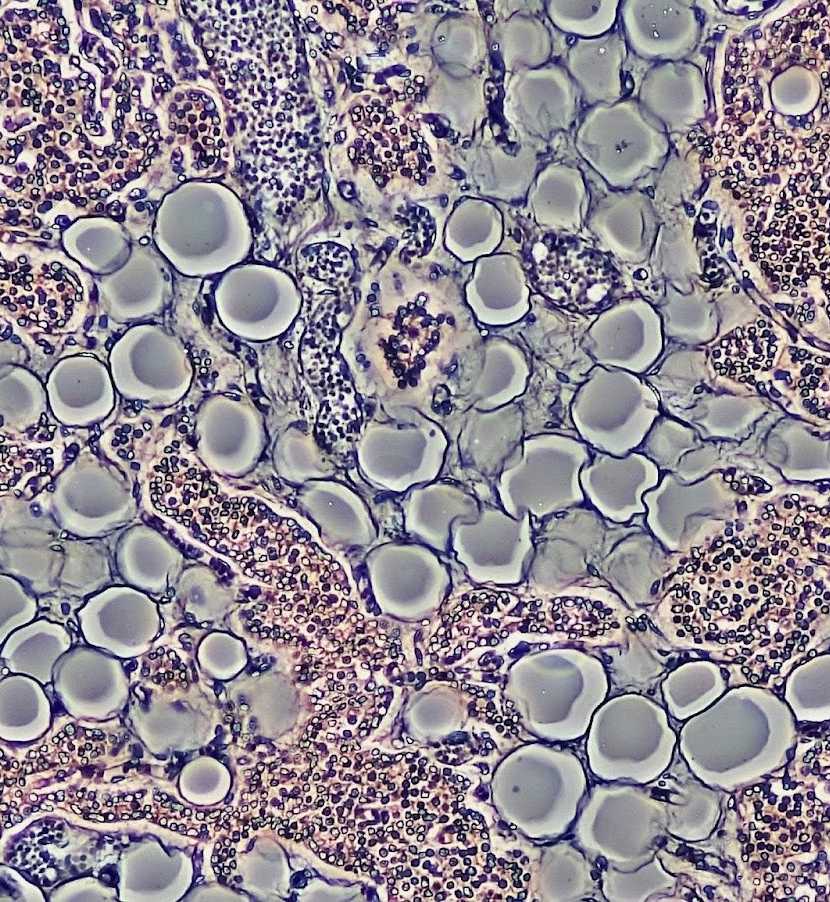
Infectious diseases rely on interactions between pathogen and host cells, and single-cell omics has proved essential in unfurling them at scale. Researchers studying tuberculosis have utilized scRNA-seq to analyze lung granulomas from individuals infected with Mycobacterium tuberculosis and discovered heterogenous populations of macrophages - some that support continued infection while others mount antimicrobial responses - among which were many that mounted effective defenses against further spread. Dual RNA-Seq technology enables scientists to explore host and bacterial transcripts within individual cells simultaneously (dual-RNA-seq), providing the opportunity to correlate host defense gene expression with intracellular bacterial gene regulation and thus identify pathways which support dormancy or promote activation. This complex approach has led to the identification of several macrophage subtypes with high expression of nitric oxide synthase and thus exhibit bactericidal activity, while others upregulate genes associated with lipoid droplet formation which provide essential nutrition for Mycobacterium growth.
Single-cell immunoprofiling of blood samples during acute viral infections such as dengue fever or SARS-CoV-2 infection has provided insight into T cell clonotypes and B cell repertoires associated with protective immunity. Single-cell TCR sequencing coupled with single-cell RNA-seq has provided further detail into this phenomenon, showing which antigen-specific T cells expanded more significantly among those who developed mild disease than severe illness; such information can provide vital clues towards developing more rational vaccine designs as well as uncovering correlates of protection.
Impact on Therapeutic Development and Customized Medicine
High-resolution profiling at the single-cell level accelerates development of targeted therapies and allows for the creation of tailored treatment regimens. Antiviral drug efficacy may vary dramatically based on host cell state and their intrinsic antiviral defenses; single-cell proteomic assays have revealed that some subpopulations of hepatocytes display baseline expression of interferon-stimulated genes even before being exposed to Hepatitis C virus infection; these "pre-activated" cells were found to resist viral entry and replication more effectively than their neighbors.
By testing potential drug candidates against different cellular states, researchers can more accurately anticipate which compounds will work well across diverse tissues while simultaneously eliminating those which only inhibit viral replication in some cells. Single-cell transcriptomics has revealed immunosuppressant monocyte subsets driving poor outcomes of sepsis patients; after which monoclonal antibodies targeting surface markers of these monocytes restored immune balance in ex vivo assays. Future clinicians could perform single-cell profiling on patient biopsies to assess which antimicrobial or immunomodulatory therapies may provide the greatest potential benefits, ushering in an era of precision infectious diseases care.
Challenges and Future Directions
Single-cell omics holds great promise in infectious disease research; however, its implementation poses several obstacles. Cell viability may be compromised during tissue dissociation procedures when dissecting fragile or necrotic infected tissues, leading to biased sampling. Enhancement strategies--such as gentle microfluidic sorting or fixation protocols designed to maintain RNA integrity--are being devised in order to mitigate these issues. Second, single-cell experiments remain limited by their high cost and computational complexity, particularly in settings with limited resources where emerging infections often surface. Advancements such as microfluidic droplet systems and barcoded bead technologies are helping reduce per-cell costs; however, data processing pipelines remain computationally intensive.
In response, open-source bioinformatics workflows are being optimized for cloud deployment in order to increase access to advanced analytics. Integrating multiomic layers, such as single-cell epigenomics with transcriptomics, poses complex analytical challenges in terms of data alignment, normalization, and interpretation. Researchers are taking on this problem through machine learning approaches that can detect regulatory networks even from sparse multimodal data sets. Building comprehensive reference atlases of infected tissues requires large-scale collaborative efforts like those seen in the Human Cell Atlas project, since only by gathering data from multiple populations and geographic regions can we fully grasp how host genetics, microbiome composition and environmental influences shape infection outcomes.
Conclusion
Single-cell omics has transformed infectious disease research in many ways, providing us with an unprecedented view into pathogengenesis, immunity and treatment strategies. By resolving heterogeneity within infected tissues, these technologies reveal the intricate host-pathogen dialogues that define disease progression trajectories. Single-cell approaches provide invaluable insight into every stage of infectious disease management: surveillance, diagnostics, therapy and prevention. While single-cell omics faces challenges such as standardizing workflows, reducing costs and scaling computational infrastructure; ongoing innovations may expand its use into clinical practice and global health initiatives.

Comments (0)