Microcytic hypochromic anemia
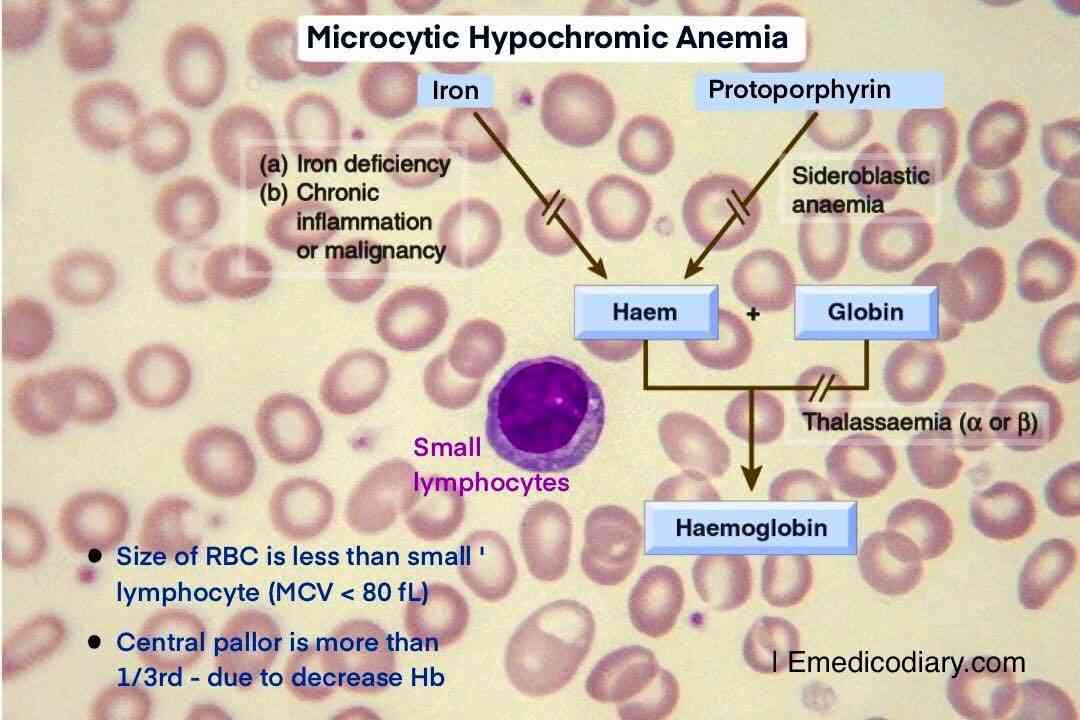
Microcytic hypochromic anemia is a type of anemia characterized by a decrease in the size of RBCs (with MCV < 80 fL) and an increase in central pallor due to a decrease in hemoglobin content. This condition is often caused by an inadequate supply of iron to the developing red blood cells or a defect in the production of hemoglobin. The differential diagnosis of microcytic hypochromic anemia includes Iron deficiency anemia, Thalassemia, Anemia of chronic disease, Sideroblastic anemia, and Lead poisoning.
Microcytic Hypochromic Anemia causes
- Iron deficiency Anemia
- Thalassemia
- Sideroblastic Anemia
- Anemia of Chronic Disease
- Lead Poisoning
Morphological Classification of Anemia
Based on Red blood cell Indices, morphologically, anemia can be classified as microcytic hypochromic anemia, normocytic normochromic anemia & macrocytic anemia.
1. Microcytic Hypochromic anemia is characterized by small RBCs (microcytes) with a mean corpuscular volume (MCV) less than 80 femtoliters (fL). Examples of microcytic hypochromic anemia include iron deficiency anemia, thalassemia, and anemia of chronic disease.
2. Normocytic Normochromic anemia is characterized by normal-sized RCSs with an MCV between 80 and 100 fL. Examples of normocytic normochromic anemia include anemia of chronic disease, aplastic anemia, and hemolytic anemia, blood loss.
3. Macrocytic anemia is characterized by large RBCs (macrocytes) with an MCV greater than 100 fL. Examples of macrocytic anemia include vitamin B12 deficiency anemia and folate deficiency anemia.
Here, in this article, we mainly focused on details of microcytic hypochromic anemia.
Causes of Microcytic Hypochromic Anemia
Microcytic hypochromic anemia occurs due to impaired hemoglobin synthesis, either due to a defect in heme synthesis or due to a defect in globin chain synthesis. This includes lack of iron in Iron Deficiency Anemia, or lack of iron release from macrophages to serum in Anemia of chronic disease, or failure of protoporphyrin synthesis in Sideroblastic anemia, or failure of globin chain synthesis in Thalassaemia. Lead aslo inhibits heme & globin synthesis.
A. Defect in heme synthesis
- Iron Deficiency Anemia
- Anemia of Chronic Disease
- Sideroblastic Anemia
- Lead Poisoning
B. Defect in globin chain synthesis
- Thalassemia
Causes of microcytic hypochromic anemia can be remembered as TAILS or SITA.
Symptoms of Microcytic Hypochromic Anemia
Common symptoms of anemia are
- Fatigue
- Tiredness
- Palpitation
- Effort dyspnea
- Effort intolerance
Less common symptoms of anemia are
- Faintness
- Pounding in the ear
- Efoort angina
Signs of Microcytic Hypochromic Anemia
Common symptom of Microcytic hypochromic anemia is Pallor, less commonly High cardiac output, Congestive cardiac failure. Others signs are mentioned specifically below according to conditions.
Clinical Feature of Iron Deficiency Anemia
- Atropic glossitis
- Angular cheilosis
- Dysphagia
- Koilonychia (Spoon nail)
Clinical Feature of Thalassemia
- Anemia
- Jaundice
- Hepatosplenomegaly as a result of extramedullary hemopoiesis
- Thalassemic face (Chipmunk facies) due to bone marrow hyperplasia
- Thining of the cotrex of many bones with tendency to fractures
- Bossing of skull with Hair-on-end appearance on X ray.
- Repeated blood transfuion lead to iron overload
Clinical features of Lead Poisoning
- Abdominal pain (lead colic)
- Constipation
- Lead line (Blue pigment between gum tooth line)
- Nephropathy, Neuropathy
Iron Deficiency Anemia
Iron deficiency anemia is the most common cause of microcytic hypochromic anemia. It occurs due to decrease in body's iron stores, and there is insufficient iron available for the production of hemoglobin. The iron profile of iron deficiency anemia shows a decrease in serum iron, ferritin, and percent saturation of iron binding protein, and an increase in total iron-binding capacity (TIBC).
Causes of Iron Deficiency Anemia
Iron Deficiency Anemia develops when the supply of iron is insufficient for the requirement of hemoglobin synthesis. This can be occured as
A. Increased Physiological Demand
- Children during period of growth
- Women during Menstruation, Pregnancy, Parturition, Lactation
B. Inadeuate Iron Suppy
- Nutritional deficiency
- Gastrectomy
- Tropical sprue
- Coeliac disease
C. Pathological Blood Loss
- Hookworm infestation (Ancylostoma duodenale)
- Bleeding peptic ulcer
- Carcinoma ofd stomach, colon
- Hemorrhoids (Piles)
- Ulcerative colitis
- Menorrhagia in female
Plummer-Vinson Syndrome
Plummer-Vinson Syndrome occur in severe severe iron deficiency anemia characterized by chronic iron deficiency anemia, koilonychia and dsyphagia (esophageal webs)
Thalassemia
Thalassemia is a group of genetic disorders characterized by a defect in the production of hemoglobin. There are two types of thalassemia: alpha and beta-thalassemia. Beta thalassemia is the most common type, and it is caused by a defect in the beta-globin gene. Hemoglobin electrophoresis is used to diagnose thalassemia, and it shows a decrease in HbA and an increase in HbA2 in beta-thalassemia major. In beta-thalassemia minor, there is a slight increase in HbA2.
Anemia of chronic disease
Anemia of chronic disease is a type of anemia that occurs in people with chronic infections, inflammatory diseases, or cancer. The iron profile of anemia of chronic disease shows a decrease in serum iron and percent saturation and an increase in ferritin. The increase in ferritin is due to the body's adaptation to store iron within cells to prevent pathogens from using the circulating iron. TIBC may be decreased in anemia of chronic disease due to the increase in ferritin levels, which signals the liver to decrease the release of transferrin.
Sideroblastic anemia
Sideroblastic anemia is a rare type of anemia characterized by the inability of the bone marrow to use iron to produce hemoglobin. The iron profile of sideroblastic anemia shows an increase in serum iron, ferritin, and percent saturation and a decrease in TIBC. The diagnosis of sideroblastic anemia is confirmed by a bone marrow examination, which shows the presence of ring sideroblasts. In ring sideroblasts, iron appears as a ring around the nucleus of normoblasts when stained with Prussian blue or Perl's stain.
Lead poisoning
Lead poisoning can also cause microcytic hypochromic anemia. Lead interferes with the production of hemoglobin, and it also damages red blood cells. The diagnosis of lead poisoning is confirmed by a blood lead level test.
Differential diagnosis of microcytic hypochromic anemia
A. Iron Profile
|
Iron profile
|
Iron Deficiency Anemia
|
Thalassemia
|
Anemia of Chronic Disease
|
Sideroblastic Anemia
|
|
Iron
|
Decreased
|
Normal
|
Decreased
|
Increased
|
|
Ferritin
|
Decreased
|
Normal
|
Increased
|
Increased
|
|
% Saturation
|
Decreased
|
Normal
|
Normal
|
Increased
|
|
TIBC
|
Increased
|
Normal
|
Decreased
|
Decreased
|
Note:
- Serum iron measures the circulating Iron level.
- Serum ferritin measures the amount of storage iron.
- % Saturation of iron-binding protein or Transferrin saturation measures amount of transferrin bound to iron. It is the ratio of serum iron to TIBC.
- Total Iron Binding Capacity (TIBC) measures the amount of transferrin in serum. It is the indirect measurement of transferrin (Transport protein of iron).
Serum ferritin is raised in Anemia of Chronic Diseases because pathogens use circulating iron to survive. So, the body adapts a system in which iron is stored within the cells of the body and prevents pathogens from using the circulating iron.
TIBC can be decreased in Anemia of Chronic Disease because an increase in ferritin level, can signal the Liver to decrease the release of transferrin.
B. Hemoglobin Electrophoresis: Hemoglobin Electrophoresis is done for Thalassemia
|
Hb Electrophoresis
|
Hb A
|
HbA2
|
HbF
|
|
Normal level
|
97%
|
1.5 – 3.2%
|
< 1%
|
|
β Thalassemia Major
|
Heavily Decreased
|
Slightly increased
|
10 – 90%
|
|
β Thalassemia Minor
|
Slightly decreased
|
Slightly increased
|
|
- In Sickle cell anemia (75-95%) HbS, along with the present of HbA2 and HbF. But no HbA.
- In β Thalassemia Major HbF ↑ (10-90%), slight increase in HbA2, very low HbA.
- In β Thalassemia Minor, slight increase in HbA2.
C. Bone Marrow Examination: Ring sideroblasts are present in sideroblastic anemia.
Iron appears as a ring around the nucleus of normoblasts. (Prussian blue reaction/Perl’s stain - Positive)
In conclusion, microcytic hypochromic anemia can be caused by various conditions, including iron deficiency anemia, thalassemia, anemia of chronic disease, sideroblastic anemia, and lead poisoning. The diagnosis of each condition requires a different approach, including the iron profile for iron deficiency anemia and anemia of chronic disease, hemoglobin electrophoresis for thalassemia, bone marrow examination for sideroblastic anemia, and blood lead level test for lead poisoning. Prompt and accurate diagnosis is crucial to ensure proper treatment and management of the underlying condition.

Comments (0)